CHAPTER 121
Burns
Jeffrey C. Schneider, MD; Amy X. Yin, MD
Definition
There are approximately 450,000 burn injuries requiring medical treatment and 45,000 burn hospitalizations, including 25,000 at burn centers, in the United States each year [1]. Adult burn injury patients are most likely to be young (average age at injury for adults is 42 years) and male (70%-75%) [1,2]. Most burns in adults result from fire or flame injuries (44%-61%) [1,2]. Other causes of burns that are also commonly reported include scald, contact, grease, electrical, and chemical injuries [1,2]. Burns usually happen in the home (68%) but also occur in the workplace (10%) or as a result of motor vehicle accidents (7%) [1]. For children, scald injuries are the most common cause and occur more frequently in children younger than 5 years. However, there are disproportionally more scald and inhalation injuries in minority populations [3].
Although there are 3500 estimated deaths from fire and burns annually in the United States [1], the incidence of burns has decreased dramatically in the past 50 years as a result of public education as well as home and work safety efforts. In addition, mortality from burn injury has declined by approximately 50% during the same period [4]. Advances in medical care and the development of comprehensive burn centers (Table 121.1) have contributed to this improved mortality rate. Survival of patients admitted to burn centers is estimated to be 96% [1]. Currently, once survival is ensured, medical management and treatment of burn injury are focused on wound healing, management of complications, and rehabilitation.
Symptoms
The symptoms of burn injury are directly related to the depth, size, and location of the injury. As expected, nociceptive pain is a major symptom of burn injury. Involvement of nerve endings in the dermal layer may also result in impaired or altered sensations causing neuropathic pain. Pruritus is common in the acute period and is linked to both the chronic inflammatory state and altered pain pathways of burns. Furthermore, postburn pain and pruritus may persist for years after injury, and regular monitoring with use of standardized measures is recommended. The visual analog scale, numeric pain rating scale, and 5-D scale for itching [5] are useful in assessing symptoms and treatment response.
Deep partial-thickness and full-thickness burns interrupt the function of skin appendages. Damaged skin appendages may include the apocrine sweat glands, resulting in dry, friable skin that does not heal well and is susceptible to infection. In larger burns, the loss of sweat glands may also impair body temperature regulation. The overall poor skin condition after burn injury may lead to chronic wounds.
Scar tissue develops weeks to months after closure of deep partial-thickness and full-thickness burns. Hypertrophic scars and contractures may result. This can be painful, cause deformity, and interfere with joint function. Contractures may lead to subluxation of hand or feet joints and dislocation of hips or shoulders. Scoliosis and kyphosis can result from burn scar contracture and postural changes.
Other symptoms are related to the multitude of other burn complications (see section on potential disease complications), some of which arise from the complex and prolonged intensive care and hospital course. Severe deep injury of extremities can require amputations of nonviable limbs. Formation of osteophytes and heterotopic ossification occur in burns and are associated with long-term immobilization [6]. Chronic infections from skin wounds and immune compromise are significant concerns. Other issues include complications from inhalation injury resulting in chronic pulmonary symptoms, hormone imbalances, deconditioning and malnutrition, and loss of bone and muscle mass [7]. Last, premorbid psychiatric disorders and psychiatric complications from the burn itself are prevalent and include sleep disturbances, depression, anxiety, substance abuse, and post-traumatic stress.
Physical Examination
A thorough physical examination is necessary to assess the burn itself as well as resulting complications. The evaluation should begin with an examination of the skin for burn location and depth, sensation, and signs of infection. Determination of burn depth allows categorization of wound severity.
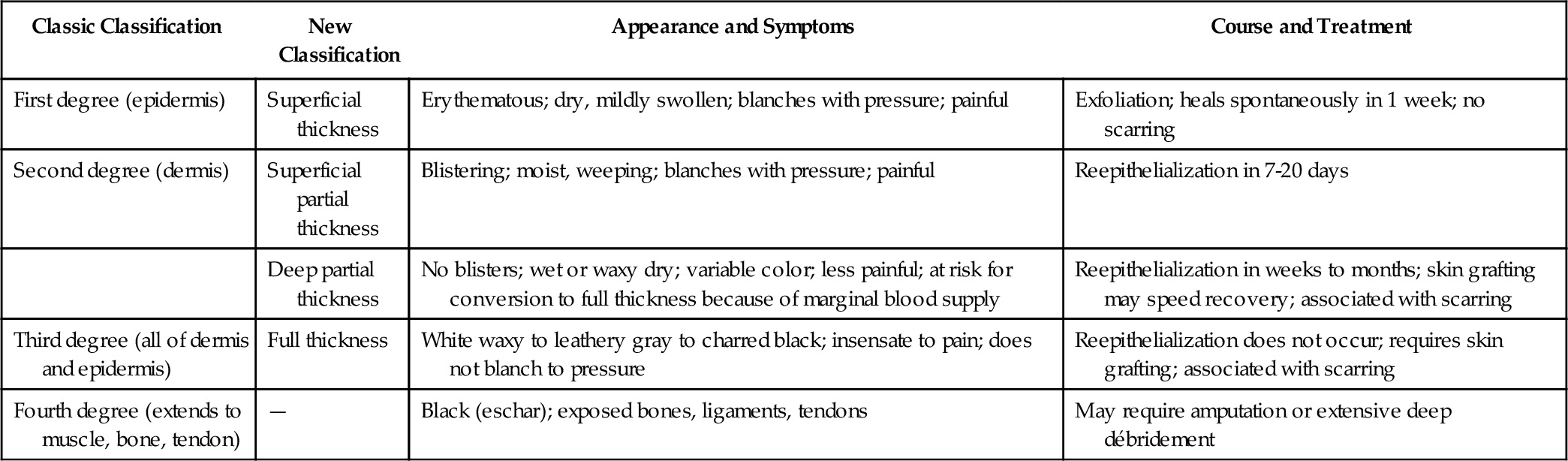
The current burn classification system groups burns into four categories of varying depth: superficial, superficial and deep partial thickness, and full thickness. Superficial injuries, traditionally known as first-degree burns, solely affect the epidermal layer. The category of second-degree burns is divided into superficial and deep partial-thickness burns. Superficial partial-thickness burns interrupt the epidermis and superficial (papillary) dermis. These often have good vascular supply and are painful with a pink or red and sometimes blistered appearance [8]. Deep partial-thickness burns extend into the deep (reticular) dermis and damage skin appendages, which affects some degree of sensory and apocrine function. Full-thickness burns, also called third-degree burns, affect the entire epidermal and dermal layers and result in complete loss of skin appendages. Deep partial-thickness and full-thickness burns usually have poor blood flow and can be painless and appear less red [8]. Severe injuries also may penetrate to the muscle, tendon, and bone. Such deep injuries, classified as fourth-degree burns, are not part of the newer anatomic classification system (Fig. 121.1 and Table 121.2).
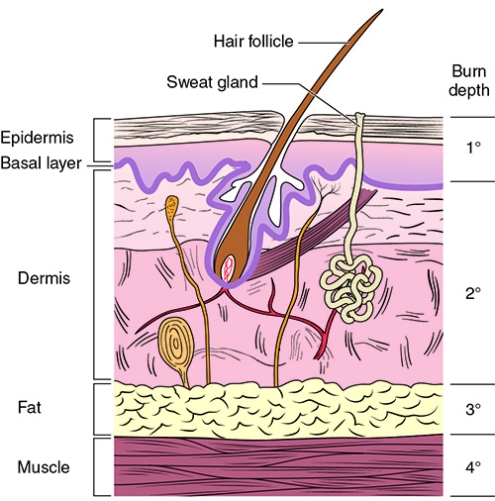
The depth of burn is an important factor in determining acute management of wounds. Burn surgeons often classify burns as superficial wounds, which heal by conservative management, or deep wounds, which require surgical intervention. Clinical assessment is the most widely used technique to evaluate burn wound depth and severity. Unfortunately, the clinical evaluation is accurate only about 64% to 76% of the time, and other techniques, briefly discussed in diagnostic studies, may also be used to evaluate wound depth [9,10]. Because of the evolving nature of burn wounds in the first few days after injury, monitoring the progression of the wound over time allows one to best assess its ultimate anatomic classification and management plan.
Postoperative burn wounds should also be closely watched in the rehabilitation setting. Postoperative wound evaluation includes inspection of grafts for hematoma, seroma, infections, and areas of graft loss [8]. After skin grafting, and as the skin matures, one should monitor for signs of hypertrophic scarring, which initially appears as erythematous, raised, and hardened skin.
A complete neurologic examination including an assessment of motor and sensory function, reflexes, and cognition should also be performed. Immediately after injury or surgery, the sensory examination is primarily limited to light touch modality because of pain. However, after wound closure, the sensory examination enables one to evaluate for small- and large-fiber neuropathies. Deep burn wounds may involve the vascular supply and affect wound healing. A pertinent vascular examination includes assessment of peripheral pulses of the involved extremities. The musculoskeletal examination should assess not only strength but also joint range of motion and deformities. The motor examination of joints crossed by a deep partial-thickness or full-thickness burn should not be performed until after skin graft “take” is ensured, usually within a week after grafting. Note that burn patients may have significant weakness from deconditioning and lean muscle loss. A complete cardiac and pulmonary examination should be performed with particular attention to signs of respiratory complications and hypermetabolic state. Psychiatric examination should include a thorough screening for signs of sleep disturbance, depression, anxiety, substance abuse, and post-traumatic stress. Patients who exhibit symptoms of a major psychiatric disorder should receive a complete psychiatric evaluation.
Functional Limitations
Functional limitations are directly related to the severity and location of the burn and related complications. Those with burns to the upper extremities may experience impairments in activities of daily living, fine motor tasks, and occupational activities. Burns to the lower extremities may result in impairments in mobility and higher level exercise and sport activities. Small burns to sensitive areas such as the face, including the eyes, ears, nose, or mouth, and genitals may result in significant impairments in specific functions.
Another effect is impaired psychological function. Psychological impairments are common and significant, leading to difficulty with community and social integration [11,12]. Factors associated with delayed return to work include increased hospital length of stay, electrical etiology, injury at work, and the need for inpatient rehabilitation. After hospitalization, barriers for returning to work include pain, neurologic issues, and impaired mobility [13].
Diagnostic Studies
Many different diagnostic tests are useful in the initial assessment of the burn patient. These may include tests to assess wound depth. The “gold standard” of burn depth analysis is biopsy with histologic assessment, but this is not standard practice [14]. Techniques using laser Doppler imaging, thermography, vital dyes, ultrasonography, and confocal laser scanning microscopes have been suggested for wound depth assessment, but these methods are not routinely used clinically. Bronchoscopic evaluation of the airway is performed for inhalation injury along with serum carboxyhemoglobin level.
In the rehabilitation setting, diagnostic tests are targeted toward short- and long-term sequelae of burns. Plain radiographs are used to evaluate for abnormal bone and joint changes, such as bone growth deformity in children, osteophytes, or joint subluxation and dislocation. Plain films are also used to evaluate heterotopic ossification but may not demonstrate findings until 3 weeks (see Chapter 130) [15]. Heterotopic ossification is diagnosed as early as 7 days after formation with a triple-phase bone scan. The aberrant ossification is visualized by increased uptake in the third phase of the scan. For patients with signs or symptoms of peripheral nerve injury, nerve conduction study and electromyography are used for the diagnosis of neuropathy.
Treatment
Initial
The initial management of the severely burned patient focuses on the ABCs: airway, breathing, and circulation. Aggressive fluid resuscitation to compensate for insensible fluid losses is a mainstay of acute management [16], but recent literature has shown overresuscitation to be a possible complicating issue [17]. Other principles of initial management include maintenance of clean and protected wounds, use of antimicrobial agents and infection prevention, emergent relief of ischemic compression by fasciotomy or escharotomy, and early excision and grafting of open wounds. A detailed review of the rapid advances in acute management of burn injuries is beyond the scope of this chapter.
Rehabilitation
Rehabilitation of burn patients is a complex issue. The most common and significant issues are discussed in this section.
Pain
Pain management after burn injury is an integral part of rehabilitation. Background nociceptive pain from the injury itself and exacerbations of pain from therapy, dressing changes, débridement, and other procedures can cause significant discomfort. Long-acting opioid pain medications are commonly used to treat background pain [18]. Premedication with short-acting opioid analgesics before dressing changes or procedures and for breakthrough pain is standard of care [18,19]. Because of the development of drug tolerance or a history of recreational opioid use, both common in burn patients, selection of opioids and doses has to be individualized to patients and may exceed standard dosing guidelines for appropriate symptom control. As the wounds heal, a slow and careful opioid taper is needed to prevent withdrawal. Although there is limited evidence for sole use of nonopioids in severe burn pain, nonsteroidal anti-inflammatory drugs and acetaminophen can be valuable in combination with opioids [18]. Other nonopioid pain medications, like muscle relaxants and antiepileptics, may also be used but have not been well studied.
Strong consideration should also be given to nonpharmacologic pain treatment options. Techniques that demonstrate reduction of pain scores include massage, hypnosis, multimodal distraction techniques, cognitive-behavioral techniques, and music therapy [18,20,21]. Off-the-shelf virtual reality has been shown to reduce acute pain intensity during wound care procedures [22].
Clinicians should note that pain is often a multifactorial experience and therefore should make extended efforts to treat all possible contributing factors, including pruritus, neuropathy, anxiety, sleep disturbance, depression, and post-traumatic stress.
Pruritus
Moisturizing is encouraged for treatment of pruritus; not only do emollients such as aloe vera and lanolin help improve skin quality, but massaging may provide itch relief by the gate theory and desensitization of the skin [23]. Studies have also shown that topical treatments with colloidal oatmeal, liquid paraffin, EMLA (eutectic mixture of local anesthetics) application, and doxepin cream can be effective for symptom management.
A mainstay of treatment is antihistamines. Histamine is found in abundance in burn wounds and is implicated as a primary mediator of pruritus. Selective H1 and H2 antihistamines are generally preferred to nonspecific antihistamines for their limited side effect profile. The use of cetirizine and cimetidine was also shown to be more effective than diphenhydramine and placebo in treatment of postburn pruritus [23]. However, the effect of any antihistamine is often limited. A study of 35 adult patients using diphenhydramine, hydroxyzine, and chlorpheniramine showed similar effect with complete relief in only 20%, partial relief in 60%, and no relief in 20% of patients [24].
Gabapentin has been shown in recent studies to relieve pruritus both as monotherapy and in combination with antihistamines. Some consider postburn pruritus to be a neuropathic process, and the effect of gabapentin may be due to the similar nerve pathways for pain and pruritus. A comparative study of gabapentin, cetirizine, and the combination of the two in 60 patients showed significantly better results in the gabapentin group and the combination group compared with the cetirizine-only group [25]. Pregabalin may be similarly effective but has not been studied in postburn pruritus. Other agents including ondansetron, paroxetine, and naltrexone have shown potential usefulness as adjunctive treatments.
Biofeedback therapy and psychological support may attenuate symptoms. Modalities including laser treatment, massage, and transcutaneous electrical nerve stimulation have also demonstrated positive results and may be useful [26–28]. The use of botulinum toxin injection is under investigation [29].
Wounds
The goal of wound care is to provide a moist, clean environment for reduced bacterial colonization and reepithelialization. Silver-based dressings are the cornerstone of wound management because silver ions have broad antimicroorganism activity. Silver sulfadiazine is the best known and most widely used silver-based agent for burns. More recent research suggests that new dressings that elute nanocrystalline silver have better antimicrobial activity, including against methicillin-resistant Staphylococcus aureus [30]. These dressings allow longer intervals between dressing changes and increase the patient’s comfort. Hydrofiber dressings are another new dressing type that may be less painful and are commonly used for exudative burns [31]. There has also been increasing interest in honey. Several trials comparing honey with traditional dressing in minor burns showed shorter healing times [30]. In general, there are many dressing options, and dressing selection should take into account knowledge and familiarity of the health care providers.
Hypertrophic Scarring
Compression garments are considered standard of care for treatment of hypertrophic scars. Such garments are initiated with closure of wounds. Initially, pressure wrappings are applied around the affected areas with plastic elastic (ACE), cotton elastic (Tubigrip), or adhesive elastic (Coban) bandages. As edema resolves, the scarred area assumes a more stable shape, and custom-made pressure garments are then fitted. These garments are usually recommended to be worn 23 hours per day for up to 1 to 2 years after a burn. Compliance with this schedule is difficult for many patients. The efficacy of this treatment has not been established in the literature [32], but a number of studies show some improvement in clinical appearance in moderate or severe scarring [33].
Silicone gel sheeting is also considered first-line treatment, but the use of silicone gel sheeting or silicone spray does not demonstrate greater effect compared with pressure garment use alone [34].
Contractures
Positioning and splinting are used to prevent development of contractures and to maximize joint function. Preventive treatment ideally begins on admission to the intensive care unit. The optimal position to minimize contracture development is depicted in Figure 121.2. Particular attention is given to burns that cross joints and exposed tendons. Such joints are at high risk for contracture development and should receive empirical splinting and exercises to maintain range of motion.
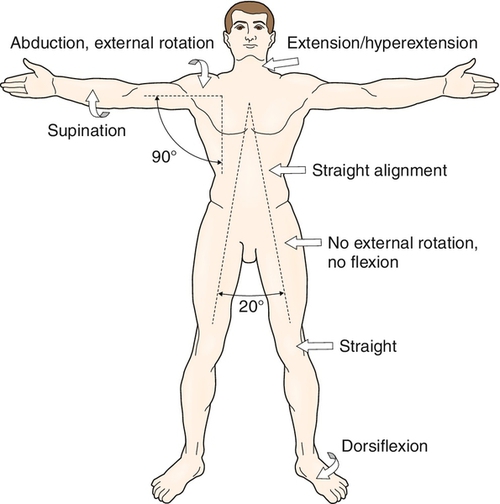
Positioning should always be paired with passive or active range of motion exercises to prevent the development of contractures. Range of motion exercises can begin immediately if the patient has not undergone skin grafting and usually within 1 week after grafting so as not to interfere with graft take. Once a contracture develops, rehabilitation interventions such as splinting, positioning, range of motion exercises, and serial casting have been shown to prevent worsening of the contracture and to improve joint motion [35–38].
Heterotopic Ossification (see Chapter 130)
Conservative treatments include positioning and range of motion exercises. Medications such as nonsteroidal anti-inflammatory drugs or bisphosphonates and radiation therapy are efficacious in the prevention of heterotopic ossification in other disease populations (e.g., spinal cord injury and hip arthroplasty). Their use can be considered, but studies have not examined their effect in burn patients [15].
Hypermetabolism and Deconditioning
After severe burns, survivors often experience a hypermetabolic state with increased catabolism and loss of lean body and bone mass. Meeting nutritional needs, often under the guidance of a dietitian, is an important part of burn care. Enteral feeding may be needed in the acute setting for effective nutrition. Consideration should also be given to nutritional supplementation including vitamins C and D, zinc, and thiamine. Oxandrolone, an anabolic steroid, has been shown in multiple randomized controlled trials, with up to 1 year of use, to increase muscle protein synthesis and weight gain and to decrease hospital length of stay [39]. Because of prolonged hospitalization and the loss of muscle, burn survivors are often severely deconditioned. Long-term exercise training programs are needed for return to premorbid functional level. Aerobic and progressive resistance training programs have been shown to be efficacious in improving strength, peak oxygen consumption, lean body mass, and pulmonary function in burn survivors [40].
Psychological Comorbidity
There is limited literature validating treatment of depression, acute stress disorder, post-traumatic stress disorder, and sleep disorders specifically in the burn population [41]. One small study suggests that sertraline may be useful in preventing post-traumatic stress disorder in burned children [42]. Regardless, a large body of evidence documents the efficacy of both pharmacologic and nonpharmacologic treatments of these disorders in other populations [43–45], and psychological conditions in burn patients should be addressed on the basis of these guidelines. Treatment of the burn-injured patient ideally involves collaboration with a mental health team to assist in the diagnosis and treatment of these problems.
Procedures
Botulinum toxin injection is under study as a treatment for postburn pruritus. Another procedure being evaluated is extracorporeal shock wave therapy, which may promote perfusion, increase angiogenesis, and accelerate burn wound healing [46]. Extracorporeal shock wave therapy may also have a role in improving pliability and appearance of postburn scarring [47]. However, both these procedures are investigational at this time.
Surgery
Excision and grafting of open wounds are ideally performed within 1 week of injury in clinically stable patients. The goal is to remove necrotic and inflamed tissue for promotion of physiologic wound closure. Studies have shown that early excision and grafting minimizes fluid loss, reduces metabolic demand, and decreases the risk of infection and sepsis [48].
There are many techniques for grafting. Most commonly, partial-thickness burns are treated with split- and full-thickness grafts of epidermis and superficial (papillary) dermis harvested from a nonaffected area (autograft). For larger wounds, mesh grafts or tissue expanders may be used [8]. Allograft, dermal substitutes, cultured epithelial autograft, and Meek technique for micrografts can be used for extensive burns with minimal viable tissue. Deeper burns may require excision and coverage with skin, muscle, or myocutaneous flaps, but these may lead to great deformity [8].
Bone marrow mesenchymal stem cells are under investigation for the possible regeneration of sweat gland–like structures. A few centers have performed face transplants for severe burn patients [49].
In spite of aggressive rehabilitation after a burn injury, significant contractures may still develop. Surgical release of the contracted joint is indicated when there are significant functional impairments despite appropriate conservative treatment.
Surgical resection of heterotopic bone is indicated if it results in significant joint impairment despite a course of conservative treatment or nerve entrapment.
Scarring, disfigurement, and other cosmetic concerns are addressed with reconstructive surgical efforts. Severely burned patients may undergo multiple surgeries during the span of years after their injury. Planning of the myriad possible procedures is a task that should involve multiple members of the burn team, including the patient and his or her family, physiatrist, surgeon, therapists, and mental health professionals.
Potential Disease Complications
Long-term Pain and Pruritus
Pain and pruritus after burn injury are difficult to manage and may become chronic and include physical impairments. Hypersensitivity can be a chronic consequence of burn injury regardless of the severity of the burn [50]. Patients with long-term severe pain and depression are associated with lower physical function at 2 years after injury [51]. This should be taken into account for rehabilitation, return to work, and community integration.
Hypertrophic Scarring
Hypertrophic scarring is common (32%-67%) among those severely burned and is more prevalent among darker pigmented individuals [52]. When it crosses a joint, it may result in deformities and contractures, leading to psychological, functional, and cosmetic impact [15].
Contractures
Contractures are a common and significant complication of burn injury. They result in cosmetic deformity as well as decreased joint range of motion and function. Contractures are most common at the shoulder, elbow, and knee. Length of stay, inhalation injury, and extent of burn are associated with increased incidence and severity of contracture [53]. Contractures of the hand most commonly occur at the wrist but may involve the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints of all digits. Predictors of hand contracture development include concomitant medical problems, total body surface area grafted, and presence of hand burn and hand grafting [54].
Amputation
Amputations may complicate burn injuries and are most commonly associated with electrical injury. Low-voltage (< 1000 V) injuries most commonly result in amputation of the digits. High-voltage injuries frequently result in major amputation (10%-50%).
Osteophytes and Heterotopic Ossification
Osteophytes are the most frequently observed skeletal alteration in adult burn patients and are most often seen at the elbow.
Heterotopic ossification occurs in approximately 1% of burn injuries and also is most frequently located at the elbow. It commonly is manifested with a decrease in range of motion and may cause impairments in joint function and activities of daily living.
Neuropathy
Mononeuropathies, mononeuropathy multiplex, and peripheral neuropathy have all been documented after burn injury. Risk factors for the development of mononeuropathy include electrical injury, intensive care, and history of alcohol abuse. Compression neuropathy can also result from bulky dressing and improper and prolonged positioning. Mononeuropathy multiplex and peripheral neuropathy in burn patients may be due to a combination of direct thermal injury and the body’s systemic response to injury. Risk factors for the development of a generalized peripheral neuropathy include intensive care stay, age, and diabetes [55].
Thermoregulation
Full-thickness burns damage the sweat glands present in the dermal layer. After skin grafting, these glands do not regenerate, leading to impaired sweating in involved areas. For those with larger burns, this may affect thermoregulation, particularly with physical activity in warm climates.
Psychological and Cognitive Complications
Psychological complications are some of the most significant sequelae of burn injury. Acute stress disorder, post-traumatic stress (11%-45%), depression (16%-53%), and sleep disturbances (13%-73%) are common after burn injuries. Preexisting psychiatric disorders are associated with longer hospital stays and require more surgical interventions. Burn patients, regardless of premorbid psychiatric history, often require long-term psychiatric follow-up.
Cognitive impairments may result from anoxia associated with inhalation injury or hypoperfusion associated with shock. A high index of suspicion is needed for diagnosis and treatment of patients with mild cognitive impairments. Neuropsychological evaluation may assist in diagnosis.
Potential Treatment Complications
Medications used to treat pruritus and pain have diverse side effects. The most common adverse effects of opioids and opioid-like pain medications are nausea, diarrhea, and constipation. Gastrointestinal, hepatic, and renal complications may arise from prolonged use of acetaminophen or nonsteroidal anti-inflammatory drugs. Antihistamines used for pruritus have sedating effects. The most common side effects of gabapentin and pregabalin are dizziness and somnolence. Topical treatments, such as silicone gel sheets for hypertrophic scarring, may result in skin maceration or contact dermatitis and rash. Splinting and casting for contractures may cause skin abrasions or pressure sores. Improper positioning and splinting may also lead to compression neuropathies, most commonly seen at the peroneal nerve. Surgical interventions always carry a risk of bleeding, infection, and poor wound healing. This is especially true for burn patients with immune compromise and poor skin integrity.