CASE 128
History: A 47-year-old woman presents with dysphagia.
1. What should be included in the differential diagnosis of the imaging finding shown in the figure? (Choose all that apply.)
2. What is the most common surgical technique used for the management of esophageal carcinoma?
A. Bypass with colonic conduit
3. What is the most common intraoperative complication of esophagectomy?
C. Tracheobronchial tree injury
D. Recurrent laryngeal nerve injury
4. The most common nonmalignant reason for performing an esophagectomy in a pediatric patient is esophageal atresia. Which is the most common of the types of esophageal atresia (EA), often associated with a tracheoesophageal fistula (TEF)?
D. EA with proximal and distal TEF
ANSWERS
CASE 128
Esophagectomy with Small Bowel Transposition
1. A, B, D, and E
2. C
3. D
4. C
References
Kim TF, Lee KH, Kim YH, et al: Postoperative imaging of esophageal cancer: what chest radiologists need to know. Radiographics. 2007;27(2):409–429.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 39.
Comment
The surgical repair of esophageal resection can present the unsuspecting radiologist with some perplexing esophageal findings later in life when the patient undergoes an upper GI examination. Radiologists practice the specialty of radiologic imaging in the profession of medicine. It is crucial when possible to talk to the patient before any examination, to answer all questions or concerns, and to take a concise past and current medical history. Such an approach would greatly reduce the likelihood of the resident being startled by the findings.
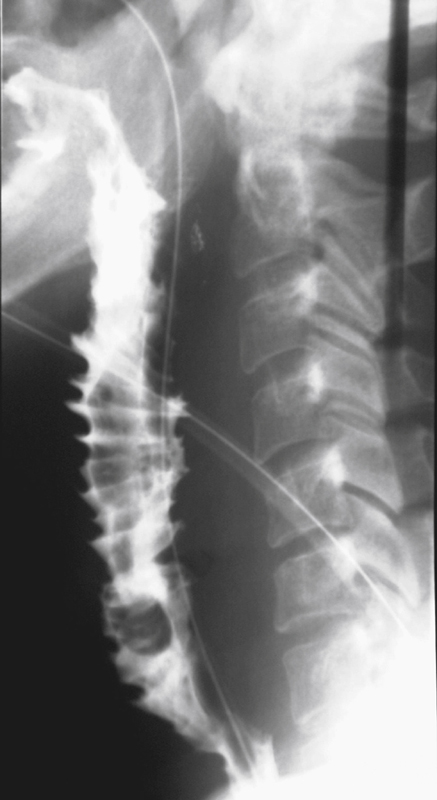
In this case, the patient had a pharyngoesophageal carcinoma that was treated with resection and jejunal interposition between the pharynx and the distal esophagus (see figure). In an attempt to maintain the continuity of the bowel, most of these surgeries today are done using colonic interposition. Such procedures may also be seen in patients who have fibrosis and marked generalized strictures of the esophagus. The haustral fold pattern of the interposed colon is retained to some extent and is usually easily recognizable. In the case of jejunal interposition, the normal jejunal pattern alters and is more difficult to recognize. The major long-term problem is gastric acid reflux, which is severe in almost 25% of these patients. A few cases (< 5%) develop a tracheoesophageal fistula. There is an increased risk of malignancy in patients whose interpositions were performed for malignancy. There has been some discussion in the literature about the risk of malignancy in interposition done for nonmalignant diseases; it seems to be minimal.







