CASE 124


History: A patient presents with chest pain.
1. What are potential causes for the perfusion abnormality in Fig. D? (Choose all that apply.)
B. Tumor
D. Emphysema
2. What is the most likely diagnosis?
C. Tumor
D. Sarcoidosis
3. Which symptom or CT feature favors a pulmonary artery sarcoma over a pulmonary embolism?
A. Bilaterality
B. Expansion of the pulmonary artery
D. Unilateral lung hypoperfusion on ventilation/perfusion scan
4. What is the most common cause of a unilateral hilar mass?
A. Lung cancer
B. Sarcoidosis
ANSWERS
Reference
Yi CA, Lee KS, Choe YH, et al. Computed tomography in pulmonary artery sarcoma: distinguishing features from pulmonary embolic disease. J Comput Assist Tomogr. 2004;28(1):34–39.
Comment
Imaging
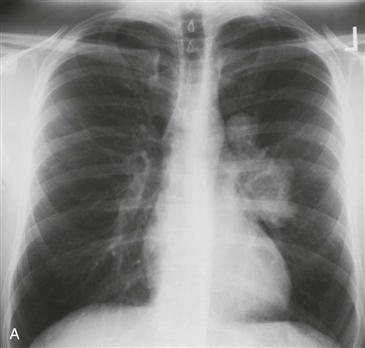
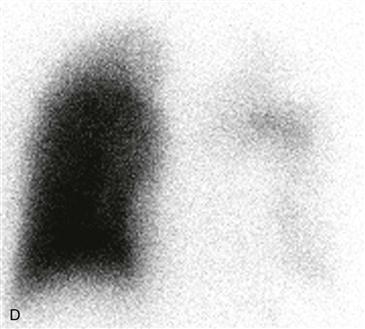
Chest radiograph and CT scan show lobulated filling defects within the main and left pulmonary arteries and a large left hilar mass (Figs. A–C). A corresponding perfusion image from a technetium-99m-labeled macroaggregated albumin study shows minimal left lung perfusion (Fig. D).
Differential Diagnosis
Pulmonary artery sarcoma is extremely rare, and prospective diagnosis is difficult. The main differential diagnosis is pulmonary embolism. Both conditions may manifest with dyspnea, cough, and chest pain. CT findings that are predictive of pulmonary artery sarcoma include a filling defect occupying the entire lumen of the main or proximal pulmonary arteries, expansion of the involved artery, or extraluminal extension of tumor (Figs. A–C). Other clues to the diagnosis include unilateral distribution and heterogeneous enhancement of the intraluminal filling defect (Fig. B). Prognosis of pulmonary artery sarcoma is poor with an average survival of 12 months after symptom onset.