CHAPTER 126
Joint Contractures
Guy Trudel, MD, MSc, FRCPC, DABPMR
Definition
A joint contracture is a limitation in the passive range of motion of a joint. Changes in articular structures (bone, cartilage, capsule) or nonarticular structures (muscles, tendons, skin) can prevent a joint from moving passively through its full range. A classification according to the tissue limiting the range of motion is proposed in Table 126.1.
Table 126.1
Classification of Contractures According to the Tissue Restricting the Range of Motion of the Joint
| Type | Condition* |
| Arthrogenic | |
| Bone | Intra-articular fracture, osteophyte |
| Cartilage | Osteochondritis dissecans |
| Synovium | Pigmented villonodular synovitis, synovial chondromatosis |
| Capsular | Secondary to immobility and capsular shortening, adhesive capsulitis, arthrofibrosis |
| Other | Meniscal tear, labrum tear, palmar or plantar fibromatosis |
| Myogenic | |
| Muscle | Muscle fibrosis, myositis ossificans, muscle adaptation to altered neurologic supply (spasticity, flaccidity) |
| Fascia | Eosinophilic fasciitis |
| Tendinous | Tendon transposition, shortening |
| Cutaneous | Burn, scleroderma |
| Mixed (any combination of the above types) | Burn and adhesive capsulitis |
* One or more clinical conditions illustrate each type of joint contracture.
By this definition, regardless of the nature of the tissue alteration, if it results in joint motion limitation, the joint condition is called a joint contracture. For example, a muscle with adaptive shortening or fibrosis restricting joint motion is classified as joint contracture—myogenic type. It should not be referred to as a muscle contracture.
As such, joint motion limited by pain or spasticity qualifies as a joint contracture only if the limitation is demonstrated after the pain or the influence of the hyperactive upper motor neuron (increased tone, spasticity, co-contraction) has been removed. For example, when a person with a spinal cord injury is treated for spasticity, the tone in the lower extremities will be reduced and an apparent chronic ankle plantar flexion contracture may disappear.
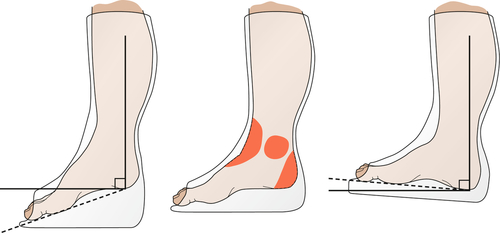
Conventionally, a joint contracture is named according to the joint involved and the direction opposite the lack of range. Some examples: a knee flexion contracture lacks full extension; an elbow extension contracture lacks full flexion; and an ankle plantar flexion contracture lacks dorsiflexion.
A contracture is the final common path of numerous conditions preventing movement of a joint through its full range of motion. Pain, trauma, immobility, weakness, and edema commonly contribute to reduced joint range of motion. The body’s natural reaction to a painful joint is to “splint” or immobilize it. Not moving the joint through its full range, with time, can cause structural changes to one or more articular or nonarticular tissues, and a joint contracture can ensue [1]. Joints traumatized by fracture or reconstructive surgery, such as anterior cruciate ligament repair or arthroplasty, are susceptible to contractures [2]. Joint contractures can happen as a consequence of the disease (prolonged immobility in bed in intensive care units; Fig. 126.1) or as part of the treatment (casting after fracture or prolonged use of a brace). Any joint can be affected. At the spine, affected vertebral amphiarthrodial and facet diarthrodial joints can limit the range at one or more segments.
Neurologic conditions that increase muscle tone or cause weakness contribute to contractures because of unequal forces generated by opposing muscle groups. In upper motor neuron conditions, such as after a stroke or traumatic brain injury, spasticity and excessive muscle tone prevent a joint from accessing portions of its normal range [3]. Similarly, in lower motor neuron injuries, such as a plexopathy or peripheral nerve injury, the unopposed muscle pull will limit joint motion toward the paralyzed muscle. The range of motion not accessed will eventually be lost, resulting in a joint contracture.
A number of other local conditions, such as arthritis, joint infections, and burns, will cause contractures [4]. In addition, conditions affecting multiple systems, such as muscular dystrophy, diabetes, and Parkinson and Alzheimer diseases, can limit mobility or initiation and put the patient at risk for contractures.
Data on incidence and prevalence of joint contractures are limited and often describe one specific joint [4]. Nevertheless, these studies indicate a common problem. At least one joint contracture was noted in 7% to 51% of persons after a spinal cord injury [5–7]. Between 16% and 81% of persons with an acquired brain injury developed a joint contracture [3,8,9], and 51% of children who had an obstetric brachial plexus injury were found to have a shoulder contracture [10]. In institutionalized elderly, one study reported that 71% of those who were immobile had a joint contracture, whereas none of the mobile patients had a joint contracture [11].
Symptoms
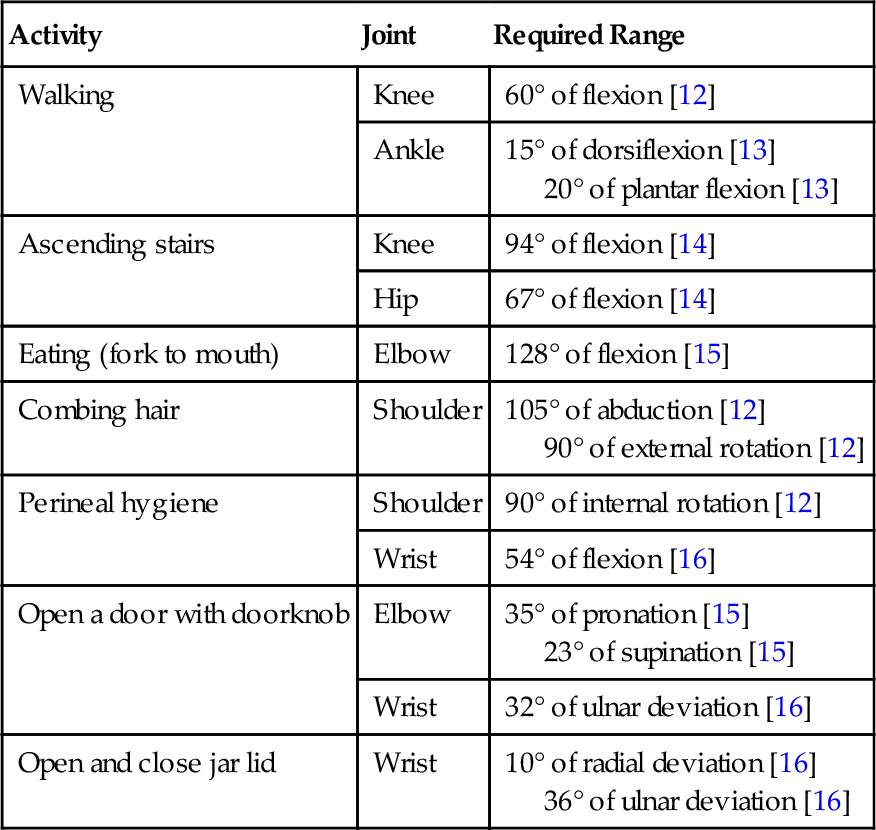
Joint contractures develop insidiously and may progress asymptomatically. They are painful only with attempts to move the joint through its full range beyond the restriction. Many daily activities do not require a joint to move through its entire range. Therefore a contracture may develop unnoticed for extended periods until the joint restriction interferes with functional activity (Table 126.2). In the outpatient setting, patients with hand and finger joint contractures might present with complaints of a weak or ineffective grasp. A patient with a knee flexion contracture may complain of a limp [17] or of hip or low back pain. Nearly half of tetraplegic spinal cord injury patients with a shoulder contracture experienced shoulder pain [18]. Subjects with spinal muscular atrophy or congenital myopathy were more than eight times more likely to experience elbow pain if they had an elbow contracture [19].
Table 126.2
Range of Motion Required to Perform Select Activities of Daily Living
| Activity | Joint | Required Range |
| Walking | Knee | 60° of flexion [12] |
| Ankle | 15° of dorsiflexion [13] 20° of plantar flexion [13] |
|
| Ascending stairs | Knee | 94° of flexion [14] |
| Hip | 67° of flexion [14] | |
| Eating (fork to mouth) | Elbow | 128° of flexion [15] |
| Combing hair | Shoulder | 105° of abduction [12] 90° of external rotation [12] |
| Perineal hygiene | Shoulder | 90° of internal rotation [12] |
| Wrist | 54° of flexion [16] | |
| Open a door with doorknob | Elbow | 35° of pronation [15] 23° of supination [15] |
| Wrist | 32° of ulnar deviation [16] | |
| Open and close jar lid | Wrist | 10° of radial deviation [16] 36° of ulnar deviation [16] |
Physical Examination
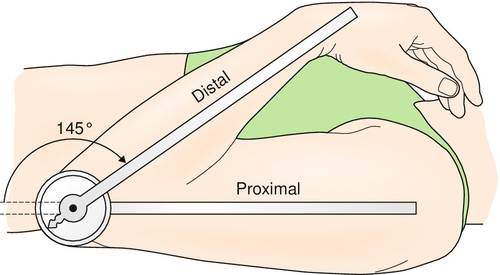
The patient must be relaxed, properly positioned, and in no pain. The clinician inspects the patient for abnormalities of limb shape, size, symmetry, and position. Edema, effusion, or deformity of the joints is noted. Skin is also assessed for any areas of breakdown or thickening complicating a contracture. Palpation of joints for swelling and tenderness must be completed. Passive range of motion is particularly important when weakness prevents normal active movement. The most precise tool for joint measurement is a universal goniometer (Fig. 126.2). Spine combined movements can be assessed with an inclinometer. Comparison is made with the contralateral side or with normative values [20].
A complete neuromuscular examination can detect potential causes of contractures. Particular attention must be paid to strength and specifically to the presence of muscle imbalance in opposing muscle groups. Reflexes and tone are assessed. In the presence of spasticity, the clinician should first apply prolonged passive stretch to determine whether a full range of motion can be achieved. If it is not achieved, the clinician can use modalities (e.g., therapeutic heating), optimize medication, or use motor block injections to rule out that spasticity is masking normal passive range of the joint. Finally, a sensory examination detecting abnormal sensation will influence the choice of treatment modalities.
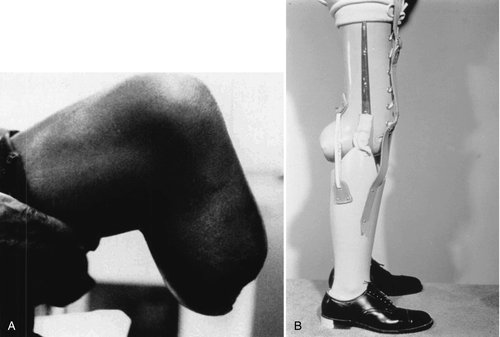
Functional Limitations
Joint contractures affect the performance of activities of daily living. Functional limitations depend on the underlying medical condition, the joints affected, and the severity of the joint contractures (Table 126.2). Upper extremity contractures of the elbow, wrist, and fingers impair the performance of all basic activities of daily living, such as dressing and grooming, as well as advanced skills requiring fine motor coordination, like writing. In a disabled elderly population, half as many subjects with an upper limb contracture fed themselves compared with those without a contracture [21]. Upper limb contractures can also limit mobility in patients using gait aids. Lower extremity contractures interfere mainly with mobility [21]. Hip and knee flexion contractures alter gait pattern, increase energy expenditure, and impair wheelchair mobility and car transfers. Fixed spinal deformity may limit many activities of daily living. Patients with transtibial amputations are at risk for development of a knee flexion contracture after their amputation (Fig. 126.3A). This may result in an inability to fit that patient with the most functional below-knee prosthesis. Instead, a bent-knee prosthesis, offering the patient less function and increased energy cost, must be used (Fig. 126.3B). Multiple upper and lower limb joint contractures exacerbate disability.
Diagnostic Studies
The diagnosis of a joint contracture is clinical. Radiographic evaluation can identify contributing conditions, such as osteophytes and heterotopic ossification. If a systemic cause is suspected, specific investigations are indicated.
Treatment
Initial
Successfully treating a medical condition that limits the joint range of motion may resolve the contracture; however, such conditions can also produce an irreversible joint contracture. A stepwise assessment and treatment plan may therefore be needed.
Prevention is at the heart of joint contracture management. Moving joints actively or passively through their full range on a daily basis prevents contractures. Continuous passive motion devices, such as those used after total knee joint arthroplasty, can achieve this postoperatively [22].
Pain control is essential to the prevention and treatment of contractures, particularly after an acute injury or after a surgical procedure [23]. Rest, ice, compression, elevation, and joint protection can help reduce pain in the acute stage, allowing earlier initiation of range of motion. Appropriate use of analgesics will promote the patient’s comfort and compliance with stretching sessions.
Therapeutic positioning and splinting prevent contractures in immobilized patients [23]. These measures maintain the correct length of connective tissue and alternate between different positions of the joint. An example of therapeutic positioning is lying prone to stretch the hip joints in extension. External rotation and abduction of the shoulders with an arm support attached to the bed of patients in the intensive care unit will maintain shoulder range. Standing upright or on an incline will help stretch the ankle joints. Hand and finger as well as ankle static orthoses are useful for preventing finger and ankle contractures.
Rehabilitation
Once contractures have developed, rehabilitation includes sustained stretching and exercises to increase range of motion. Again, analgesia and control of spasticity should be optimized to benefit the stretching sessions. A recent Cochrane review has questioned the effectiveness of up to 7 months of stretching in the treatment of contracture in both neurologic and non-neurologic conditions [24]; therefore, aggressive treatment may be required during a longer period.
Therapeutic modalities are commonly used to potentiate the effect of stretching sessions. The combination of modalities that heat soft tissues with stretching is an effective treatment [25]. Ultrasound, for example, heats soft tissues around large joints to a therapeutic temperature range of 40° C to 43° C, improving their elasticity [23]. Small joints can be heated by the use of paraffin bath dips or hydrotherapy (e.g., for hand and finger contractures in scleroderma or nerve injury).
Dynamic bracing can achieve prolonged, continuous stretching of joint contractures. Serial casting or serial splinting is also used with the same intent. After maximal stretching, a cast or orthosis is applied to preserve gains. The cast or orthosis is removed every 2 or 3 days, stretching is repeated, and the cast or orthosis is reapplied at an enhanced angle (Fig. 126.4). Joints casted or splinted at the end range of motion for longer periods led to improved benefit [26]. Serial casting or splinting should be carefully monitored on limbs with circulatory or sensory compromise because of increased risk of skin breakdown and ulcer formation.
Provision of assistive devices to lessen specific disability and of gait aids to try to normalize gait completes the rehabilitation process.
Procedures
If spasticity is thought to maintain contractures, despite optimized oral medication, treatments such as motor point blocks with phenol or botulinum toxin injections or intrathecal baclofen are considered. These procedures can be diagnostic as well as therapeutic because they can differentiate a joint contracture from spasticity. These procedures can constitute an adjunct to dynamic bracing and serial casting or splinting.
Extracorporeal shock wave lithotripsy [27] and ablative laser therapy [28] are being evaluated for skin-related contractures.
Surgery
In fixed contractures, surgical treatments include tenotomy, tendon lengthening, joint capsule release, and joint reconstruction. In some cases, skin grafts or flaps may be necessary to close resulting large skin defects [29]. These procedures are reserved for patients in whom less aggressive methods of treatment have failed and the fixed contractures significantly affect function [23].
Potential Disease Complications
Joint contracture can lead to ankylosis of a joint with corresponding loss of function. Upper limb contractures, especially if they are affecting multiple joints, can lead to dependency for all aspects of care. Mobility can be decreased to a bedridden state. Pressure sores can develop because of the limited options for mobility and weight-bearing areas. Infection by bacterial and fungal agents can occur in the skinfolds if contractures prevent adequate access for hygiene.
Potential Treatment Complications
Aggressive stretching can inadvertently result in pain; tears in muscle, ligament, or capsule; and joint subluxation. These complications can lead to bleeding, especially in patients receiving anticoagulation or those with a bleeding diathesis or thrombopenia.
Splinting and casting can result in skin ulceration or limb ischemia if patients are inappropriately selected or not closely monitored. This risk is increased if the patient lacks protective sensation because of the underlying disease.







