CASE 113



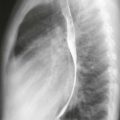
1. What are potential etiologies of the abnormality seen on the frontal radiograph? (Choose all that apply.)
A. Lymphoma
B. Lung cancer
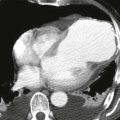
2. Based on the CT scan, which portion of the aorta is most abnormal?
A. Ascending
B. Arch
C. Descending
D. Abdominal
3. What is the most likely diagnosis of the arch abnormality?
4. What is the most likely etiology?
A. Trauma
C. Infection
ANSWERS
Reference
Reddy GP, Gunn M, Mitsumori LM, et al. Multislice CT and MRI of the thoracic aorta. In: Webb WR, Higgins CB, eds. Thoracic imaging: pulmonary and cardiovascular radiology. ed 2 Philadelphia: Lippincott Williams & Wilkins; 2010.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 377–379, 398.
Comment
Etiology and Pathology
Etiologies of an aortic pseudoaneurysm include atherosclerosis (penetrating aortic ulcer), infection, trauma (deceleration injury), and iatrogenic injury. Pseudoaneurysms are characterized by disruption of one or more layers of the vessel wall, whereas true aneurysms have intact walls. A nonsyphilitic infection of the aortic wall with aneurysm formation is called a mycotic aneurysm and is most commonly seen in patients with aortic wall damage (i.e., in a setting of trauma, endocarditis, or drug abuse). Pathogens most commonly responsible for mycotic aneurysms include Streptococcus, Staphylococcus, Pneumococcus, and Salmonella species. Mycobacterium tuberculosis can affect the aorta by contiguous spread from infected lymph nodes or the spine.
True and False Aneurysm
In a true aneurysm of the aorta, all three layers of the aortic wall are intact. In contrast, a false aneurysm results from a focal disruption of one or more layers of the aortic wall and may be contained by the adventitia and surrounding fibrous tissue.
Imaging
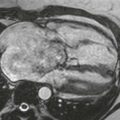
CT and MRI are the best imaging methods for evaluation of a thoracic aortic aneurysm. Disruption of the wall is difficult to identify by imaging examination. However, many observers use a rule of thumb: a relatively narrow ostium (<50% of the aneurysm diameter) suggests that the outpouching is a pseudoaneurysm, and a wide ostium suggests a true aneurysm. Most mycotic aneurysms have a saccular configuration, may contain peripheral thrombus, and can grow rapidly. There may be periaortic fat infiltration from associated inflammation. The case shown is atypical for mycotic aneurysm because the saccular outpouching has a relatively wide neck (Figs. A–C).