CASE 118


History: A 62-year-old woman presents with abdominal pain that is worse on the right.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in the figures? (Choose all that apply.)
2. Which of the following statements regarding the epidemiology of typhlitis is true?
A. Mortality rate of nearly 50%
B. Predominantly affects female patients
C. Increased risk with increased age
D. Most commonly recognized in patients with lymphoma
3. Which of the following statements regarding the investigation of typhlitis is true?
A. If typhlitis is suspected, colonoscopy is warranted.
B. CT is the most sensitive modality to detect typhlitis.
C. Barium enema is useful to assess extent of disease.
D. The presence of pneumatosis makes typhlitis unlikely.
4. Most inflammatory diseases of the colon demonstrate bowel wall thickening on cross-sectional imaging such as CT. Which is the exception?
ANSWERS
CASE 118
Typhlitis of the Cecum
1. A, B, D, and E
2. A
3. B
4. C
References
Cronin TG, Calandra JD, Del Fava RL. Typhlitis presenting as toxic cecitis. Radiology. 1981;138:29–30.
Thoeni RF, Cello JP. CT imaging of colitis. Radiology. 2006;240:623–638.
Vowels M. Typhlitis: neutropaenic colitis. Australas Radiol. 1988;32:477–479.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 313.
Comment
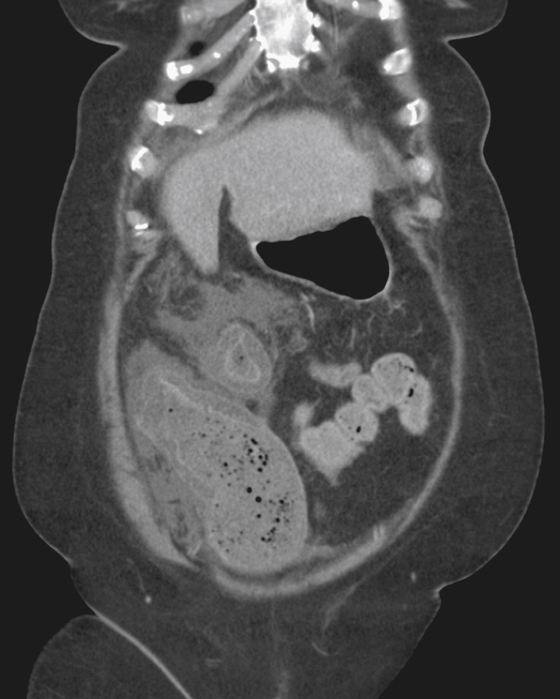
Neutropenic colitis, or typhlitis, is an inflammatory condition of the right side of the colon that occurs in patients undergoing treatment for leukemia, lymphoma, and sometimes other malignancies. Typically this condition affects the pediatric population, but in some instances it is encountered in the adult population. The clinical findings include fever, abdominal pain, and sometimes diarrhea. CT is the diagnostic modality of choice, demonstrating thickened bowel wall (sometimes with pneumatosis) and pericolic inflammatory changes in the mesenteric fat (see figures). These changes in the bowel are the result of a combination of edema, hemorrhage, and inflammatory exudate. Neoplastic involvement is not a feature of the disease.
The history of a compromised immune system immediately makes neutropenic colitis the primary diagnostic consideration. Interestingly, the treatment of neutropenic colitis is primarily aggressive antibiotic treatment. Surgery is necessary only for patients with obvious perforation and abscess development. Most patients respond well to antibiotics and supportive treatment and do not require surgery.







