Procedure 12 Open Carpal Tunnel Release
![]() See Video 10: Open Carpal Tunnel Release
See Video 10: Open Carpal Tunnel Release
Indications
 Diagnosis of carpal tunnel syndrome with one of the following:
Diagnosis of carpal tunnel syndrome with one of the following:
Examination/Imaging
Clinical Examination
 Phalen test (Fig. 12-1): The patient’s wrist is held in a flexed position for up to 1 minute or until onset of symptoms. A positive test consists of the onset of numbness or paraesthesia in the median nerve distribution. Care must be taken to avoid direct pressure or flexion at the elbow when performing this examination, in order to avoid inducing ulnar nerve symptoms.
Phalen test (Fig. 12-1): The patient’s wrist is held in a flexed position for up to 1 minute or until onset of symptoms. A positive test consists of the onset of numbness or paraesthesia in the median nerve distribution. Care must be taken to avoid direct pressure or flexion at the elbow when performing this examination, in order to avoid inducing ulnar nerve symptoms.
 Carpal tunnel compression test (Fig. 12-2): The examiner applies direct pressure to the carpal tunnel with his or her thumb for up to 1 minute or until onset of symptoms. A positive test consists of the onset of numbness or paresthesia in the median nerve distribution. As with Phalen test, care is taken to avoid direct pressure or flexion at the elbow when performing this examination.
Carpal tunnel compression test (Fig. 12-2): The examiner applies direct pressure to the carpal tunnel with his or her thumb for up to 1 minute or until onset of symptoms. A positive test consists of the onset of numbness or paresthesia in the median nerve distribution. As with Phalen test, care is taken to avoid direct pressure or flexion at the elbow when performing this examination.
 Tinel sign (Fig. 12-3): The examiner taps directly over the carpal tunnel with his or her long and index fingers. A positive test consists of paresthesia or pain in a median nerve distribution.
Tinel sign (Fig. 12-3): The examiner taps directly over the carpal tunnel with his or her long and index fingers. A positive test consists of paresthesia or pain in a median nerve distribution.
 Two-point discrimination (tests innervation density; abnormal test is a late finding)
Two-point discrimination (tests innervation density; abnormal test is a late finding)
 Semmes-Weinstein monofilament test (tests pressure threshold; more sensitive)
Semmes-Weinstein monofilament test (tests pressure threshold; more sensitive)
Surgical Anatomy
 The superficial palmar fascia is a fanlike palmar fascial extension into which the palmaris longus inserts.
The superficial palmar fascia is a fanlike palmar fascial extension into which the palmaris longus inserts.
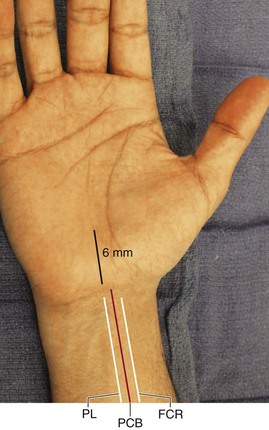
 The palmar cutaneous branch of the median nerve (PCN) lies between the flexor carpi radialis and palmaris longus tendons in the distal forearm, but its branches may be found up to 6 mm ulnar to the thenar crease in the palm (Fig. 12-4).
The palmar cutaneous branch of the median nerve (PCN) lies between the flexor carpi radialis and palmaris longus tendons in the distal forearm, but its branches may be found up to 6 mm ulnar to the thenar crease in the palm (Fig. 12-4).
 The transverse carpal ligament (flexor retinaculum) forms the roof of the carpal tunnel.
The transverse carpal ligament (flexor retinaculum) forms the roof of the carpal tunnel.
 The walls of the carpal tunnel are formed by the hamate and triquetrum ulnarly and the scaphoid and trapezium radially.
The walls of the carpal tunnel are formed by the hamate and triquetrum ulnarly and the scaphoid and trapezium radially.
 Nine tendons (four flexor digitorum profundus [FDP] tendons, four flexor digitorum superficialis [FDS] tendons, one flexor pollicis longus [FPL] tendon) travel within the carpal tunnel, along with the median nerve.
Nine tendons (four flexor digitorum profundus [FDP] tendons, four flexor digitorum superficialis [FDS] tendons, one flexor pollicis longus [FPL] tendon) travel within the carpal tunnel, along with the median nerve.
 The median nerve lies in the volar and radial quadrant of the carpal tunnel.
The median nerve lies in the volar and radial quadrant of the carpal tunnel.
 The recurrent motor branch typically arises from the volar-radial aspect of the median nerve at the distal end of the transverse carpal ligament and turns proximally and radially to innervate the thenar muscles. Multiple variations may exist, including a transligamentous course (recurrent motor branch pierces transverse carpal ligament), subligamentous origin, multiple recurrent motor branches, origin of recurrent motor branch from ulnar side of median nerve, recurrent motor branch anterior to transverse carpal ligament, absence of recurrent motor branch (ulnar nerve supplies thenar muscles), and others. Overall, the incidence of an anomalous course is 19%, with a transligamentous recurrent motor branch being the most common anomalous variation.
The recurrent motor branch typically arises from the volar-radial aspect of the median nerve at the distal end of the transverse carpal ligament and turns proximally and radially to innervate the thenar muscles. Multiple variations may exist, including a transligamentous course (recurrent motor branch pierces transverse carpal ligament), subligamentous origin, multiple recurrent motor branches, origin of recurrent motor branch from ulnar side of median nerve, recurrent motor branch anterior to transverse carpal ligament, absence of recurrent motor branch (ulnar nerve supplies thenar muscles), and others. Overall, the incidence of an anomalous course is 19%, with a transligamentous recurrent motor branch being the most common anomalous variation.
Exposures
 A 2.5- to 3-cm longitudinal incision is made in the proximal palm.
A 2.5- to 3-cm longitudinal incision is made in the proximal palm.
 The incision does not cross the distal wrist flexion crease.
The incision does not cross the distal wrist flexion crease.
 The incision should be placed 6 mm ulnar to the thenar crease (Fig. 12-5).
The incision should be placed 6 mm ulnar to the thenar crease (Fig. 12-5).
Procedure
Step 1
 The incision is made as described earlier (see Fig. 12-5).
The incision is made as described earlier (see Fig. 12-5).
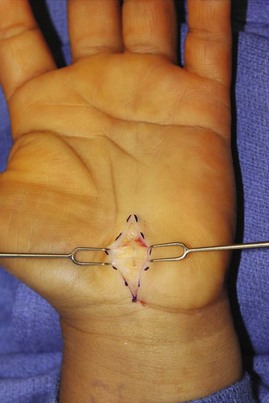
 Double skin hooks are used to retract the skin (Fig. 12-6).
Double skin hooks are used to retract the skin (Fig. 12-6).
 A no. 15 blade is used to incise down to the superficial palmar fascia, which has longitudinal fibers (Fig. 12-7).
A no. 15 blade is used to incise down to the superficial palmar fascia, which has longitudinal fibers (Fig. 12-7).
 A blunt self-retaining retractor is placed for radial and ulnar retraction, and blunt Senn retractors are used for distal and proximal retraction.
A blunt self-retaining retractor is placed for radial and ulnar retraction, and blunt Senn retractors are used for distal and proximal retraction.
Step 2
Step 3
Step 4
 Tenotomy scissors are used to spread distally, just superficial to the transverse carpal ligament.
Tenotomy scissors are used to spread distally, just superficial to the transverse carpal ligament.
 Under direct visualization, the distal release is completed with scissors (Fig. 12-10).
Under direct visualization, the distal release is completed with scissors (Fig. 12-10).
Step 4 Pearls
The presence of perivascular fat indicates proximity to the superficial palmar arch and the distal end of the release.
The surgeon’s small finger can be passed distally into the palm; if the release is complete, it should pass easily. Alternatively, the close end of the scissors can be inserted into the wound and, with a pullback motion, can define whether there is residual ligament that has not been divided.
Step 5
 Tenotomy scissors are used to spread on top of the ligament proximally.
Tenotomy scissors are used to spread on top of the ligament proximally.
 A freer elevator is placed under the ligament, and the contents of the carpal tunnel are pressed down and away from the ligament.
A freer elevator is placed under the ligament, and the contents of the carpal tunnel are pressed down and away from the ligament.
 The proximal release is completed under direct visualization with scissors (Fig. 12-11).
The proximal release is completed under direct visualization with scissors (Fig. 12-11).
Step 5 Pearls
Care is taken not to veer radially or ulnarly, to prevent injury to important structures (PCN and ulnar neurovascular bundle, respectively).
The surgeon’s small finger can be passed proximally into the distal forearm.
If tight bands are present, antebrachial fascia may be divided with scissors.
It is important to do this under direct visualization, as opposed to blindly advancing the scissors.
Synovectomy and neurolysis are not necessary unless specifically indicated (e.g., synovectomy in rheumatoid arthritis).
Postoperative Care and Expected Outcomes
 Elevation and finger motion are encouraged.
Elevation and finger motion are encouraged.
 Light activity is encouraged when comfortable.
Light activity is encouraged when comfortable.
 The dressing can be removed in 3 to 4 days, and handwashing is encouraged.
The dressing can be removed in 3 to 4 days, and handwashing is encouraged.
 Lifting is limited to 5 lb for 6 weeks.
Lifting is limited to 5 lb for 6 weeks.
 At 6 weeks the patient can gradually resume full activity.
At 6 weeks the patient can gradually resume full activity.
 With mild and/or intermittent symptoms, relief is often immediate.
With mild and/or intermittent symptoms, relief is often immediate.
 With prolonged or severe symptoms (two-point discrimination changes, thenar weakness), relief of symptoms may occur over many months, and the patient may not experience complete improvement.
With prolonged or severe symptoms (two-point discrimination changes, thenar weakness), relief of symptoms may occur over many months, and the patient may not experience complete improvement.
Freshwater MF, Arons MS. The effect of various adjuncts on the surgical treatment of carpal tunnel syndrome secondary to chronic tenosynovitis. Plast Reconstr Surg. 1978;61:93-96.
Keith MW, Masear V, Amadio P, et al. Treatment of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009;17:297-405.
Keith MW, Masear V, Chung K, et al. Diagnosis of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009;17:389-396.
Lanz U. Anatomical variations in the median nerve in the carpal tunnel. J Hand Surg [Am]. 1977;2:44-53.
Watchmaker GP, Weber D, Mackinnon SE. Avoidance of transaction of the palmar cutaneous branch of the median nerve in carpal tunnel release. J Hand Surg [Am]. 1996;21:644-650.