Antiinfective Medications
Objectives
1. Identify the major antiinfective drug categories and the organisms against which they are effective.
2. Outline the most important things to teach the patient who is taking antiinfective medications.
3. Define spectrum and explain what this word means in antiinfective therapy.
4. List some of the most common adverse reactions to medications used to treat infections.
Key Terms
antibiotics (ăn-tĭ-bī-ŎT-ĭks, p. 162)
antimicrobials (ăn-tĭ-mī-KRŌ-bē -ălz, p. 162)
bactericidal (băk-tēr-ĭ-SĪD-ăl, p. 162)
bacteriostatic (băk-tēr-ē-ō-STĂT-ĭk, p. 162)
broad-spectrum drugs (p. 162)
generation (JĚN-ěr-Ā-shun, p. 162)
helminthiasis (hěl-mĭn-THĪ-ă-sĭs, p. 181)
narrow-spectrum drugs (p. 162)
pathogen (PĂTH-ō-jěn, p. 161)
spectrum (p. 162)
superinfection (SŪ-pěr-ĭn-fěk-shŭn, p. 163)
Overview
![]() http://evolve.elsevier.com/Edmunds/LPN/
http://evolve.elsevier.com/Edmunds/LPN/
This chapter describes the main information about many types of antiinfective medications. It is divided into three sections: The first section discusses major bacterial antiinfective agents; the second section describes the drugs used in treating tuberculosis (TB). The third section discusses drugs used to treat parasitic infections: amebicides, anthelmintics, and antimalarial preparations. Antifungal medications are included in Chapter 13, along with other antiviral and antiretroviral drugs used in the treatment of acquired immune deficiency syndrome (AIDS).
Because of the many different types of infections and the numerous drugs that have been developed to treat them, antiinfective drugs are some of the most commonly given drugs. Thus nurses need to learn as much as possible about these drugs and what to teach patients who are taking them.
Organisms of many different types are always on the skin and inside the body of a healthy individual. These organisms do not make a person ill unless there is some alteration in the skin barrier or a change that makes the person at higher risk, such as being pregnant or having AIDS. Infants, young children, and older adults have the greatest risk of infection, as do people with poor circulation, poor nutritional status, or multiple diseases, and those who often come in contact with people who have infections.
An organism that causes infection is a pathogen. As a very basic summary of important definitions, pathogenic organisms that cause disease because of their ability to divide rapidly and overwhelm the immune system or produce toxins come in a variety of forms. Bacteria are a large domain of single-celled, prokaryote microorganisms. They have a wide range of shapes and characteristics. This is a generic term that is now often replaced by more specific names. A fungus is a member of a large group of eukaryotic organisms that include microorganisms, such as yeasts and molds; grow in irregular masses, without roots, stems, or leaves; and live and feed on other organisms. A virus is a small infectious agent that can replicate (reproduce itself) only inside the living cells of organisms. With few exceptions, viruses are capable of passing through fine filters that trap most bacteria. How a virus is classified depends on the features of its virion (or complete virus particle). The two main classes are ribonucleic acid (RNA) viruses and deoxyribonucleic acid (DNA) viruses. A parasite is an organism, protozoa, or worm that lives on or in another organism and draws its food from the other organism.
Each infection in a patient must be carefully evaluated to identify the specific organism causing the infection and the drug that will be most effective against it. Although some parasites may be seen with the naked eye, most infectious organisms are visible only under a microscope. Bacteria must be carefully cultured and tested to see which antimicrobials are effective against them (antimicrobial sensitivity). Nurses will often be asked to collect specimens for this type of testing. Bacteria can be identified by their shape. Learning what organism is present allows the health care provider to order the medication that will best treat that particular bacteria.
Antiinfective agents, or antimicrobials, are chemicals that kill or damage the pathogenic organisms. Antiinfective agents are classified by their chemical structures or by their mechanisms of action. Some of these chemicals are made from other living microorganisms (such as the penicillins), and are classified as antibiotics. Other chemicals are synthetics (such as sulfonamides) or combinations of synthetic and naturally occurring microorganisms. Some drugs have become more refined, purified, and sensitive as a result of long-term testing. Each new group of these drugs developed from other similar drugs is called a generation; the original drugs are referred to as first-generation drugs, and later groups are called second-generation drugs, third-generation drugs, and so on.
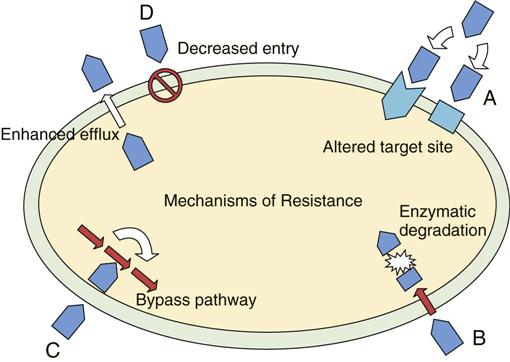
Antiinfective medications work in different ways to affect pathogenic bacteria (Figure 12-1). They may attack a bacterium’s internal cell processes, which are vital to its existence, or they may destroy the external cell wall, making it weaker or unable to reproduce; in some cases, they actually kill the organism. Agents that are bactericidal kill the bacteria; those that are bacteriostatic limit or slow the growth of the bacteria, weakening or eventually leading to the death of the bacteria. (The “cidal” or “static” part of the word gives a clue about the activity, whether it refers to bacteria or to fungi [fungicidal or fungistatic].) Bacteria are often classified as gram positive or gram negative, depending on whether they are stained by Gram stain. The number of organisms the medication is effective against is described in terms of its spectrum. Some antiinfective medications are effective against only a few gram positive or negative bacteria. These are called narrow-spectrum drugs. An example is a drug effective against only one type of pneumonia. Other drugs are effective against both gram negative and gram positive bacteria. These are known as broad-spectrum drugs. An example is Levofloxacin. A specimen must be cultured and the antibiotic that is most effective against that particular organism is then determined through sensitivity testing. The correct antibiotics must be given to destroy the pathogen and to limit the adverse effects for the patient.
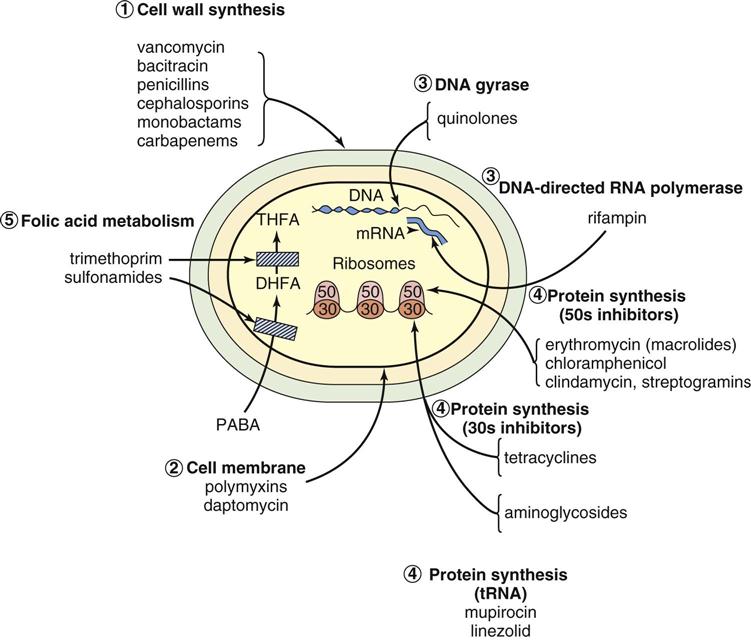
PABA, paraaminobenzoic acid; DHFA, dihydrofolic acid; THFA, tetrahydrofolic acid.
Antibiotics are not effective against viral, parasitic, or fungal infections and other antimicrobials are required. However, it is common for a patient with a viral or fungal infection to also develop a bacterial infection, because the body’s defenses are weakened. A secondary infection occurs when one infection follows another. In a mixed infection, both infections are present at the same time.
Antibiotics may cause adverse or negative reactions. These include:
• allergy (penicillin and sulfa products cause the most allergies);
• and gastrointestinal (GI) distress so severe that it may require stopping the drug.
Antibiotics can also result in superinfection, when other organisms that are not sensitive to a prescribed antibiotic (for example, yeast) are able to multiply, overgrow, and get out of control because the antibiotic also killed the normal bacterias that would have kept them under control. Pseudomembranous colitis is a condition now commonly seen in hospital and nursing homes that arise from superinfections caused by Clostridium difficile.When an antibiotic is given when the body’s natural immune system would have been effective, given for the wrong bacteria or for a virus for which it is ineffective, the pathogens are not destroyed and may become stronger. Overuse or unnecessary use of antibiotics has led to several current problems in using antibiotics: (1) patients expect and demand a prescription every time they feel ill; (2) the organisms that were weak may all have been killed over the years, leaving only the very virulent or strong pathogens; and (3) exposing organisms to antibiotics that did not kill them has led to the development of “super germs” that have built up a tolerance or resistance to common antibiotics. The result of these factors is that many common organisms infecting patients are now resistant to available drugs, and new antiinfectives have not yet been developed to fight them (Figure 12-2). Because many bacteria have developed resistance to multiple drugs, vancomycin may be a drug of last resort in many patients. Vancomycin is effective against some gram-positive bacteria that are resistant to multiple drugs and is used in cases of severe infection. Even now vancomycin has been found to be ineffective in some parts of the country for methicillin resistant streptococcus A (MRSA) infections. It is frightening to realize that there are common bacteria now for which we have no effective antibiotics. It may take several years before researchers are able to find new antiinfective drugs, and many patients may be left without effective drugs when they really do need them. One thing that can be done is to take special consideration to monitor antimicrobial use in children.
Antibiotics 
Penicillins
Action
Penicillins interfere with the creation and repair of the cell wall of the bacteria. They also bind or stick to specific enzymes that the bacteria needs so that the bacteria cannot use them. This process makes the bacterial cell weak and allows it to break down more easily (see figure 12-2).
Uses
Penicillins were first used on a wide scale in the 1940’s and were the main antibiotics for many years. Penicillin is the broad-spectrum drug of choice for susceptible gram-positive and gram-negative organisms. Penicillins are considered the safest antibiotics.
There are many penicillin products, including oral amoxicillin to injectable procaine penicillin. The choice of drug to give a patient depends on the infectious bacteria (as identified by cultures or smears) or on the basis of the clinical picture. Penicillin is effective in the treatment of the following susceptible organisms: alpha-hemolytic streptococci; group A beta-hemolytic streptococci; streptococci belonging to groups C, G, H, L, and M; and Spirillum minus (rat-bite fever), Treponema pallidum (syphilis), Clostridium perfringens, Clostridium tetani, Corynebacterium diphtheriae, Staphylococcus, Pasteurella meningitidis, and other less common organisms. Penicillin is also used for prophylactic (preventive) treatment against bacterial endocarditis in patients with rheumatic or congenital heart disease before they have dental procedures or surgery of the upper respiratory tract, genitourinary tract, or GI tract. Some penicillins may be useful against organisms used by terrorists as bioweapons.
As broad spectrum antibiotics, penicillin has been used for almost every type of infection, including those for which they were not effective. Over the years, overuse and inappropriate use of penicillin has led to the development of penicillin-resistant strains of disease. These penicillin-resistant strains of bacteria produce a chemical called penicillinase. β-lactamase (penicillinase) is an enzyme that disrupts the internal structure of penicillin and thus destroys the antimicrobial action of the drug. Although penicillin continues to be an important antibiotic, research on penicillin has led to the identification of many other types of antibiotics that may now be used to control infection.
Adverse Reactions
Adverse reactions to penicillin are many. Major reactions include neuropathy (nerve damage in a variety of places and seen with high parenteral dosages), fixed drug eruptions (usually a single spot that itches), nausea, vomiting, epigastric distress, anemia, and blood dyscrasias. Allergy to penicillin has also become a problem, producing rash, erythema (redness or inflammation), urticaria (hives), angioedema (swelling of the skin and mucous membranes), laryngeal edema (swelling of the larynx), and anaphylaxis (shock). These allergic reactions may occur suddenly or after the patient has been taking the medicine for some time and may be life threatening. They may occur up to 10% of the time in patients taking penicillin products.
Drug Interactions
Other bacteriostatic antibiotics such as tetracycline and erythromycin may decrease the bactericidal effect of penicillin. Probenecid prolongs blood levels of penicillin by blocking its renal clearance. Use of ampicillin and oral contraceptives together has produced menstrual irregularities and unplanned pregnancies because penicillin reduces the level of available hormone. Indomethacin, phenylbutazone, or aspirin may increase serum penicillin levels. Antacids may decrease the absorption of penicillin. Penicillin may change the results of some laboratory tests. For example, penicillin may cause increased bleeding time when the platelet count is normal, giving a false positive urine protein test and lupus erythematosus cell test.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
The patient in need of antibiotic therapy may vary from being asymptomatic (showing no symptoms) to being severely ill. Look for common clues to infection, such as fever, redness, swelling, or pain.
Ask whether there is a prior history of penicillin allergy, asthma, or hypersensitivity (allergy) to procaine or tartrazine, and find out if the patient is pregnant or breastfeeding. These conditions may be contraindications or precautions to the use of penicillin. Anaphylactic (shock) reactions have occurred with both oral and parenteral penicillin therapy. Penicillin should be used with caution in patients who have many other drug allergies.
With intramuscular (IM) injections, follow institutional policy about whether to aspirate (pull back on the plunger of the syringe to check for blood) to prevent medicine from accidentally being injected into a blood vessel.
Patients often spread infections to family or friends. For example, the sexual partners of patients infected with syphilis or gonorrhea must be treated also.
Penicillin changes the results of many laboratory tests, so while the patient is on penicillin therapy, the results of laboratory culture and sensitivity tests, as well as many other laboratory findings, may be incorrect.
The type and dosage of penicillin ordered depends on the pathogen and severity of the infection. Over the years, several different types of penicillin have been developed: natural penicillins (Penicillins G and V), penicillinase resistant drugs; broad-spectrum aminopenicillins; and other types of broad-spectrum drugs. Table 12-1 presents a summary of penicillins.
![]() Table 12-1
Table 12-1
| GENERIC NAME | TRADE NAME | COMMENTS |
| Natural Penicillins | ||
| penicillin G (benzathine) | Bicillin Permapen |
Long-acting IM penicillin. In children, administer parenterally in midlateral aspect of thigh. In adults, give IM in gluteal muscle. Oral dosage exhibits poor absorption and is not recommended for routine use. |
| penicillin G (potassium) | Pfizerpen | Given primarily to infants and children IV as 15-30 min infusions. |
| penicillin G (procaine, aqueous) (APPG) | Wycillin Bicillin-CR |
Contains procaine to decrease injection pain; determine if patient is allergic to procaine. Give deep IM injection in gluteal muscle; aspirate before injection; rotate injection sites. Drug of choice for gonorrhea. |
| penicillin V |
Stable in gastric juices; however, blood levels are higher when administered on an empty stomach. 125 mg, 250 mg, and 500 mg is equivalent to 200,000, 400,000, and 800,000 units, respectively. | |
| penicillin V potassium | Used in treatment of mild to moderately severe infections when patient can take oral medication. | |
| Penicillinase Resistant | ||
| cloxacillin | Effective in treatment of pneumococci; also effective in treatment of group A beta-hemolytic streptococci. | |
| dicloxacillin | Effective in treatment of penicillinase-producing staphylococci. | |
| nafcillin | ||
| oxacillin | Rare, reversible hepatocellular dysfunction has been reported. | |
| Aminopenicillins: Broad-Spectrum Penicillins | ||
| amoxicillin | Amoxil Moxilin Sumox Trimox |
|
| amoxicillin and clavulanate potassium | Augmentin | |
| ampicillin | Principen | |
| ampicillin sodium (parenteral) | Used in treatment of a variety of serious infections and often used concomitantly with a sodium aminoglycoside or a cephalosporin. | |
| ampicillin sodium and sulbactam sodium | Unasyn | Give either IV or IM. |
| bacampicillin | ||
| Extended Spectrum | ||
| Carbenicillin | Geocillin, Geopen | Available in both IV and IM form. |
| Mezlocillin | Mezlin | Available in IV form. |
| piperacillin | Effective against a wide number of gram-positive and gram-negative aerobic and anaerobic bacteria. | |
| piperacillin sodium and tazobactam sodium | Zosyn | Administer by IV infusion over 30 min. |
| ticarcillin | Ticar | Uncomplicated urinary tract infection. |
| ticarcillin and clavulanate sodium | Timentin | Reduced dosage required in patient with renal impairment. |
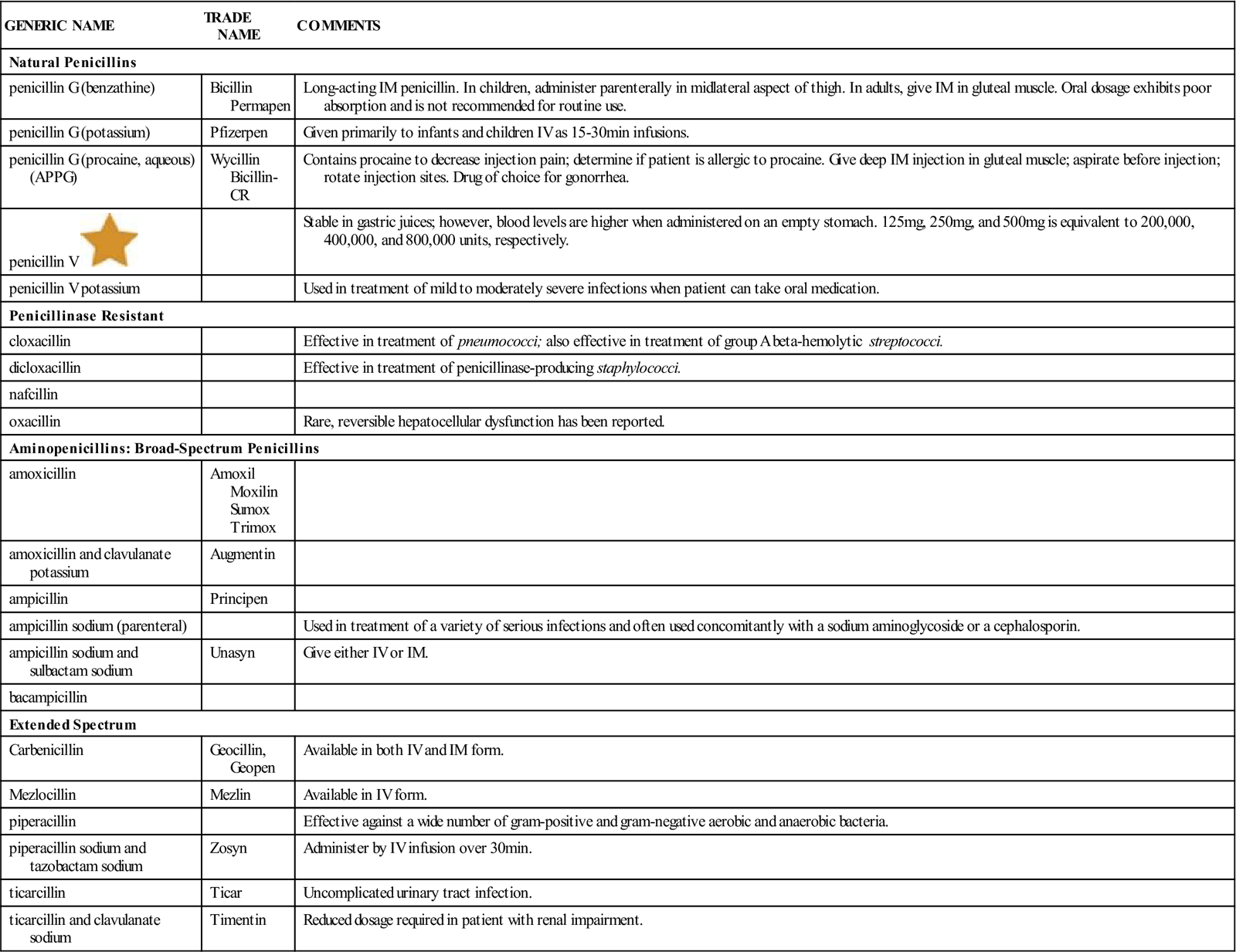
IM, Intramuscular; IV, intravenous.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Take the patient’s blood pressure and pulse before giving IM penicillin injections to have baseline information. The patient should be advised the first time they receive this medicine to wait 30 minutes after administration by mouth (PO) or IM administration before leaving an office or clinic. This allows time to watch for signs of adverse reactions. Also watch the patient for signs of allergic reaction, although some allergic responses may not develop for days after taking the medication.
Tetracyclines
Action
The tetracyclines are bacteriostatic agents. They act by interfering with the ability of the bacterial to make protein. Without this protein, the bacteria cannot stay alive.
Uses
The tetracyclines are important broad-spectrum drugs and they are effective against many gram-negative and gram-positive organisms (see Table 12-2 on p. 170). Many other drugs are more effective so that tetracyclines are the first choice drugs in only a few diseases, such as Lyme disease, stomach ulcers caused by Helicobacter pylori, Chlamydia, Rocky Mountain spotted fever, cholera, and typhus. Many adolescents use tetracycline-based products in the prevention or treatment of acne.
Adverse Reactions
The tetracyclines are relatively safe, with very few serious adverse effects. They commonly produce mild episodes of nausea, vomiting, and diarrhea that may require stopping the drug. These effects are often dose related, and they result from GI irritation, changes in the normal bacteria in the bowel, and overgrowth of yeast.
The use of tetracycline in pregnancy and in children younger than 8 years of age may produce permanent yellow-brown tooth discoloration or inadequate bone or tooth development.
Photosensitivity may occur with tetracycline treatment, so the patient should avoid exposure to the sun or ultraviolet rays. Pregnant women should not use tetracyclines because they are category D agents which may damage the fetus.
Tetracycline should be used with caution in patients with poor liver function, because the drug may cause hepatotoxicity.
Superinfections may develop, particularly after long-term use. These reactions, such as diarrhea, oral thrush (Candida infection of the mouth), or vaginal itching, are usually irritating but mild. At other times, the superinfection may become life threatening. Overgrowth of organisms is commonly seen in AIDS patients, whose immune systems may be totally overwhelmed by a mild superinfection.
Vertigo may develop with the use of any of the tetracyclines; however, vertigo is more common with the use of minocycline.
Drug Interactions
Patients should not drink milk or take any dairy or calcium while taking these medications. Tetracyclines bind with calcium and iron and may reduce the drug’s absorption up to 50%. Tetracycline is best taken with water on an empty stomach 1 hour before eating or 2 hours after eating.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Tetracycline products that are out of date (older than the expiration date on the label) should not be used, because it may lead to damage of the proximal renal tubules.
Doxycycline (Vibramycin) is a particularly good drug, especially for the older adult population because it may be taken twice daily and is usually tolerated even by some individuals who have reduced renal function.
Macrolides
Action
Macrolides such as erythromycin are either bacteriocidal or bacteriostatic depending on the organisms and the dose used. Marcolides weaken the bacteria by limiting the production of protein, which is essential to the life of the bacteria.
Uses
The macrolides are used as alternatives to penicillin for many infections for which organisms have developed penicillin resistance. They are the drugs of choice in Streptococcus infections, Haemophilus influenza, Mycoplasma pneumoniae, and Chlamydia infections. They are also used in legionnaires disease and in the treatment of pertussis (“whooping cough”).
Adverse Reactions
Macrolides are associated with very few serious side effects. They are often considered a safe first choice for patients with uncomplicated infection. Mild abdominal pain, nausea, and diarrhea are the most common effects. Watch for signs of superinfection.
Drug Interactions
Macrolides increase the action of oral anticoagulants, digoxin, and many other drugs and thus may produce both drug and kidney toxicity. A drug handbook should be consulted whenever other drugs are given along with a macrolide. Anesthetic agents and anticonvulsant drugs may interact to cause high serum drug levels and toxicity.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
The major differences between erythromycin and the newer macrolides include better GI tolerability, a broader spectrum of activity, and less dosing frequency for the newer products. Giving the medication with food reduces GI irritation.
Caution should be used when this drug is given with any other medication because of the risk of drug-drug interactions and increase of adverse effects.
The strength of erythromycin varies by product. The strength of different products are reported as the erythromycin base equivalence. Because of differences in absorption, 400 mg of ethylsuccinate is required to provide the same free erythromycin serum levels as 250 mg of erythromycin base, stearate, or estolate. This accounts for the differences in doses of different erythromycin products.
Many macrolides may be administered orally or parenterally. Topical application should be avoided to prevent sensitization. The patient should be kept well hydrated (supplied with fluids). Drinking extra fluids to ensure a minimum urine output of 1500 mL decreases the chances of renal toxicity.
All chewable forms of erythromycin must be fully chewed to obtain the complete therapeutic effect.
Aminoglycosides
Action
Aminoglycosides weaken the bacteria by limiting the production of protein, which is essential to the life of the bacteria.
Uses
These products, such as gentamycin and amikacin, are used in the treatment of serious aerobic gram-negative infections, including those caused by Escherichia coli, Serratia, Proteus, Klebsiella, and Pseudomonas; aerobic gram-negative bacteria, mycobacteria, and some protozoans. Streptomycin (SM) is used in the treatment of TB. Some products are used to sterilize the bowel before intestinal surgery.
Adverse Reactions
Aminoglycosides may cause serious adverse effects including damage to the kidney (nephrotoxicity) that is usually reversible if the drug is stopped quickly. They may also produce permanent damage to the inner ear (ototoxicity), hearing impairment, dizziness, loss of balance, ringing in the ears, and persistent headache. Aminoglycosides have a narrow therapeutic range, so the blood levels of these drugs should be closely watched to avoid toxic levels. Dosage is calculated on the basis of the patient’s weight and is increased or decreased based on blood levels so an effective level is maintained. The narrow therapeutic range (when the lowest and highest acceptable drug levels are not far apart) requires that the sample for the antibiotic blood level be drawn just before the next scheduled dose is given. This sample will show the lowest blood level of the antibiotic (found at the “trough”), rather than a blood level at a higher range (at or near the “peak”). The lowest blood level will determine whether the dosage needs to be adjusted to stay within the therapeutic range and not go above the toxic level or below the effective level. Because of the nephrotoxicity of these agents, blood urea nitrogen and creatinine levels must also be monitored during the course of therapy.
Drug Interactions
Using this drug with many products, particularly vancomycin, increases the risk of nephrotoxicity. Ototoxicity is also increased with aspirin, furosemide, ethacrynic acid, and many other drugs.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Some of these products are available over-the-counter (OTC) or by prescription for eye, ear, or skin infections. When given for systemic bacterial infections they must be given parenterally as they are poorly absorbed from the GI tract.
Patients should have frequent hearing and urine tests to monitor for nephrotoxicity and ototoxicity.
Fluoroquinolones
Action
Fluroquinolones are bacteriocidal and act by interfering with bacterial DNA synthesis, which makes it difficult for the pathogens to reproduce themselves and attack other cells.
Uses
There are four generations of fluoroquinolones, which are all effective against gram-negative pathogens. The newer ones are significantly more effective against gram-positive microbes. These agents are used as alternatives to other antibiotics in the treatment of respiratory, GI, gynecologic, skin, and soft-tissue infections. Ciprofloxin (Cipro) is the drug of choice for anthrax exposure in a bioterrorist attack.
Adverse Reactions
Fluoroquinolones are generally viewed as safe drugs for most patients. Nausea, vomiting, and diarrhea are the most common side effects and may occur in up to 20% of patients. Patients may also have headache, dizziness, and abnormal heart rhythms.
Drug Interactions
Fluoroquinolones should not be taken with multivitamins or mineral supplements because they reduce the absorption of the antibiotic by as much as 90%. When taken with warfarin, fluoroquinolones will increase warfarin’s anticoagulant effects. Antacids and ferrous sulfate may decrease absorption of the drugs. Patients may develop excessive nervousness, anxiety, or tachycardia if taken with coffee or other caffeine-containing products.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Fluoroquinolones are well absorbed orally and may be given only once or twice per day. Take drug with food to decrease adverse GI effects.
Cephalosporins
Action
Cephalosporins are bactericidal and weaken the bacteria by interfering with building of the bacteria’s cell wall.
Uses
There are four generations of cephalosporins, all of which have broad spectrum activity against gram-negative organisms. In general, second- and third-generation drugs are more effective and more potent than first-generation agents against a broad group of gram-negative organisms; however, they are also less effective against gram-positive organisms. Third-generation agents are also more effective against inactivation by beta-lactamase (an enzyme that some organisms make to protect them against the action of some antibiotics). However, these agents cost more and may have more side effects. Differences among drugs within categories are primarily based on the drug’s activity. Later-generation drugs are more effective against some of the organisms to which earlier generation agents have been resistant.
Cephalosporins are used for serious infections, like bacteremia and septicemia (infections of the blood); and infections of the lower respiratory tract, central nervous system (CNS), genitourinary system, joints, and bones. These drugs are also used in patients who cannot take penicillin.
Adverse Reactions
Nausea, vomiting, and diarrhea are frequent. The most common adverse effect is acute hypersensitivity. Although some patients may have only a minor rash and itching, anaphylaxis is possible. There may be severe pain at the injection site. Nephrotoxicity has been reported with some cephalosporins, and the incidence is greater in older adult patients and in patients with poor renal function.
Drug Interactions
Alcohol taken with these products may produce a severe disulfiram reaction resulting in severe flushing, vomiting, and collapse. Other products, such as probenecid, may decrease elimination of the drugs by the kidneys.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Must be given by the IV or IM route because it is not absorbed from the GI tract.
Patients who have had a recent and severe reaction to penicillin should not be prescribed these products.
Sulfonamides
Action
Sulfonamides have a bacteriostatic effect against a wide range of gram-positive and gram-negative microorganisms by inhibiting folic acid synthesis, which is essential for cell growth and function.
Uses
Sulfonamides are usually used to treat acute and chronic urinary tract infections, particularly cystitis, pyelitis, and pyelonephritis caused by E. coli or Nocardia asteroides. Other indications include toxoplasmosis, acute otitis media caused by H. influenzae, and preventive therapy in cases of recurrent rheumatic fever. Susceptible organisms include Streptococcus pyogenes, Streptococcus pneumoniae, some strains of Bacillus anthracis, C. diphtheriae, Haemophilus ducreyi, Chlamydia trachomatis, and other less common organisms. Several sulfonamides are useful only in the treatment of ulcerative colitis, and as preoperative and postoperative therapy for bowel surgery.
Adverse Reactions
Adverse reactions to sulfonamides include many minor but irritating problems such as headache, drowsiness, fatigue, dizziness, vertigo (feeling of dizziness or spinning), tinnitus (ringing in the ears), hearing loss, insomnia (inability to sleep), anorexia (lack of appetite), nausea, vomiting, stomatitis (inflammation of the mouth), abdominal pain, rash, fever, malaise (weakness), pruritus (itching), dermatitis, local irritation, anaphylactic shock, crystalluria (formation of crystals in the urine), hematuria (blood in the urine), and proteinuria (large amounts of protein in the urine) may develop with overdosage and indicate that the patient may have a severe hypersensitivity to sulfonamides.
Drug Interactions
Sulfonamides may increase the effect of oral anticoagulants, methotrexate, sulfonylureas, thiazide diuretics, phenytoin, and uricosuric agents. Many other drugs taken at the same time will cause the effects of sulfonamides to be increased. Penicillins may be less effective when given with a sulfonamide. The sulfonamide’s effect may be decreased by local anesthetics. Antacids may cause less absorption of the sulfonamide. Sulfonamides may change the results of various laboratory tests including urine glucose.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Warn the patient to stay out of the sun, because severe photosensitivity (abnormal response to exposure to sunlight) can occur if the patient’s skin is exposed to excessive amounts of sunlight or ultraviolet light.
Sulfonamide dosage depends on the severity of the infection being treated, the drug used, and the patient’s response to and tolerance of the drug. Generally, the short-acting sulfonamides are given at more frequent intervals than are the intermediate- or long-acting sulfonamides. Also, short-acting sulfonamides usually require a special first dose (initial loading dose) that is larger than the dose that will be regularly taken.
Sulfonamides are more fully and quickly absorbed when they are taken on an empty stomach. They should be taken either 1 hour before or 2 hours after meals, along with a full glass of water.
To prevent formation of crystals in the urine, the patient must drink large amounts of water while taking this medication.
It is particularly important with these drugs that the patient should take all the medication prescribed and not stop just because the symptoms have disappeared, so they do not have a relapse.
The health care provider should be notified quickly if a skin rash, blood in the urine, bruises, nausea, or other adverse effects of therapy develop because these may indicate development of more severe reactions.
Miscellaneous Antiinfective Drugs
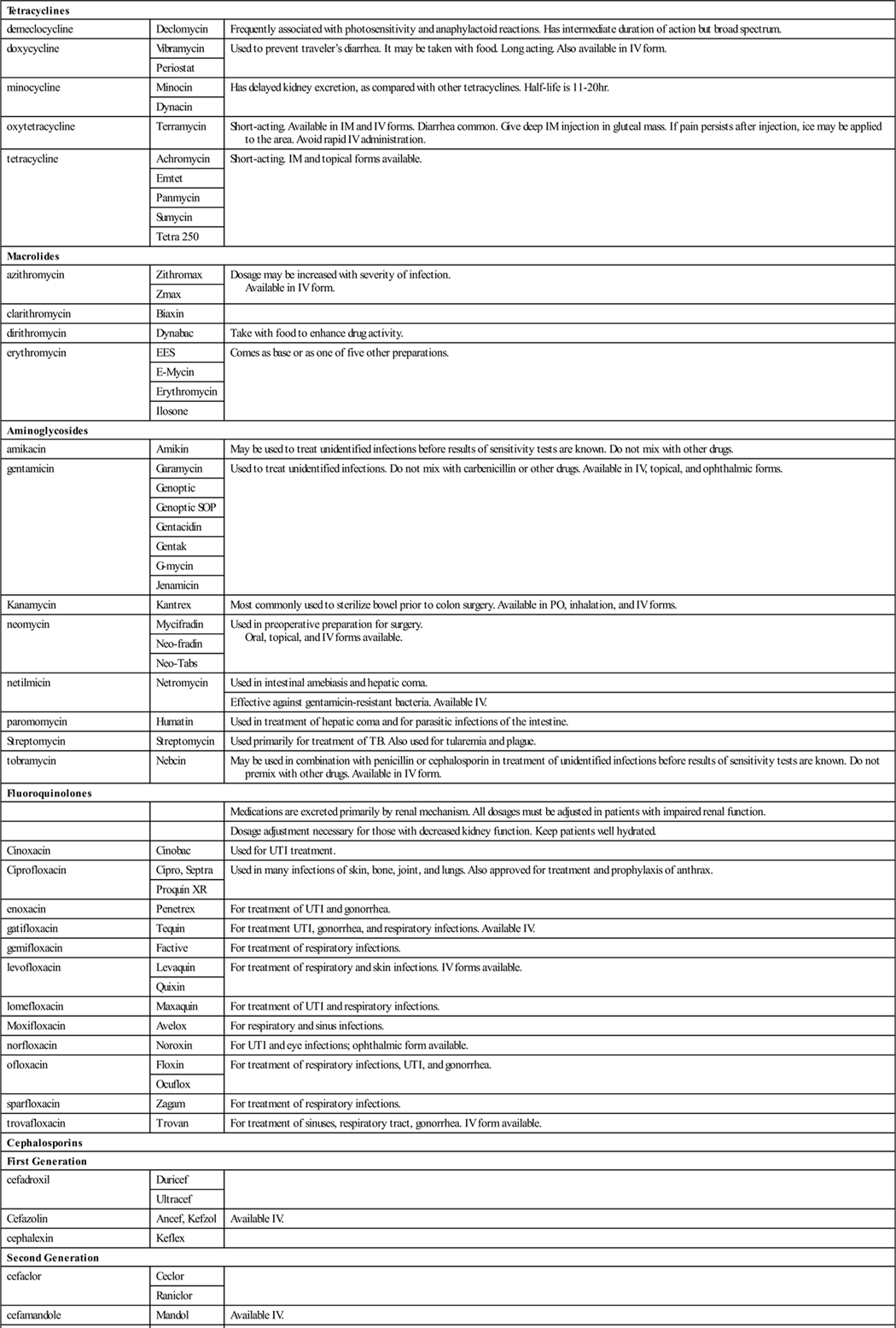
There are many other antiinfective agents on the market, some representing drug classes that are no longer widely used, some with very narrow uses, and some new drugs, which nurses may occasionally see ordered. Two of the most important, carbapenem and vancomycin, are described here in greater detail. A selection of other drugs are presented only in Table 12-2.
![]() Table 12-2
Table 12-2
| Tetracyclines | ||
| demeclocycline | Declomycin | Frequently associated with photosensitivity and anaphylactoid reactions. Has intermediate duration of action but broad spectrum. |
| doxycycline | Vibramycin | Used to prevent traveler’s diarrhea. It may be taken with food. Long acting. Also available in IV form. |
| Periostat | ||
| minocycline | Minocin | Has delayed kidney excretion, as compared with other tetracyclines. Half-life is 11-20 hr. |
| Dynacin | ||
| oxytetracycline | Terramycin | Short-acting. Available in IM and IV forms. Diarrhea common. Give deep IM injection in gluteal mass. If pain persists after injection, ice may be applied to the area. Avoid rapid IV administration. |
| tetracycline | Achromycin | Short-acting. IM and topical forms available. |
| Emtet | ||
| Panmycin | ||
| Sumycin | ||
| Tetra 250 | ||
| Macrolides | ||
| azithromycin | Zithromax | Dosage may be increased with severity of infection. Available in IV form. |
| Zmax | ||
| clarithromycin | Biaxin | |
| dirithromycin | Dynabac | Take with food to enhance drug activity. |
| erythromycin | EES | Comes as base or as one of five other preparations. |
| E-Mycin | ||
| Erythromycin | ||
| Ilosone | ||
| Aminoglycosides | ||
| amikacin | Amikin | May be used to treat unidentified infections before results of sensitivity tests are known. Do not mix with other drugs. |
| gentamicin | Garamycin | Used to treat unidentified infections. Do not mix with carbenicillin or other drugs. Available in IV, topical, and ophthalmic forms. |
| Genoptic | ||
| Genoptic SOP | ||
| Gentacidin | ||
| Gentak | ||
| G-mycin | ||
| Jenamicin | ||
| Kanamycin | Kantrex | Most commonly used to sterilize bowel prior to colon surgery. Available in PO, inhalation, and IV forms. |
| neomycin | Mycifradin | Used in preoperative preparation for surgery. Oral, topical, and IV forms available. |
| Neo-fradin | ||
| Neo-Tabs | ||
| netilmicin | Netromycin | Used in intestinal amebiasis and hepatic coma. |
| Effective against gentamicin-resistant bacteria. Available IV. | ||
| paromomycin | Humatin | Used in treatment of hepatic coma and for parasitic infections of the intestine. |
| Streptomycin | Streptomycin | Used primarily for treatment of TB. Also used for tularemia and plague. |
| tobramycin | Nebcin | May be used in combination with penicillin or cephalosporin in treatment of unidentified infections before results of sensitivity tests are known. Do not premix with other drugs. Available in IV form. |
| Fluoroquinolones | ||
| Medications are excreted primarily by renal mechanism. All dosages must be adjusted in patients with impaired renal function. | ||
| Dosage adjustment necessary for those with decreased kidney function. Keep patients well hydrated. | ||
| Cinoxacin | Cinobac | Used for UTI treatment. |
| Ciprofloxacin | Cipro, Septra | Used in many infections of skin, bone, joint, and lungs. Also approved for treatment and prophylaxis of anthrax. |
| Proquin XR | ||
| enoxacin | Penetrex | For treatment of UTI and gonorrhea. |
| gatifloxacin | Tequin | For treatment UTI, gonorrhea, and respiratory infections. Available IV. |
| gemifloxacin | Factive | For treatment of respiratory infections. |
| levofloxacin | Levaquin | For treatment of respiratory and skin infections. IV forms available. |
| Quixin | ||
| lomefloxacin | Maxaquin | For treatment of UTI and respiratory infections. |
| Moxifloxacin | Avelox | For respiratory and sinus infections. |
| norfloxacin | Noroxin | For UTI and eye infections; ophthalmic form available. |
| ofloxacin | Floxin | For treatment of respiratory infections, UTI, and gonorrhea. |
| Ocuflox | ||
| sparfloxacin | Zagam | For treatment of respiratory infections. |
| trovafloxacin | Trovan | For treatment of sinuses, respiratory tract, gonorrhea. IV form available. |
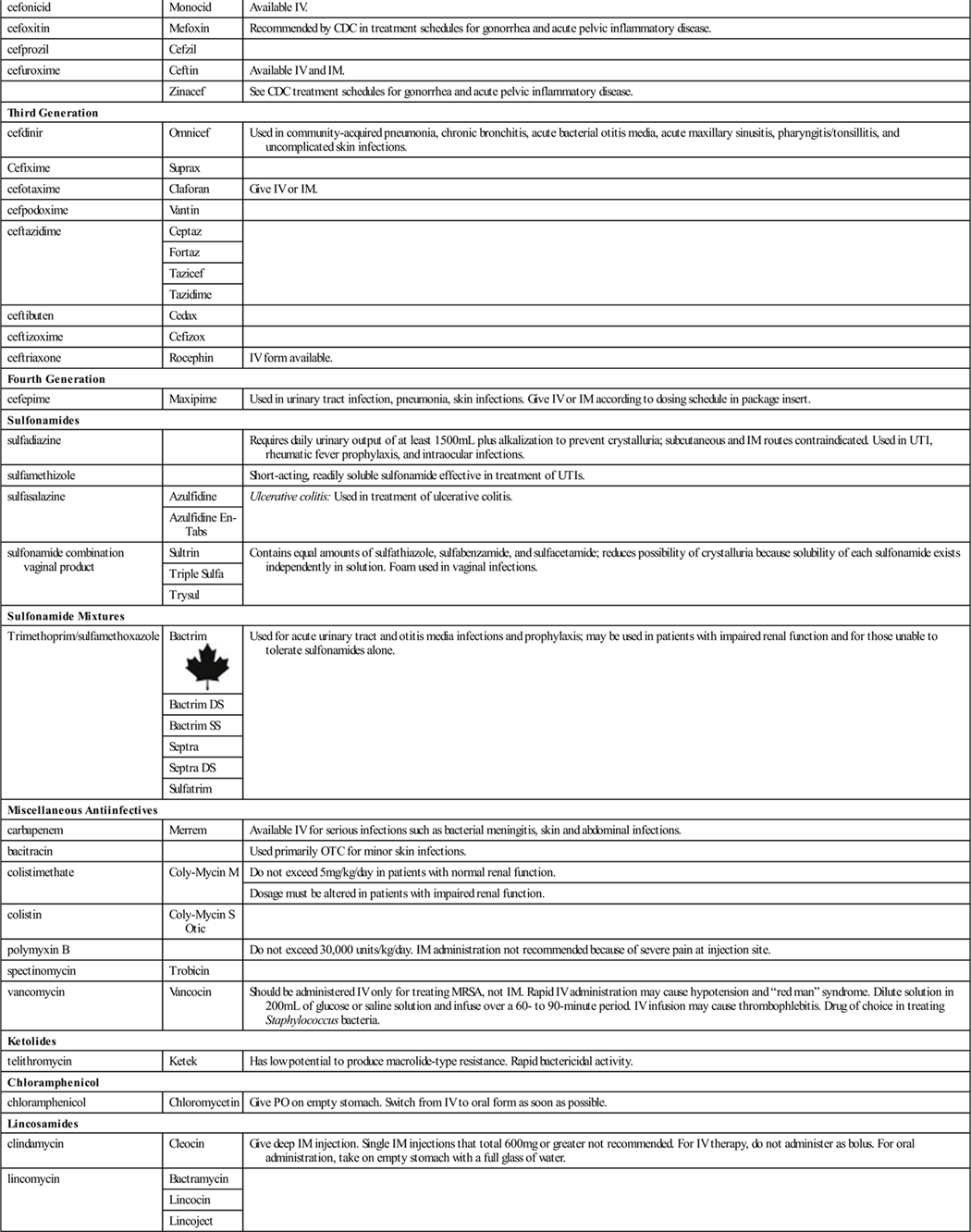
| Cephalosporins | ||
| First Generation | ||
| cefadroxil | Duricef | |
| Ultracef | ||
| Cefazolin | Ancef, Kefzol | Available IV. |
| cephalexin | Keflex | |
| Second Generation | ||
| cefaclor | Ceclor | |
| Raniclor | ||
| cefamandole | Mandol | Available IV. |
| cefonicid | Monocid | Available IV. |
| cefoxitin | Mefoxin | Recommended by CDC in treatment schedules for gonorrhea and acute pelvic inflammatory disease. |
| cefprozil | Cefzil | |
| cefuroxime | Ceftin | Available IV and IM. |
| Zinacef | See CDC treatment schedules for gonorrhea and acute pelvic inflammatory disease. | |
| Third Generation | ||
| cefdinir | Omnicef | Used in community-acquired pneumonia, chronic bronchitis, acute bacterial otitis media, acute maxillary sinusitis, pharyngitis/tonsillitis, and uncomplicated skin infections. |
| Cefixime | Suprax | |
| cefotaxime | Claforan | Give IV or IM. |
| cefpodoxime | Vantin | |
| ceftazidime | Ceptaz | |
| Fortaz | ||
| Tazicef | ||
| Tazidime | ||
| ceftibuten | Cedax | |
| ceftizoxime | Cefizox | |
| ceftriaxone | Rocephin | IV form available. |
| Fourth Generation | ||
| cefepime | Maxipime | Used in urinary tract infection, pneumonia, skin infections. Give IV or IM according to dosing schedule in package insert. |
| Sulfonamides | ||
| sulfadiazine | Requires daily urinary output of at least 1500 mL plus alkalization to prevent crystalluria; subcutaneous and IM routes contraindicated. Used in UTI, rheumatic fever prophylaxis, and intraocular infections. | |
| sulfamethizole | Short-acting, readily soluble sulfonamide effective in treatment of UTIs. | |
| sulfasalazine | Azulfidine | Ulcerative colitis: Used in treatment of ulcerative colitis. |
| Azulfidine En-Tabs | ||
| sulfonamide combination vaginal product | Sultrin | Contains equal amounts of sulfathiazole, sulfabenzamide, and sulfacetamide; reduces possibility of crystalluria because solubility of each sulfonamide exists independently in solution. Foam used in vaginal infections. |
| Triple Sulfa | ||
| Trysul | ||
| Sulfonamide Mixtures | ||
| Trimethoprim/sulfamethoxazole | Bactrim |
Used for acute urinary tract and otitis media infections and prophylaxis; may be used in patients with impaired renal function and for those unable to tolerate sulfonamides alone. |
| Bactrim DS | ||
| Bactrim SS | ||
| Septra | ||
| Septra DS | ||
| Sulfatrim | ||
| Miscellaneous Antiinfectives | ||
| carbapenem | Merrem | Available IV for serious infections such as bacterial meningitis, skin and abdominal infections. |
| bacitracin | Used primarily OTC for minor skin infections. | |
| colistimethate | Coly-Mycin M | Do not exceed 5 mg/kg/day in patients with normal renal function. |
| Dosage must be altered in patients with impaired renal function. | ||
| colistin | Coly-Mycin S Otic | |
| polymyxin B | Do not exceed 30,000 units/kg/day. IM administration not recommended because of severe pain at injection site. | |
| spectinomycin | Trobicin | |
| vancomycin | Vancocin | Should be administered IV only for treating MRSA, not IM. Rapid IV administration may cause hypotension and “red man” syndrome. Dilute solution in 200 mL of glucose or saline solution and infuse over a 60- to 90-minute period. IV infusion may cause thrombophlebitis. Drug of choice in treating Staphylococcus bacteria. |
| Ketolides | ||
| telithromycin | Ketek | Has low potential to produce macrolide-type resistance. Rapid bactericidal activity. |
| Chloramphenicol | ||
| chloramphenicol | Chloromycetin | Give PO on empty stomach. Switch from IV to oral form as soon as possible. |
| Lincosamides | ||
| clindamycin | Cleocin | Give deep IM injection. Single IM injections that total 600 mg or greater not recommended. For IV therapy, do not administer as bolus. For oral administration, take on empty stomach with a full glass of water. |
| lincomycin | Bactramycin | |
| Lincocin | ||
| Lincoject | ||
Miscellaneous Agent—Carbapenem
Action
Carbapenem is a broad-spectrum antibiotics are effective against gram-positive and gram-negative bacteria. They penetrate bacterial cells and interfere with the making of vital cell wall parts, which leads to cell death, making them bactericidal.
Uses
Carbapenem is used in acute infections caused by bacterial meningitis, intraabdominal infections, skin, and skin structure infections.
Adverse Reactions
Carbapenem may produce pseudomembranous colitis, hypersensitivity reactions, and impaired renal function.
Nausea, vomiting, diarrhea, headache, rash, sepsis, constipation, apnea, shock, and pruritus were all reported.
Drug Interactions
Carbapenem competes with probenecid, so these drugs should not be given at the same time. The drug may reduce the activity of valproic acid, which is given to prevent seizures.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
Carbapenem is administered intravenously. Reduced dose is required in patients with reduced kidney function. Watch for adverse effects, as they are frequent.
Miscellaneous Agent—Vancomycin
Action
This drug is bacteriocidal, inhibiting the building of the bacterial cell-wall.
Uses
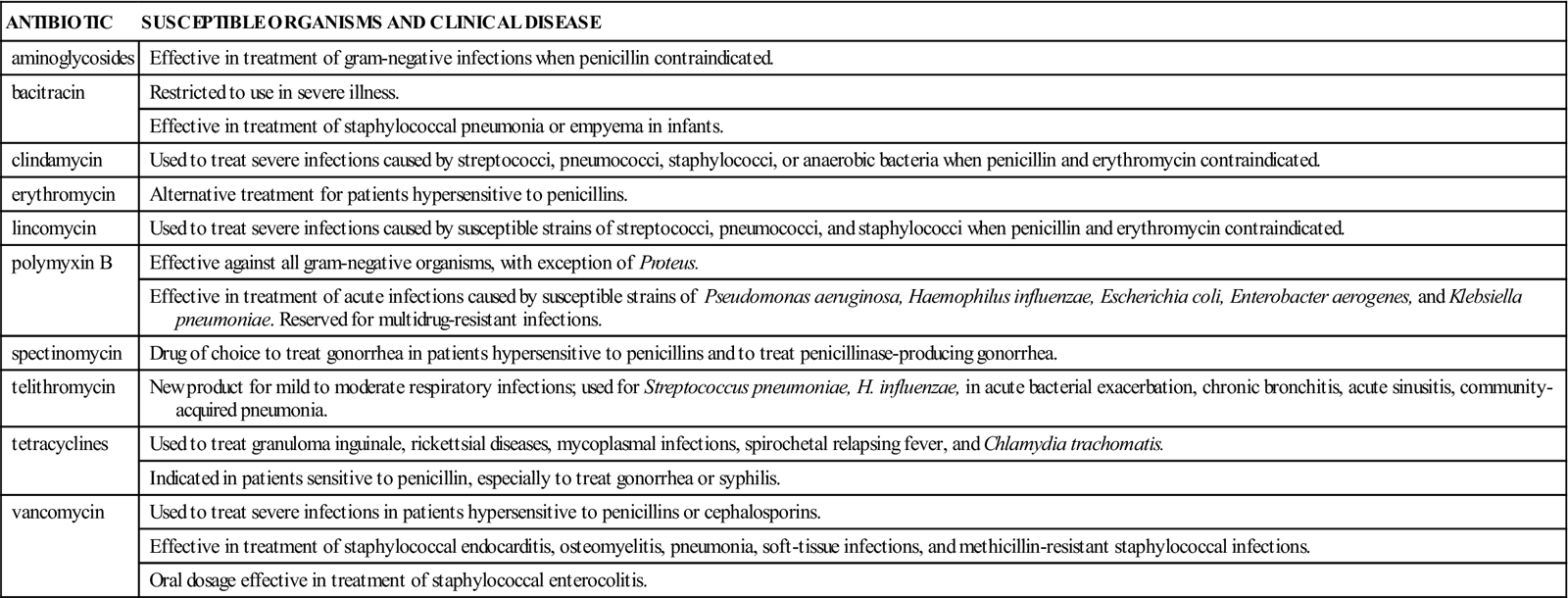
Vancomycin is an antibiotic usually reserved for severe gram-positive infections such as Staphylococcus aureus and Pneumocystis pneumoniae. It is one of the powerful antibiotics to which most organisms are still sensitive (Table 12-3). It is used for treating methicillin-resistant S. aureus (MRSA) infections.
![]() Table 12-3
Table 12-3
Sensitivity of Specific Organisms to Some Broad-Spectrum Antibiotics
| ANTIBIOTIC | SUSCEPTIBLE ORGANISMS AND CLINICAL DISEASE |
| aminoglycosides | Effective in treatment of gram-negative infections when penicillin contraindicated. |
| bacitracin | Restricted to use in severe illness. |
| Effective in treatment of staphylococcal pneumonia or empyema in infants. | |
| clindamycin | Used to treat severe infections caused by streptococci, pneumococci, staphylococci, or anaerobic bacteria when penicillin and erythromycin contraindicated. |
| erythromycin | Alternative treatment for patients hypersensitive to penicillins. |
| lincomycin | Used to treat severe infections caused by susceptible strains of streptococci, pneumococci, and staphylococci when penicillin and erythromycin contraindicated. |
| polymyxin B | Effective against all gram-negative organisms, with exception of Proteus. |
| Effective in treatment of acute infections caused by susceptible strains of Pseudomonas aeruginosa, Haemophilus influenzae, Escherichia coli, Enterobacter aerogenes, and Klebsiella pneumoniae. Reserved for multidrug-resistant infections. | |
| spectinomycin | Drug of choice to treat gonorrhea in patients hypersensitive to penicillins and to treat penicillinase-producing gonorrhea. |
| telithromycin | New product for mild to moderate respiratory infections; used for Streptococcus pneumoniae, H. influenzae, in acute bacterial exacerbation, chronic bronchitis, acute sinusitis, community-acquired pneumonia. |
| tetracyclines | Used to treat granuloma inguinale, rickettsial diseases, mycoplasmal infections, spirochetal relapsing fever, and Chlamydia trachomatis. |
| Indicated in patients sensitive to penicillin, especially to treat gonorrhea or syphilis. | |
| vancomycin | Used to treat severe infections in patients hypersensitive to penicillins or cephalosporins. |
| Effective in treatment of staphylococcal endocarditis, osteomyelitis, pneumonia, soft-tissue infections, and methicillin-resistant staphylococcal infections. | |
| Oral dosage effective in treatment of staphylococcal enterocolitis. |
Adverse Reactions
May be associated with minor hypersensitivity reactions or anaphylaxis. This drug causes frequent but minor side effects such as rash on the upper body (red-man syndrome), flushing, and hypotension. Higher doses may produce nephrotoxicity and ototoxicity.
Drug Interactions
This drug adds to the toxicity of other antibiotics such as the aminoglycosides, and other products that are ototoxic or nephrotoxic. Cholestyramine and colestipol decrease the absorption of the drug.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
This drug is usually given intravenously because it is not absorbed from the GI tract (Table 12-3).
Significant reactions to antibiotics are summarized in Table 12-4.
![]() Table 12-4
Table 12-4
Significant Adverse Reactions Produced by Specific Broad-Spectrum Antibiotics
| ANTIBIOTIC | ADVERSE REACTION |
| aminoglycosides | Significant renal toxicity, which is usually reversible; risk of toxicity increases in patients with renal impairment. Significant auditory and vestibular ototoxicity may occur in patients on prolonged therapy or those taking higher than recommended dosages. |
| bacitracin | Renal toxicity leading to tubular and glomerular necrosis has been reported. Also, increased serum drug levels without an increase in drug dosage and severe pain and rash with IM injection are seen. |
| cephalosporins | Painful IM injections; thrombophlebitis with IV therapy. May produce hemolytic anemia and other blood dyscrasias. |
| clindamycin | Severe and fatal colitis characterized by abdominal cramps, diarrhea, and rectal passage of blood and mucus (these symptoms may not appear until after treatment is completed). |
| colistin | Renal toxicity; transient neurologic disturbances have been reported with colistimethate, as well as nephrotoxicity manifested by decreased urinary output and increased serum creatinine. |
| erythromycin | GI distress, sensorineural hearing loss, and hepatotoxicity possible. |
| lincomycin | Severe and fatal colitis characterized by abdominal cramps, diarrhea, or rectal passage of blood and mucus (these symptoms may not develop until treatment is completed). Hypotension and cardiac arrest may occur after rapid IV administration. |
| polymyxin B | Nephrotoxicity may develop, evidenced by proteinuria, cellular urinary casts, azotemia, decreased output, or elevated BUN. Neurotoxicity may be evidenced by irritability, weakness, drowsiness, ataxia, numbness of extremities, blurring of vision, or respiratory paralysis. |
| tetracycline | Black, “hairy” tongue possible; oral dosage effective in treatment of staphylococcal enterocolitis. |
| vancomycin | Nephrotoxicity with toxic effect increased at high serum levels or with prolonged therapy; ototoxicity may also occur. |
BUN, Blood urea nitrogen; GI, gastrointestinal; IM, intramuscular; IV, intravenous.
 Nursing Implications and Patient Teaching for Antibiotics in General
Nursing Implications and Patient Teaching for Antibiotics in General 
n Assessment
Watch for common indicators of infection, such as fever, redness, swelling, or pain.
Find out as much as possible about the patient’s health history, including prior renal damage, hepatic problems, systemic lupus erythematosus, alcoholism, or drugs that may interact with an antibiotic. Ask about pregnancy or breastfeeding, age, and occupation (i.e. If they are a cook in a restaurant or working with young children or are around people who are immunocompromised). These factors may be contraindications or precautions to antibiotic drug therapy.
n Diagnosis
Are there other factors that may pose a problem to the patient taking this drug? For example, patients reporting any previous allergy to one drug may also be allergic to some other drugs.
n Planning
Many broad-spectrum antibiotics cross the placental barrier and are secreted in breast milk.
Many of the parenteral antibiotics should be used with caution because of their toxic effects. Most antibiotics should be given with extreme caution to patients with poor renal function, but the risk of toxicity is low in patients with normal renal function.
n Implementation
The nurse should make certain the drugs are taken at the proper time in order to maintain blood levels of the antibiotic and for the full course of the therapy. The dosage depends on the type and the severity of the infection.
n Evaluation
Superinfection may occur in the patient who is taking extended antibiotic therapy. Monitor for infections in the mouth and the rectal or vaginal areas.
Because of the possibility of ototoxicity in patients taking vancomycin, watch for patient complaints of tinnitus, or ringing in the ears, which may be a sign that the patient is at risk for deafness.
With some broad-spectrum antibiotics, the nurse will monitor for liver toxicity by checking for abdominal pain, jaundice, dark urine, pale-colored stools, or weakness. Blood or mucus in the stools may indicate colitis. If large doses of antibiotics are given, the patient should be monitored closely for sensorineural hearing loss. Observe the patient for therapeutic effects, allergy, and superinfection.
n Patient and Family Teaching
Tell the patient and family the following:
• If GI upset occurs, the patient should eat a few plain crackers with the medicine.
• Liquid medication should be kept in a dark colored and light-resistant container.
Table 12-5 presents a summary of the broad-spectrum antibiotics.
![]() Table 12-5
Table 12-5
| GENERIC NAME | TRADE NAME | COMMENTS |
| Primary Treatment Agents | ||
| ethambutol | Myambutol |
Give once every 24 hr. When one other bactericidal drug is used in combination with this medication, therapy generally lasts 18-24 months. It has been used in twice-weekly regimens. Ethambutol may be taken with food; watch for optic neuritis, rash. |
| isoniazid | Isoniazid INH Nydrazid |
Well absorbed after PO or IM administration. Dosage is determined by weight, with the usual adult dose being 5 mg/kg or 300 mg/day. Children require higher doses than adults. Give with pyridoxine to reduce incidence of peripheral neuropathies. Isoniazid is the drug of choice in the prophylactic treatment of TB infections. Watch for hepatic and neurologic toxicity. |
| pyrazinamide | Pyrazinamide |
Should be administered with at least one other antitubercular drug. |
| Watch for hepatic toxicity and hyperuricemia, arthralgia, and arthritis. | ||
| rifampin | Rifadin | Used in combination with other antitubercular drugs. Peak plasma concentrations occur 2-4 hr after ingestion. Watch for hepatic and hematologic toxicity. |
| Rimactane | ||
| rifapentine | Priftin | |
| streptomycin | Used in TB and also for other serious bacterial infections. May be given IM although injection is painful. | |
| Retreatment Agents | ||
| para-aminosalicylate (PAS) | Paser | May produce nausea, vomiting, diarrhea, or abdominal pain. Watch for GI distress, hepatitis. |
| capreomycin | Capastat Sulfate | Give deep IM. Watch for renal and eighth cranial nerve toxicity. |
| cycloserine | Seromycin Pulvules | Watch for psychoses, seizures, rash. |
| ethionamide | Trecator-SC | Take with meals or antacids to reduce GI distress. High percentage of patients cannot tolerate therapeutic dose. |
| Dosages should never exceed 1 g/day. Usual dose is 0.5-1 g/day PO. Watch for hepatitis, GI distress, hypersensitivity. | ||
| kanamycin | Kantrex | Watch for renal and eighth cranial nerve toxicity. |
| Prevention In HIV Patients | ||
| rifabutin | Mycobutin | Divided dose, taken with food, may decrease GI distress. |
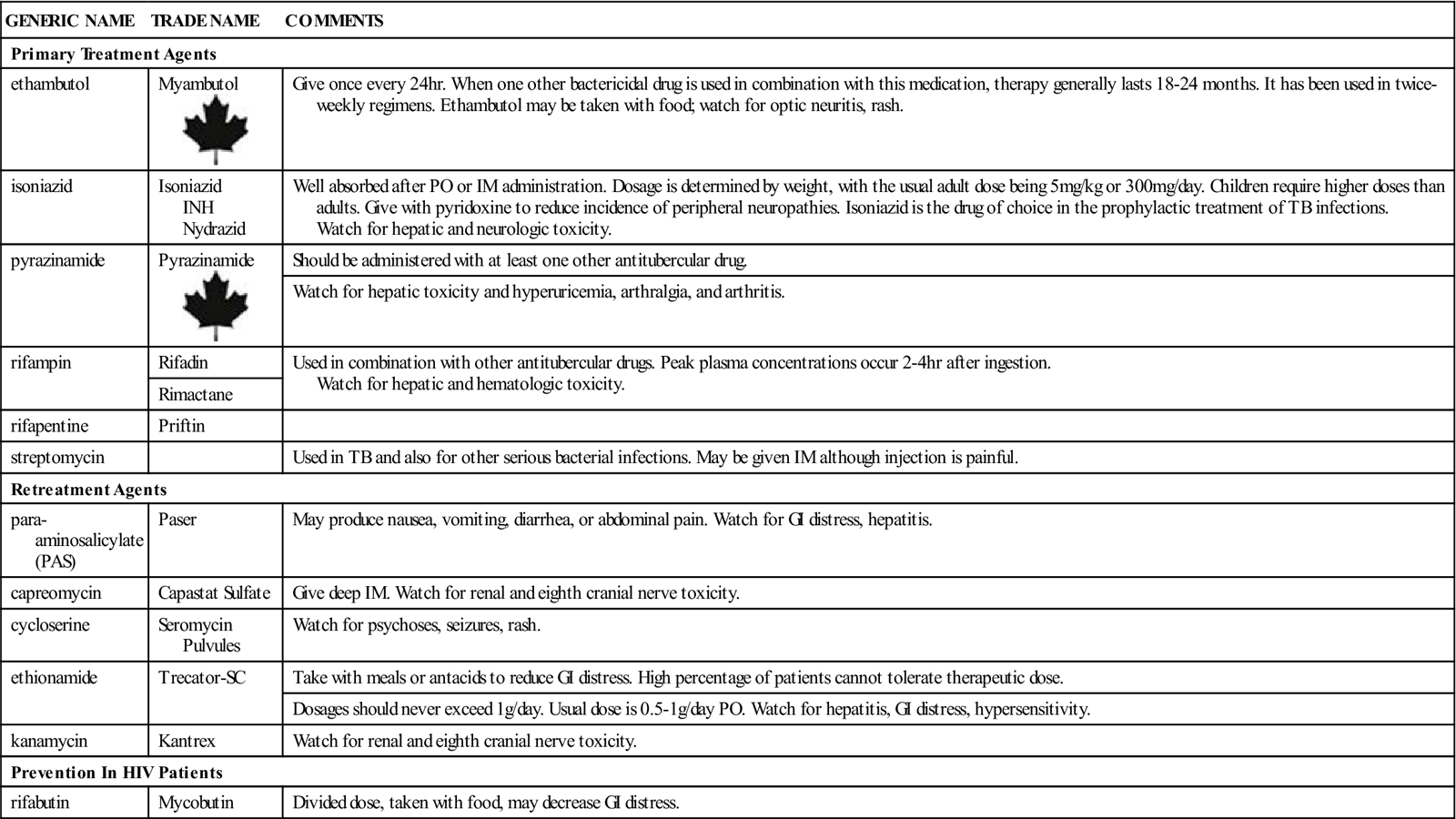
GI, Gastrointestinal; IM, intramuscular; PO, by mouth; TB, tuberculosis.
Antitubercular Drugs 
Overview
Tuberculosis is disease seen in ancient times and still found among poor and undernourished people. It is most commonly seen in underdeveloped nations where living conditions are crowded and unsanitary. However, it is also increasingly found in the United States among immigrants, drug users, alcoholics, and AIDS patients or others with lowered immunity. The diagnosis of TB centuries ago was a death sentence. It is once again a frightening disease because so many drugs are no longer effective against it. It is primarily a disease of the lungs but may also be seen in bones, bladder, and other parts of the body. At present, most cases of infectious TB are found in people who have not been adequately treated with antitubercular medications and in people who contract primary TB as a result of reduced immunity from human immunodeficiency virus (HIV) infection. TB may once again become a major killer.
TB is caused by the bacterium Mycobacterium tuberculosis, which infects animals as well as humans. Multidrug-resistant (MDR) organisms (strains that are resistant to current drugs) are now commonly found and require vigorous methods of treatment to control infection. New guidelines for treatment of TB are published by the Centers for Disease Control and Prevention (CDC) almost every year. Because there are many new cases of TB, as well as numerous untreated cases, new state laws have been passed that take aggressive action against individuals who are infected with TB and refuse to take or complete adequate drug therapy. To control the high numbers of new cases of TB, in some states, uncooperative patients may actually be sent to prison until they have completed the required drug therapy and have been rendered noninfectious.
Action
The main action of antitubercular drugs take place both within or outside the cell wall of the bacteria that slow down the M. tuberculosis bacteria. Most drugs used to treat TB do not kill the bacterium, but they control the disease and prevent its spread to various organ systems in the infected patient or to other individuals. The drugs control the bacteria by preventing them from producing new cell walls, so new bacterial cell growth is limited. Some antitubercular drugs are bactericidal, killing the organism.
Uses
Chemoprophylaxis, or taking a drug to prevent disease, is recommended when the patient is at high risk of developing active TB. The current duration of prophylactic treatment is 1 year. At present, isoniazid (INH) is the only drug recommended for prophylactic therapy. INH prophylaxis is not recommended for healthy individuals older than 35 because of their increased risk of developing hepatitis. Prophylaxis is recommended, however, if the patient is at special risk for developing TB, as indicated in Box 12-1. Chemotherapy, or taking a drug to treat disease, is recommended for patients with active tuberculosis.
Antitubercular drugs are classified as primary or secondary agents to describe the way they are used in treating TB. Most primary agents are bactericidal and are necessary to sterilize the TB lesions. Secondary agents are generally less effective and more toxic than primary agents. They are used with primary agents for patients infected with partially or completely drug-resistant organisms or to treat lesions found outside the lungs.
Adverse Reactions
Mycobacterium tuberculosis is able to build up a resistance to antitubercular drugs. Use of a combination of drugs helps slow the development of bacterial resistance. Most of the antitubercular medications cause only mild and infrequent symptoms such as nausea, vomiting, and diarrhea. Most of these symptoms stop when the dosage is reduced. Some of the drugs used to treat TB are toxic to various parts of the body (for example, the ears, kidneys, and liver). The patient must be watched closely to detect development of any of these more serious problems. All drugs are associated with some adverse reactions. Those for treating TB have many adverse reactions in the body. The most common or most serious are briefly described in the following text.
Capreomycin may cause headache, ototoxicity (hearing loss, tinnitus, vertigo), nephrotoxicity, abnormal liver function tests, maculopapular rash associated with febrile reaction, urticaria, muscle weakness, pain and swelling or excessive bleeding at the injection site, and sterile abscesses.
Ethambutol (EMB) is associated with dizziness, headache, confusion, dermatitis, abdominal pain, anorexia, nausea, vomiting, joint pain and swelling, optic neuritis (loss of vision), and loss of visual acuity.
Ethionamide may produce severe postural hypotension (low blood pressure when a person suddenly stands or sits up), mental depression, rash, anorexia, diarrhea, epigastric distress, jaundice, nausea, and vomiting.
INH is one of the most frequently used drugs. It may produce many neurologic disturbances in sensation and vision, as well as variable changes in electrolytes. As with many drugs, nausea, constipation, epigastric distress, and vomiting are common. Severe and sometimes fatal hepatitis may develop, even after many months of treatment. The drug also changes the results of a variety of laboratory tests. Symptoms of overdosage may occur any time from 30 minutes to 3 hours after the INH is administered. Nausea, vomiting, slurred speech, dizziness, impaired vision, and visual hallucinations may be among the early symptoms. Severe overdosage results in CNS depression, respiratory distress, coma, and severe intractable seizures.
Pyrazinamide (PZA) has been associated with photosensitivity, rashes, diarrhea, hepatocellular damage, nausea, vomiting, gout, decreased blood clotting time, and anemia.
Rifampin (RIF) may cause drowsiness, headache, generalized numbness, transient low-frequency hearing loss, visual disturbances, abdominal pain or cramps, diarrhea, epigastric distress, hepatitis, nausea, sore mouth and tongue, vomiting, and changes in blood cells. Symptoms of overdosage include nausea, vomiting, increasing lethargy, unconsciousness, liver enlargement and tenderness, and jaundice. RIF also turns the urine a reddish-orange color.
SM sulfate may produce dizziness, headache, paresthesias (numbness or tingling), vertigo, anorexia, nausea, stomatitis, vomiting, changes in blood cells, arthralgia (joint pain), hypertension (high blood pressure), hypotension (low blood pressure), myocarditis, hepatotoxicity, splenomegaly (enlarged spleen), ototoxicity, and nephrotoxicity.
Drug Interactions
The drug treatment plan for TB is often complicated. No other drugs should be taken at the same time or right after antitubercular drugs are swallowed, or put on the skin while the patient is on antituberculosis therapy. This is because other drugs may increase the significant risk for neurotoxicity and nephrotoxicity. All drugs taken by the patient should be checked closely for drug interactions, which are very common among the antitubercular drugs.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
A TB infection may develop in a patient’s lungs, bones, bladder, or other organs. A patient with active TB may have symptoms such as productive cough, pain, fever, night sweats, and weight loss, or the patient may be without symptoms. The diagnosis of TB is made from the patient’s history, physical examination, x-ray studies, and laboratory work. A PPD skin test is not given if there is a high probability that the patient has TB. Once the diagnosis is made, the patient may be hospitalized while treatment is started. Long-term treatment is required, and much of the treatment will be carried out when the patient is at home.
n Diagnosis
Patients with TB often have needs for financial, nutritional, and career counseling that will interfere with them being treated. These other problems must be diagnosed and included in the treatment plan if the needs of the patient are to be considered. These individuals may have other medical problems and may be taking multiple drugs, resulting in additional problems with side effects and scheduling of dosages. The nurse must be prepared to help analyze all the needs of the patient if effective treatment is to be offered. In particular, watch to see if the patient is compliant, because treatment programs in which the patient is watched while taking the medication (directly observed therapy) may be required to protect the public from this disease.
n Planning
Drug resistance is likely to develop if only one drug is given for active TB. Two or more drugs should always be given to provide several ways to attach the TB bacterium. Drugs that are highly ototoxic should not be given together. Two hepatotoxic drugs should not be given together when clinically active hepatitis is present.
To prevent the development of drug resistance, be aware of the following:
The CDC Advisory Council for the Elimination of Tuberculosis has issued its recommendations for initial therapy of TB. The regimen for children and adults who do not have HIV infection is as follows:
• Use daily INH, RIF, and PZA and either EMB or SM sulfate for 8 weeks.
• EMB or SM can be added to the initial regimen if needed.
• Use INH and RIF daily or two to three times per week for 16 weeks or up to 6 months.
Directly observe the patient take the medication. The daily dose should be given in the morning before the patient eats or drinks anything else.
The therapy of choice for uncomplicated pulmonary TB is the use of two drugs, INH and RIF, which are both intracellularly and extracellularly bactericidal. The duration of therapy is usually a minimum of 9 months. Sputum that is cultured 1 to 3 months after the initiation of INH and RIF therapy will usually be negative for the bacillus. The therapy usually continues for 6 months after sputum conversion takes place. When necessary, the combination of PZA and SM sulfate may be used to substitute for either one of the bactericidal drugs described previously. However, there is some controversy over the effectiveness of this shorter, 9-month course of therapy when INH is not used.
At present, intermittent therapy with INH and RIF is being investigated. The American Thoracic Society recommends that these two drugs be given daily for 2 to 8 weeks. Then the patient is switched to twice per week for a total of 39 weeks. The minimum duration of therapy is 9 months. The daily dosage recommendations for adults are INH 300 mg and RIF 600 mg. The twice-weekly dosage plan for adults is INH 15 mg/kg of body weight and RIF 600 mg. The American Thoracic Society recommends intermittent therapy only for uncomplicated pulmonary TB. See the new CDC guidelines for treatment of patients with MDR strains whenever they are issued.
Whenever a combination of drugs does not have both an intracellular and an extracellular bactericidal effect, therapy must continue for the traditional 18 to 24 months. This usually occurs when bacteriostatic drugs are used.
For TB patients with HIV infections, use the previous treatment schedule, but continue treatment for 9 months beyond culture conversion.
Because of the long-term nature of the required treatment, drug toxicity is a special problem. Dosages for older adult patients, unusually small adults, and patients with renal impairment should be watched. All patients should be carefully asked about symptoms of adverse reactions. If toxic effects, adverse reactions, or allergic reactions occur, all drugs should be stopped, and further evaluation should be done. Restarting drugs after toxic effects or adverse reactions have ceased should be done with caution.
In the event of an unsuccessful treatment regimen, the health care provider will evaluate for patient compliance and the presence of an MDR strain. If the problem is patient compliance, the same treatment regimen can be started again. With an MDR strain, two or more new drugs are added to the regimen, never a single drug, because drug resistance may develop more easily with only one new drug. The drugs used for retreatment for an MDR strain include para-aminosalicylate, capreomycin, cycloserine, ethionamide, and kanamycin.
Guidelines for the treatment of TB are frequently updated by the CDC. To avoid problems with drug resistance, the latest information should always be used in treating patients.
n Implementation
Antitubercular drugs should be given in single daily doses unless contraindicated. All drugs, unless stated otherwise, should be taken at the same time each day, preferably in the morning. This is especially important to decrease the chance of drug resistance with the combination of INH and RIF. When poor compliance is suspected, the care provider should directly observe that the patient is indeed taking the drugs.
If parenteral administration is required, the injection sites should be rotated and each site inspected for signs of tenderness, swelling, or redness.
If a patient does not seem to be getting better, closer monitoring to make sure the patient is taking the medicine may be necessary.
Many of these drugs cause gastric irritation, which may be reduced by taking the medication with food. INH is the only antitubercular medication that is best absorbed on an empty stomach. It should be taken as a single daily dose either 1 hour before or 2 hours after a meal. It should be taken with food only if it cannot be tolerated on an empty stomach.
See Table 12-5 for a summary of common antitubercular drugs.
n Evaluation
Drug resistance should be suspected if the patient has been treated for TB in the past. Drugs used in the regimen for the earlier infection may be used again while waiting for the results of sensitivity studies, but at least two new drugs should also be added. Drug resistance is low in infections acquired in the United States but high in TB infections acquired from Asian, South and Central American, and African sources. Drug resistance is less likely to occur when two bactericidal drugs are given together, rather than when one bactericidal drug is given together with bacteriostatic drugs.
Vital signs should be monitored for recurrence of acute infection. Patients should be weighed at each visit to monitor their general health status. Weight loss should be reported to the physician or other health care provider. Diet changes and nutritional supplements may be indicated.
Some patients taking EMB develop psychologic changes. If the patient becomes depressed, anxious, withdrawn, or stops talking—or shows any changes in personality—these findings should be reported to the physician or other health care provider.
Because of marked toxicity of these drugs, it is essential to carefully and regularly monitor both the bacteriologic studies and the toxic side effects of the drugs. Baseline sputum smears, culture and sensitivity studies, chest x-ray studies, weight, and renal, hepatic, and hematopoietic studies should be obtained.
n Patient and Family Teaching
Because patients must take their drugs for a long time, it is important to establish a good relationship with the patient. Clear instructions should be given about the importance of continuing to take the drugs as ordered and what problems to report to the nurse practitioner, physician, or other health care provider at the scheduled visits. It is important to stress the following instructions:
Antiparasitic Drugs
Overview
Parasites affecting humans are a worldwide problem. Three major categories of drugs used to treat parasites are discussed in this section: amebicides, anthelmintics, and antimalarial products. Each major category is discussed in detail.
Amebicides
Action
There are a wide variety of parasites and thus a wide variety of drugs used to treat them. Amebiasis is often caused by the parasite Entamoeba histolytica. In the United States and Canada, this infection is seen primarily in people who have traveled abroad. It is also found in those who have eaten unwashed fruits or vegetables imported from other countries, so parasitic infection could be common. The main action of an amebicide is to destroy the invading amoeba, which may be located within the GI tract or some other place in the body (extraintestinal). Infections outside the intestinal tract are much more difficult to treat. The most common extraintestinal infection is a hepatic abscess.
Uses
Amebicides are the primary therapy for both intestinal and extraintestinal amebiasis. The choice of drug depends on the location of the infection.
Diiodohydroxyquin and metronidazole are also used to treat Trichomonas vaginali and giardiasis, which is commonly found in drinking water, particularly in other countries.
Adverse Reactions
All drugs used to treat amebiasis may cause nausea, vomiting, headache, anorexia, diarrhea, or GI distress.
Chloroquine may produce dizziness, irritability, pruritus, ototoxicity, tinnitus, vertigo, visual disturbances, or abdominal cramps.
Diiodohydroxyquin has been known to cause ataxia (poor coordination), neurotoxicity, peripheral neuropathy, optic neuritis, abdominal cramps, rectal and skin itching, constipation, and hair loss.
Paromomycin may produce vertigo, rash, ototoxicity, abdominal cramps, constipation, hematuria, and nephrotoxicity.
Symptoms of overdosage are also seen with all of these drugs and are an exaggeration and increase of the adverse effects.
Drug Interactions
With the exception of metronidazole, there are no significant drug interactions. Combining metronidazole with alcohol can produce severe headache, flushing, cramps, nausea, and vomiting. Collapse or acute psychosis may result.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including any allergy to drugs, current use of alcohol or disulfiram, the possibility of pregnancy, or the existence of chronic renal, cardiac, thyroid, or liver disease. These conditions are contraindications or precautions to the use of amebicides.
n Diagnosis
The nurse might consider asking the patient questions that would help uncover additional problems that might affect the diagnosis or treatment of the problem. For example, does this patient have problems with severe diarrhea that may produce dehydration? Are there knowledge deficits about handling, washing, and storage of fruits and vegetables? Are there other problems that limit the medication therapy for this patient?
n Planning
Four major drugs are used as amebicides. The contraindications for drug use are somewhat different, depending on the drug chosen. The specific product information should be consulted.
n Implementation
The drug to be ordered depends on the location of the infection. Some of these drugs are specific for extraintestinal infections. Because these drugs are very toxic, the decision to treat the patient should be carefully made, and only the smallest therapeutic dosage possible should be given for the shortest period. If the initial drug is ineffective and another drug is more hazardous, retreatment with the initial drug may be advised.
Teach the patient about the method of infection and review specific methods of personal hygiene to prevent reinfection and reduce the risk of spreading infection to others.
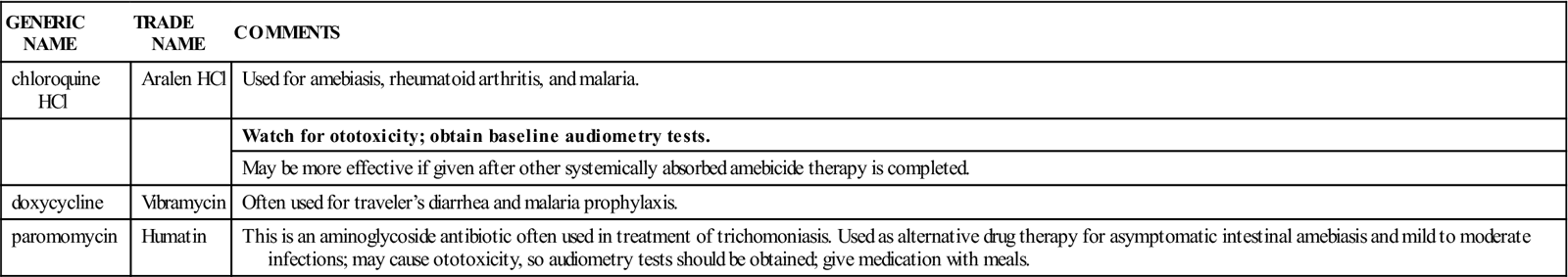
Table 12-6 provides a summary of amebicides.
![]() Table 12-6
Table 12-6
| GENERIC NAME | TRADE NAME | COMMENTS |
| chloroquine HCl | Aralen HCl | Used for amebiasis, rheumatoid arthritis, and malaria. |
| Watch for ototoxicity; obtain baseline audiometry tests. | ||
| May be more effective if given after other systemically absorbed amebicide therapy is completed. | ||
| doxycycline | Vibramycin | Often used for traveler’s diarrhea and malaria prophylaxis. |
| paromomycin | Humatin | This is an aminoglycoside antibiotic often used in treatment of trichomoniasis. Used as alternative drug therapy for asymptomatic intestinal amebiasis and mild to moderate infections; may cause ototoxicity, so audiometry tests should be obtained; give medication with meals. |
n Evaluation
After drug therapy, periodic stool tests will be required to make certain that the disease has been eliminated. These tests may be needed monthly for up to 1 year after therapy.
Be alert to signs of toxicity. If severe symptoms appear, the drug may have to be stopped.
n Patient and Family Teaching
Anthelmintics
Action
When a patient has worms, the infestation is called helminthiasis. The condition is usually caused by pinworms, roundworms, hookworms, tapeworms, or whipworms. The worm gains entrance to the body through unclean food, unwashed hands, or the skin. The diagnosis is made by finding the eggs or the parasite in the stool of the infected individual. Once the type of parasite has been identified, the health care provider may order the best medication for its destruction. The way the drug works depends on the product used.
The exact action of diethylcarbamazine citrate as an anthelmintic is not known. It is thought that it sensitizes the parasite’s cuticle to allow phagocytosis by the macrophages of the host. Mebendazole blocks the glucose uptake of helminths. Piperazine paralyzes the muscles of parasites by blocking the effects of acetylcholine at the neuromuscular junction, and the parasite is removed by normal peristalsis during the bowel movement. The exact action of thiabendazole is not known, but it is thought to interfere with metabolic pathways essential for a variety of helminths.
Uses
Thiabendazole is the drug of choice for cutaneous larva migrans (creeping eruption), pinworms, roundworms, Strongyloides, and mild cases of hookworm.
Niclosamide and paromomycin are used to treat cestodiasis (tapeworm infestation).
Piperazine and pyrantel pamoate are used to treat roundworms and pinworms. Pyrantel is also effective against hookworms.
Diethylcarbamazine citrate is used mostly in tropical areas or in patients who have been in areas where these worms are endemic. It is used to treat Bancroft filariasis, Malayan filariasis, dipetalonemiasis, or infestation with loiasis (a filarial worm dwelling in tumors in subcutaneous connective tissue and often affecting the eyes).
Mebendazole is used in single or mixed infections to treat pinworm, roundworm, hookworm, and whipworm infestations.
Adverse Reactions
Each drug has different side effects. Headache, weakness, anorexia, nausea, vomiting, abdominal pain, arthralgia, lassitude (weariness), malaise, myalgia (widespread muscle pain), and skin rash are all common reactions. Allergic reactions may occur as a result of the dead microfilaria and may be seen with fever, lymphadenitis (inflammation of the lymph nodes), pruritus, and pedal edema (foot swelling). The number of side effects increases with higher dosages and longer length of treatment.
Drug Interactions
Anthelmintic drugs work against each other (antagonistic) if they are given together. The drugs also may interfere with a number of specific drugs, such as heparin, and a variety of laboratory tests. Specific product information should be consulted for each drug.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including the presence of hypertension, allergy, eye disease, intestinal obstruction, inflammatory bowel disease, malaria, the possibility of pregnancy, and hepatic, renal, or cardiac disease. These conditions are contraindications or precautions to treatment with anthelmintics.
The patient may have no symptoms or may be listless, fatigued, and irritable or have abdominal pain, diarrhea, and weight loss. The patient may also have edema (collection of large amounts of fluid in tissues), especially of the lower extremities, and a discharge from the eyes. If helminthiasis is seen commonly in the area, learn the signs and symptoms of infestation by the various helminths.
n Diagnosis
The nurse might ask the patient questions to help determine if there are other problems that might influence the diagnosis or treatment of the problem. For example, has the patient developed skin lesions, dehydration, or other problems that require or would affect treatment? Is there lack of information that caused this problem? Are there teaching needs to prevent reinfection? Does the patient have other problems that would interfere with or limit therapy for this problem?
n Planning
Severe pruritus may occur in the treatment of cutaneous larva migrans, and an antiinflammatory agent may be necessary.
Patients with a recent history of malaria should be treated with an antimalarial agent before giving them anthelmintics to prevent a relapse.
Because pinworm infections are easily transferred from person to person, all family members may need to be treated.
Piperazine can be used in the last trimester of pregnancy. However, this drug has potential neurotoxicity, so long or repeated treatment in excess of the recommended dosage should be avoided, especially in children.
n Implementation
Thiabendazole therapy may cause an asparagus-like odor of the urine. The patient’s skin may also have an unusual odor. This medication may cause drowsiness or dizziness; therefore the patient should use caution in driving or doing tasks that require alertness.
Severe hookworm infestations may produce anemia, so iron supplementation and a diet rich in iron may be required.
The patient should store piperazine syrup and tablets in tightly closed containers to avoid evaporation or decomposition. Liquids are easier for children to take. Medication is usually given in the morning before breakfast.
Patients may develop allergic reactions to the dead microfilaria and may need treatment for symptoms. Antihistamines or corticosteroids may be necessary to reduce allergic effects, particularly in the treatment of ocular onchocerciasis.
Table 12-7 provides a summary of anthelmintics.
![]() Table 12-7
Table 12-7
| GENERIC NAME | TRADE NAME | COMMENTS |
| albendazole | Albenza | For treatment of lesions from pork or dog tapeworm. Give for <132 kg: 15 mg/kg/day in two divided doses for 28 days, followed by a 14-day cycle with no medications; repeat for two more cycles. For >132 kg: 400 mg PO twice daily with meals for 28 days, followed by a 14-day cycle with no medications; repeat for two more cycles. |
| ivermectin | Stromectol | For treatment of intestinal parasites and onchocerciasis. Give once. Usually no repeat dose needed. |
| mebendazole | Vermox |
No special diets, fasting, or purgation before administration is necessary. Medication is taken orally by chewing, crushing, or mixing with food. Given for pinworms, roundworms, hookworms, and whipworms. |
| praziquantel | Biltricide | Tablet very bitter if not swallowed promptly. |
| pyrantel | Reese’s pinworm Pin-X |
Medication can be administered as single dose for treating roundworms and pinworms; hookworms require longer therapy. No special fasting or diet necessary before taking medication. Purging not necessary. Taking drug with fruit juice or milk may make it more palatable Give for roundworm, pinworm, and hookworm therapy. |
| thiabendazole | Mintezol | Chew tablets well before swallowing. Take drug after meals. First line agent for cutaneous larva migrans and strongyloidiasis. Also given for pinworms, roundworms, and hookworms. |
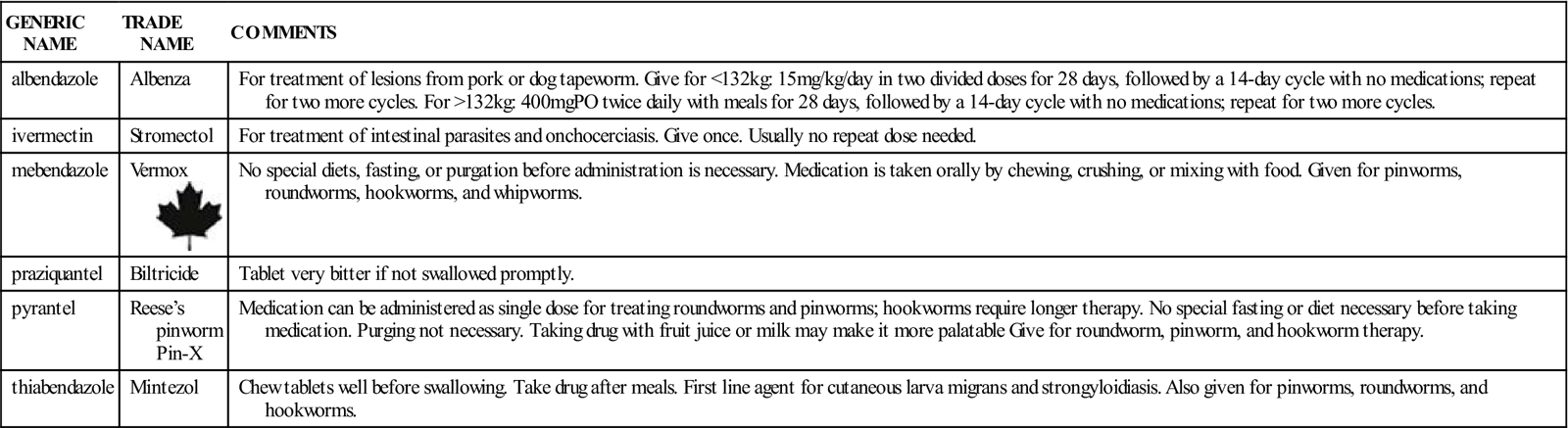
n Evaluation
Determine if the patient is taking prescribed medication as ordered and doing other things that might be part of the therapy. Collect stool specimens after every treatment to make sure the worms are gone. Check to see if the patient has had an ophthalmologic (eye) examination if currently undergoing treatment for ocular onchocerciasis.
Teach the patient the hygienic measures necessary to prevent reinfestation.
If the patient develops neurologic complications with piperazine therapy, this medication should be stopped, and another drug should be used.
n Patient and Family Teaching
Tell the patient and family the following:
• Worms passed in bowel movements are still alive and capable of infecting others. Care must be used to avoid transmission. For the week after treatment begins, the patient should do the following:
• Wash the toilet seat daily with soap and water.
• Once a week for 2 weeks, boil the sheets and underwear twice in water and disinfectant.
• Use special precautions in handling food or drink around others.
• Some people have diarrhea and abdominal discomfort while taking the medication.
• The patient may require iron supplements and an iron-rich diet during hookworm treatment.
Antimalarials
Action
Malaria is a big problem in many countries where wetlands provide a good breeding ground for mosquitoes. Patients with malaria have periods of acute sickness followed by periods during which they are symptom free. The antimalarial drugs suppress the infection but often do not cure it. Although malaria is not commonly seen in the United States or Canada, it is becoming more frequent in Florida, other areas of the southern United States, and areas adjoining Mexico. The nurse may also see cases among immigrants, migrant farm workers, and travelers returning from areas where malaria is endemic (occurs in a regular pattern). People in the military or those traveling to or living in areas where malaria is endemic can use antimalarials to prevent malaria and treat the symptoms.
Malaria is caused by four species of the protozoan Plasmodium. These species are P. falciparum, P. malariae, P. vivax, and P. ovale. The protozoan parasites are transmitted to humans by the Anopheles mosquito.
When a mosquito bites a person infected with malaria, the protozoans enter the mosquito’s stomach, where they reproduce. The resulting sporozoites make their way to the salivary glands of the mosquito. They are then transmitted to other individuals whenever the mosquito bites. The sporozoites grow and divide in the human host, entering the red blood cells of the person and maturing into the adult form of the protozoan, which then produces infection and the symptoms of malaria.
Antimalarial drugs interfere with the life cycle of Plasmodium, usually while it is in the red blood cells (Table 12-8). These drugs reduce the ability of the DNA to reproduce or serve as a template, thereby decreasing protein synthesis in susceptible organisms. Not all drugs are effective against all four species of Plasmodium. In addition, many strains of Plasmodium have developed resistance to commonly used drugs. The drugs used in treating malaria are not without risk, and the licensed practical or vocational nurse giving these drugs will need to study the drug information carefully.
![]() Table 12-8
Table 12-8
| GENERIC NAME | TRADE NAME | COMMENTS |
| Aminoquinolines | ||
| chloroquine HCl | Aralen HCl | Parenteral drug of choice for treating acute malarial attacks when oral therapy is ineffective. |
| Watch for ototoxicity; obtain baseline audiometry tests. | ||
| chloroquine phosphate | Aralen Phosphate | Used for malaria suppression and treatment. |
| hydroxychloroquine | Plaquenil | Malaria suppression and treatment. It is a synthetic antimalarial agent. Also used occasionally to treat rheumatoid arthritis and discoid lupus. |
| primaquine phosphate | Primaquine Phosphate | Initiate primaquine therapy following a course of chloroquine phosphate suppressive treatment or during the last 2 wk of therapy with chloroquine phosphate. |
| Folic Acid Agonists | ||
| pyrimethamine | Daraprim | Malaria suppression: |
| Synthetic antimalarial. Used in combination therapy for chloroquine-resistant Plasmodium falciparum. Therapy should begin 2 wk before entering malaria-endemic area and be continued for 10 wk after departure. | ||
| Miscellaneous Agents | ||
| doxycycline | Doxycycline | Used for malaria prophylaxis. |
| mefloquine | Lariam | Prevention and treatment of malaria. |
| quinine sulfate | Quinamm | This was formerly used for treatment of malaria. Now used primarily for nocturnal leg cramp treatment. |
| Nonmalarial Antiprotosoals | ||
| atovaquone | Mepron | Antiprotozoal agent also used for Pneumocystis. |
| metronidazole | Flagyl MetroGel | Drug of choice in mild to severe intestinal amebiasis and treatment of hepatic abscess; effective against protozoa such as Trichomonas vaginalis, amebiasis, and giardiasis. Has been used as combination therapy in treating Helicobacter pylori GI infection. |
| Metronidazole may cause changes in the ECG findings, ataxia, confusion, depression, insomnia, irritability, vertigo, flushing, pruritus, blurred vision, nasal congestion, abdominal cramps, constipation, dysuria (painful urination), polyuria (excretion of a large amount of urine), pyuria (increased white blood cells in the urine), fever, and metallic taste. Alcohol must be avoided as it produces severe vomiting reactions which may be life-threatening. | ||
| nifurtimox | Lampit | The drug of choice for American trypanosomiasis |
| pentamidine | NebuPent, Pentam 300 | For Pneumocystis carinii infections and prophylaxis. Available in both inhalation and IM forms. |
| sodium stibogluconate | Pentostam | For leishmaniasis |
| suramin | Germanin | Drug of choice for African trypanosomiasis. |
| Trimetrexate | Neutrexin | Alternative therapy for Pneumocystis carinii pneumonia. |
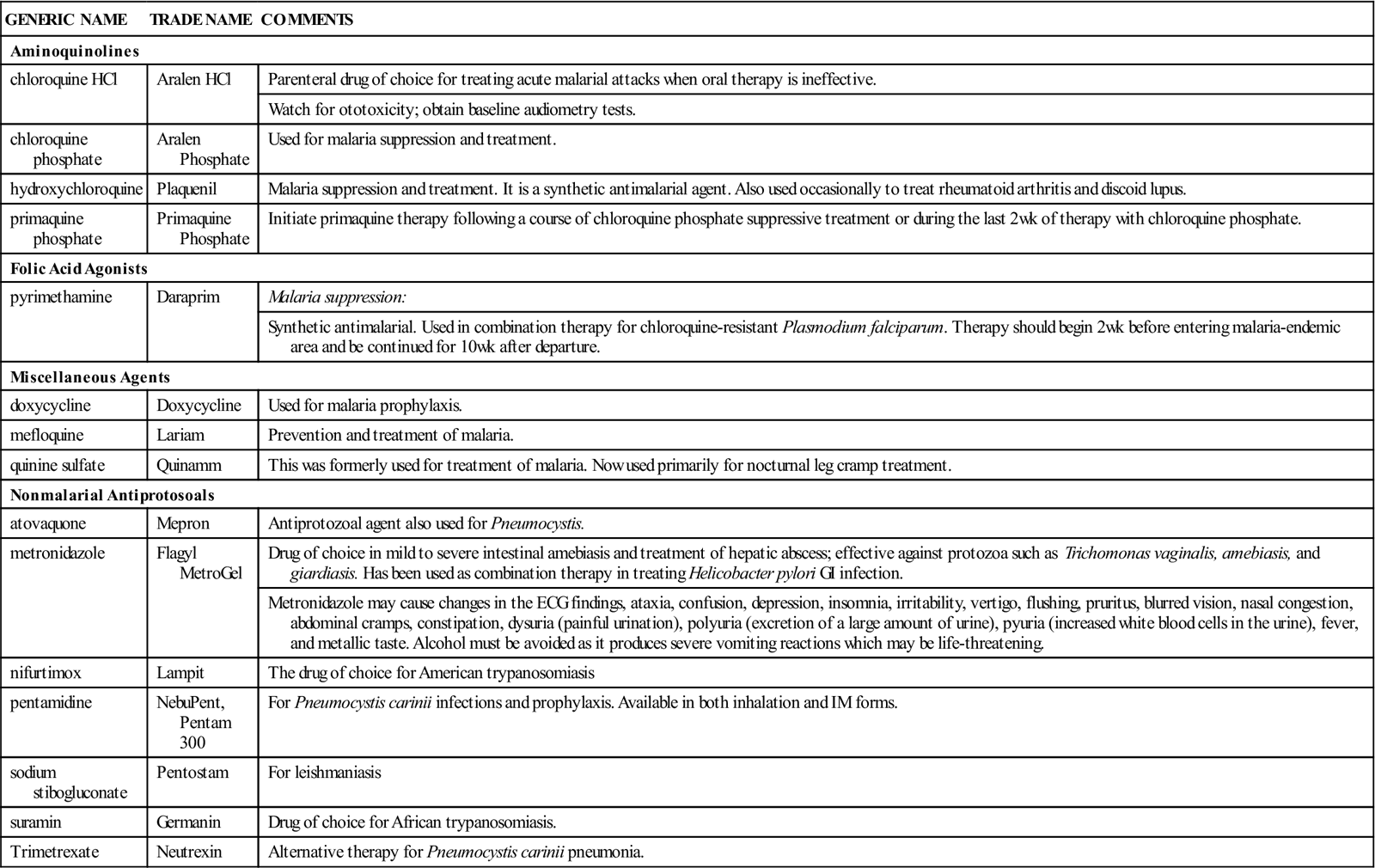
ECG, Electrocardiogram; GI, gastrointestinal; IM, intramuscular; PO, by mouth.
Primaquine interferes with the metabolism of parasites. Folic acid antagonists affect the differential growth requirements and the demand for nucleic acid precursors between the host and the parasite. In sulfonamide products, there is a competitive antagonism of paraaminobenzoic acid, which is a component in folic acid synthesis. Quinine, the earliest known medication for malaria, reduces the effectiveness of Plasmodium’s DNA to act as a template in chloroquine-resistant strains of P. falciparum. It also decreases the parasite’s oxygen use and carbohydrate metabolism. In the human body, quinine is a skeletal muscle relaxant, antipyretic, and analgesic.
A variety of other protozoals also exist, including American and African trypanosomiasis, leishmaniasis, and Pneumocystis carinii. A variety of other antiprotozoal medications may be used in treatment of these problems.
Uses
Antimalarials are used to suppress and treat acute malaria attacks caused by erythrocytic forms of P. ovale, P. malariae, P. vivax, and most strains of P. falciparum. The 4-aminoquinoline drugs are ineffective against the gametocytes of P. falciparum but are used with primaquine to cure malaria caused by P. malariae and P. vivax.
Adverse Reactions
Synthetic 4- and 8-aminoquinolines may produce hypotension, electrocardiogram (ECG) changes, mild and transient headaches, pruritus, abdominal cramps, anorexia, diarrhea, nausea, vomiting, blood dyscrasias, visual blurring, reduced hearing, and tinnitus.
Folic acid antagonists may produce anorexia, atrophic glossitis (loss of papillae of the tongue), vomiting, and anemias.
Quinine poisoning is called cinchonism and causes diarrhea, dizziness, headache, nausea, tinnitus, visual blurring, fearfulness, confusion, excitement, hypothermia (abnormally low body temperature), syncope (light-headedness and fainting), abdominal cramps, vomiting, anemias, pruritus, rash, urticaria, and night blindness.
All of these drugs may sometimes produce blood dyscrasias, as well as visual and neurologic changes. Overdose may produce convulsions and cardiac collapse.
Drug Interactions
Use of any antimalarials with other drugs that cause dermatologic, ototoxic, or neurologic symptoms may produce toxicity. There are isolated drugs that interact with these preparations, so read the manufacturers’ information carefully.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the patient’s health history, including whether the patient is pregnant or has a history of allergy, psoriasis, porphyria, or glucose-6-phosphate dehydrogenase deficiency. These conditions are contraindications or precautions to the use of antimalarials.
The symptoms of malaria include periodic fever and chills, profound sweating, headache, nausea, body pains, and exhaustion. The patient may report having been in an area where malaria is endemic. Objective signs of malaria include periodic diaphoresis (sweating) and periodic cycles of fever as high as 104° to 105° F.
n Diagnosis
Ask the patient questions to determine if there are other relevant problems that would affect the diagnosis and treatment of this problem. Is the patient dehydrated? What is the patient’s state of nutrition? Are there other chronic diseases or problems that may interfere with this therapy? Is the patient taking other medications?
n Planning
Because certain strains of P. falciparum are resistant to 4-aminoquinoline compounds, individuals infected with these strains should be treated with other antimalarial drugs such as quinine.
Individuals taking high dosages or going through prolonged antimalarial therapy may develop irreversible retinal damage to the eyes. Children are highly sensitive to 4-aminoquinoline compounds, primarily chloroquine.
Quinine should be used with care in patients with cardiac dysrhythmias. Cardiotoxicity may result with quinine use. In very sensitive individuals, reversible thrombocytopenia may occur with quinine use.
Laboratory work to measure the glucose-6-phosphate dehydrogenase level in all black patients and in those of Mediterranean ancestry may be required; antimalarial drugs may precipitate hemolysis in some vulnerable patients. The drug should be stopped if the patient develops any blood dyscrasia that is not part of the disease.
n Implementation
Chloroquine phosphate and hydroxychloroquine are administered orally. To treat malaria, an initial loading dose is usually followed by half that dose on the next 2 days. To prevent malaria, these drugs are usually started 2 weeks before the individual enters an area where malaria is endemic. The medication is taken once weekly on the same day of the week and is continued for 8 weeks after the individual has left the area.
n Evaluation
Watch for the malaria symptoms to go away. If the patient requires long-term therapy, periodic complete blood cell count and urinalysis should be monitored. Check for signs and symptoms of hemolysis. An ECG may be obtained before starting quinine therapy and again during treatment if the patient develops any cardiac rhythm problems. Any report of visual problems makes a full eye examination necessary.
n Patient and Family Teaching
Tell the patient and family the following:
• The patient should take all the medication as ordered and not stop when the symptoms disappear.
• This medication is particularly toxic and should be kept out of the reach of children.
• Quinine products may cause the skin to appear somewhat yellow.
• Quinine may cause dizziness and blurred vision. The patient should be very careful when driving.