CASE 12
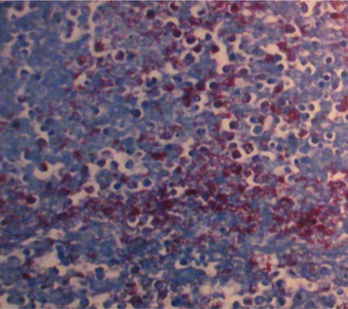
George, a frequent visitor to your emergency department, is generally in a state of total intoxication. He is 55 years old and has lived on the streets for as long as you can remember. In winter he stays overnight in a local shelter. When you see him tonight he looks quite ill and has obviously lost a significant amount of weight compared with when you saw him last (˜2 to 3 months ago). He admits he has chronic night sweats and a persistent cough with some whitish-yellow sputum. He has no history of diabetes, and indeed his blood sugar, even now, is within the normal range of 5 to 8 mmol/dL. He is unaware of any obvious acute presentation of a febrile illness and admits to a general lethargy over the past 2 to 4 weeks. There is no history of travel out of the city (including to local farms). He is currently afebrile but certainly does not look well. Blood work is unremarkable, with the exception of a modest increase in neutrophils. His chest radiograph shows significant consolidation in the lower lobes and evidence of an infectious process (inflammation) in the upper zones also (Fig. 12-1). In room air, his oxygen saturation is only 89% (normal 97% to 100%), and he is not a cigarette smoker.
QUESTIONS FOR GROUP DISCUSSION
RECOMMENDED APPROACH
Implications/Analysis of Clinical History
Malignancy, autoimmunity, or a chronic infection could help explain this symptomatology.
The weight loss/night sweats and cough would be consistent with a malignancy such as a lymphoma. It is unlikely that he has an HIV infection because there is no evidence of intravenous drug use, homosexual behavior, or previous transfusions. You should, however, confirm that these are not considerations.
THERAPY
Therapy consists of a multi-drug regimen for 6 to 12 months determined by susceptibility testing of initial isolates. Of concern is the fact that drug-resistant tuberculosis is increasing in prevalence. Unfortunately, patient noncompliance contributes to the emergence of drug-resistant strains of M. tuberculosis. Given this reality, two questions arise: Should George’s therapy be supervised? What should you do in the face of noncompliance, which will surely be the case with this patient? Some of these issues may not be relevant in the future in that a phase 1 clinical trial to test the efficacy of a recombinant tuberculosis vaccine with 20 volunteers will begin in the United States this year.
ETIOLOGY: TUBERCULOSIS
Tuberculosis is a chronic disease resulting from infection with M. tuberculosis (see Fig. 12-1). Most infections are acquired by inhalation of airborne droplets containing the organism. Phagocytosis by alveolar macrophages is the first line of cellular defense.
Host Response
Phagocytes play a central role in host defense to M. tuberculosis. Recognition may be indirect (opsonin mediated) or direct (e.g., TLR-2 and TLR-4; see Case 7). Phagocytosis of M. tuberculosis by alveolar macrophages results in the formation of a phagosome, a vesicle that is normally the site of microbial destruction (see Case 6). Included in the host defense armamentarium are lysosomal enzymes, reactive oxygen intermediates, and nitric oxide. M. tuberculosis has evolved immunoevasive strategies, however (see later), that allow it to thrive in the phagosome.