CASE 116
History: A 41-year-old woman presents with abdominal pain.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in the figures? (Choose all that apply.)
2. Which of the following complications of acute pancreatitis usually develops early in the course of the disease?
3. What is the most definitive means to diagnose benign focal pancreatitis in differentiation from pancreatic carcinoma?
4. Contrast-enhanced CT is the standard imaging modality for evaluating acute pancreatitis and its complications. Which of the following is a contraindication to the performance of a contrast-enhanced CT?
C. Allergy to intravenous contrast
D. When cholelithiasis has not been excluded as the underlying cause
ANSWERS
CASE 116
Unusual Presentation of Acute Pancreatitis
1. A, C, D, and E
2. B
3. D
4. C
References
Balthazar EJ, Freeny PC, van Sonnenberg E. Imaging and intervention in acute pancreatitis. Radiology. 1994;193:297–306.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 154.
Comment
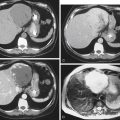
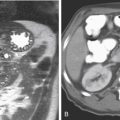
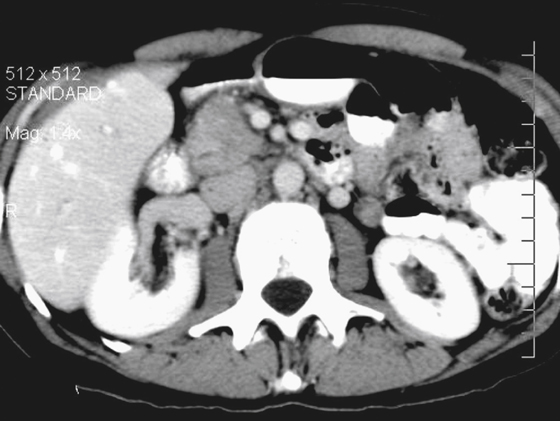
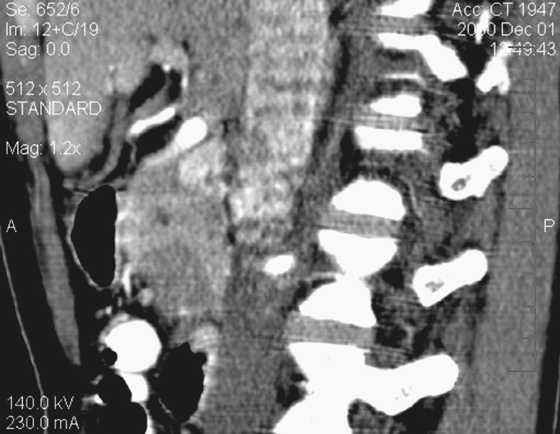
Acute pancreatitis has a variety of imaging presentations, including disease seemingly limited to the pancreatic head, as seen in this case. In most cases, more of the gland is involved with edema, and hemorrhage and necrosis occur in a few patients. Necrosis and sepsis constitute the leading causes of death in acute pancreatitis.
Most acute pancreatitis involving the pancreatic head can have a very adverse effect on the biliary system, compressing the common bile duct just as a pancreatic malignant mass might. However, that is not always the case, as with this patient. These lesions always present a dilemma and are often biopsied to rule out carcinoma. About 25% to 30% of all cases of pancreatitis manifest with findings limited to the pancreatic head (see figures). Gallstones passing through the shared ampulla of Vater can also give rise to inflammatory changes in the pancreatic head as well as throughout the entire gland. The stone does always have to be present. Some stones lodge, cause havoc with pancreatic drainage, and then pass. More than 80% of patients with gallstone pancreatitis have stones detected in stool. However, most of these have accompanying bile duct obstruction and some degree of distal pancreatic duct obstruction. In this case, the lack of biliary involvement and the normal distal pancreas suggest an inflammatory origin. A calcification in the ampulla of Vater would seal the diagnosis.
In rare instances, pancreatic carcinoma manifests as acute pancreatitis. When there is no etiologic basis for acute pancreatitis in a middle-aged or older adult, cancer is a consideration.