CHAPTER 112
Repetitive Strain Injuries
Definition
Repetitive strain injury (RSI) describes nonspecific upper extremity pain that often develops in occupational settings. RSIs are thought to result from the performance of repetitive and forceful hand-intensive tasks. These conditions are also referred to as cumulative trauma disorders, occupational overuse syndromes, and nonspecific work-related upper limb disorders. The varying nomenclature is controversial because it provides little insight into anatomy affected, disease severity, appropriate treatment, or expected prognosis. Classification systems of work-related musculoskeletal disorders often include specific diagnoses, such as carpal tunnel syndrome and de Quervain tenosynovitis, as RSIs, but the consensus in recent years has been to consider RSI an entirely separate category of occupational disorder [1]. RSIs have symptom complexes that do not fit neatly into another diagnostic classification, such as specific tendinopathy or nerve entrapment. RSIs typically have few objective physical findings and little in the way of demonstrable pathologic change.
RSI is a significant medical concern; approximately 65% of reported cases of occupational illness are attributed to repeated trauma annually [2,3]. In fact, occupational musculoskeletal disorders of the hand and wrist are associated with the longest absences from work and have greater lost productivity and wages than those of other anatomic regions [2]. There is evidence that this condition is actually underreported [4]. Important risk factors appear to be repetitive motion of the arm or wrist, movements that require extremes of hand or arm position, prolonged static postures, and vibration. Other risk factors may be poor ergonomic work environment, task invariability, lack of autonomy, and high levels of psychological distress in the workplace. In addition, the female gender appears to be more susceptible to development of RSI [5]. RSIs can develop outside of the workplace in individuals who participate in hobbies or activities that expose them to repetitive motion and prolonged postures on a consistent basis. A study demonstrated that the adult acquired upper limb amputee population is at increased risk of musculoskeletal pain in the neck/upper back and residual limb as well as in the contralateral remaining arm [6].
According to the U.S. Department of Labor, Bureau of Labor Statistics, occupations that appear to be at greatest risk for RSIs are those in the service and manufacturing industries, including any job involving computer processing and keyboard use [2]. These occupations have the most demand for upper extremity intensive tasks. Because of limitations in the assessment of risk factors, quantitative levels of exposure that are “acceptable” in each occupation are not available [7]. Clinically, it appears that the onset and perpetuation of RSIs are multifactorial. There is no proven etiology of RSI, but it is thought to develop from repetitive microtrauma to muscle, tendon, nerve, loose connective tissue, or bone that exceeds the ability of the tissue to heal itself. In animal models, when chronic repetitive motion is induced, an acute inflammatory response is stimulated in the tissue. This initial response eventually subsides and is followed by a fibrotic response that may lead to complete tissue repair if loads and repetition are sufficiently low [8]. However, in the presence of high repetition or high force, the acute inflammatory response is followed by tissue degeneration and fibrosis that leads to scarring. It is this tissue reorganization that may lead to a nonspecific pattern of pain in RSI.
Abnormal muscle fatigability may also contribute to pain [9]. Reduction in muscle blood flow and localized tissue hypoxia have been demonstrated in trapezius muscle biopsy specimens taken from assembly-line workers with prolonged, static shoulder postures who developed chronic trapezius myalgia [10]. In addition, diminished local muscle oxygenation and blood flow has been demonstrated in the forearms of individuals with RSI during static contraction, compared with controls at similar working intensities [11]. The same investigators later demonstrated that patients with RSI have an attenuated exercise-induced brachial artery blood flow and an impaired vascular endothelial function in the affected arm [12]. A subsequent study found that blood flow and oxygen consumption after exercise are similarly attenuated in both the affected and contralateral unaffected arms of patients with unilateral RSI, indicating that systemic vascular adaptations may occur [13]. These findings indicate that the underlying vasculature may be impaired in this condition. It is unclear whether these data can be extrapolated to explain the pathophysiologic mechanism of all RSIs in the upper extremity.
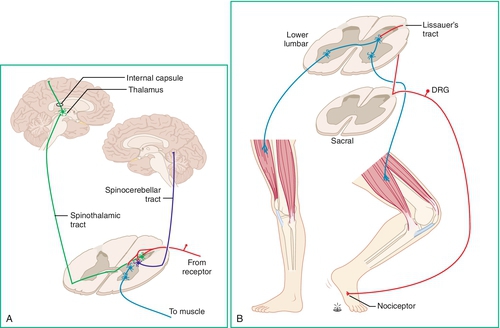
There may also be a neurogenic origin for RSI. There is evidence of neural reorganization at multiple levels of the central nervous system after the performance of repetitive tasks [2]. The repeated stimulation of nociceptive afferent nerve fibers may cause the receptors to become hypersensitive, to expand their receptive fields, and to increase the excitability of secondary neurons in the spinal cord. These changes may contribute to the hyperalgesia associated with chronic pain in RSIs. Moreover, there may also be an element of central nervous system reorganization at the level of the somatosensory cortex with repetitive tasks [2]. Figure 112.1 illustrates the distribution of somatosensory pathways in the central nervous system.
Regardless of the factors that contribute to the development of RSI, there is often a complex dynamic in managing patients with work-related musculoskeletal disorders. They are often involved in compensation claims. When the injured patient takes on the additional role of claimant, the perception of both patient and caregiver can change in many aspects of the healing and rehabilitation process. It is paramount for the physician treating RSI to take the medicolegal implications into account. Indeed, the workers’ compensation system has a great impact on the reporting and control of work-related disorders [14].
Symptoms
The predominant symptom in RSI is upper extremity pain. The discomfort often begins as a dull ache in the forearm or hand after the performance of tasks of repetitive motion. Initially, it may be intermittent and alleviated with rest. As the offending activity is repeated with regularity, the pain may increase in intensity and be triggered by minimal exertion in the workplace and even while performing simple activities of daily living, such as dressing or grooming. The symptoms usually begin in one region of the limb in a fairly localized area (e.g., wrist, elbow, or forearm) but may quickly spread to involve the entire arm and at times the contralateral arm. Pain tends to gradually increase during the workday, with peak intensity during the last hours of work. It appears to get better over the weekends and during vacations from work.
Other symptoms may include paresthesias, numbness, and weakness. If these symptoms are present, they may not follow dermatomal or peripheral nerve distributions. Patients may also complain of arm or hand muscle cramping, allodynia, stiffness, and slowing or incoordination of fine motor movements of the hand.
Patients often complain of night pain, resulting in poor sleep. A detailed investigation of sleep habits is important because sleep disruption is common in RSI. Psychological distress and depression may result if pain and sleeplessness persist. In fact, self-reported upper extremity–specific health status measured by the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire appears to correlate with depression and pain anxiety in these patients [15]. Some patients may also exhibit maladaptive illness beliefs, such as catastrophizing and fear-avoidance.
In taking a patient’s history, the clinician should attain an accurate understanding of the patient’s job description and daily workstation. It is important to thoroughly evaluate the biomechanics of body position and posture as well as the physical layout of the work site. Special attention should be given to the details of specific job duties, including the frequency, duration, and conditions under which they are performed. For example, if the patient works a desk job and spends each day on a computer, it is important to inquire about desk and chair setup and placement of the computer monitor and keyboard. The clinician should also take note of the patient’s perception and satisfaction with the workplace. This information can give the clinician valuable insight as dissatisfied workers are notorious for work-related medical claims.
Physical Examination
RSI is a diagnosis of exclusion. Typically, there are no objective physical findings. Hence, the physical examination should be comprehensive and focus on ruling out alternative diagnoses. It should include a thorough musculoskeletal examination with inspection, palpation, and testing of passive and active range of motion of the cervical spine, shoulder, elbow, wrist, and fingers. There is typically no evidence of muscle atrophy or other deformity. There may be pain on active and passive range of motion, but there is generally no restriction of motion when the examiner takes the joint through a full arc. There may be diffuse myofascial pain with palpation over the symptomatic region. In addition, there may be evidence of one or more focal fibromyalgia tender points on the symptomatic as well as on the asymptomatic side [16] (Fig. 112.2).

Neurologic assessment can rule out localized nerve disease by investigating for dermatomal, myotomal, or peripheral nerve abnormalities. In RSI, deep tendon reflexes are normal and symmetric. Manual muscle strength testing should be performed but is generally inconsistent, depending on the patient’s effort and pain level with exertion. Objective and reproducible strength tests can be performed with a hand or pinch dynamometer if level of strength is uncertain with examiner resistance. Computer-driven isokinetic dynamometers can also be used for more reliable measures of strength across uniaxial joints, such as the elbow. Sensory testing should be done by light touch as well as by pinprick. This portion of the neurologic examination is often difficult as subjective abnormalities are common. The reported impairments in sensation do not typically follow dermatomal distributions.
Provocative tests that reproduce specific pain patterns can help rule out alternative diagnoses. Examples include the Spurling test for cervical radiculopathy, Neer and Hawkins maneuvers for rotator cuff impingement, resisted wrist or finger extension for lateral epicondylitis, Tinel sign at the ulnar groove for ulnar neuritis, and Finkelstein test for de Quervain tenosynovitis. Provocative maneuvers that can rule out carpal tunnel syndrome include Tinel sign at the wrist, Phalen test, reverse Phalen test, and carpal tunnel compression. It is important to keep in mind that percussion over the median nerve at the wrist, the ulnar nerve at the cubital tunnel, or the radial nerve at the elbow may elicit pain or paresthesias in RSI, but this is not necessarily indicative of nerve injury.
Functional Limitations
RSI can limit upper extremity function to highly variable degrees [17]. Patients may have difficulty in performing activities of daily living at home, such as dressing, grooming, or preparing a meal. The pain impairment may prevent them from participating in recreational activities that they formerly enjoyed. They can also be quite limited in terms of their work-related activity. For example, pain may prevent a patient from being productive at work because he or she finds it difficult to use a keyboard and computer to do different tasks. Employers often advocate functional capacity evaluations to define more objectively the amount of physical labor that the patient can perform safely.
Diagnostic Studies
Diagnostic tests are ordered if the diagnosis is not clear after the history and physical examination, if the results of the testing will change management, or if the testing is needed for medicolegal reasons. The tests are used to exclude other definitive conditions that may remain in the differential diagnosis after examination. Needle electromyography and nerve conduction studies are often necessary to rule out a peripheral nerve lesion, such as median nerve entrapment at the wrist. Electrodiagnostic studies provide the distinct advantage of offering objective data by quantifying the degree of nerve impairment in a manner that is independent of the patient’s pain behaviors [18]. This can be important when injured workers have interest in substantial secondary gain and may not be reliable in their effort or honesty when motor and sensory nerve function is tested on physical examination.
Imaging is likely to be normal in RSI. Plain radiographs of the suspected site of disease will generally not reveal a fracture in the absence of blunt trauma but may reveal underlying degenerative changes that may or may not account for the patient’s symptoms. Magnetic resonance imaging of the cervical spine and shoulder is often ordered to rule out disc herniation, neuroforaminal stenosis, and rotator cuff disease. This study may be useful only if there is concern for one of these diagnoses on the basis of the physical examination [19]. Magnetic resonance imaging is expensive, and abnormalities such as disc bulging and degenerative spondylosis are often found in asymptomatic individuals and may not explain the current symptom complex.
Laboratory work is seldom necessary at the time of initial evaluation unless an underlying systemic illness is suspected.
Treatment
Initial
Treatment of RSIs should focus on conservative measures. The first step is to limit exposure, if possible, to the particular repetitive activities that may have contributed to the development of the RSI and that continue to induce pain. Whenever possible, accommodations at the workplace should be optimized to allow the patient to continue to perform the duties that are required by the employer. Several strategies for computer-based occupations are discussed later in this chapter. Early return to work with transitional arrangements should be facilitated when necessary. Sick leave should be avoided because it may develop into chronic disability. A substantial proportion of workers experience additional injury-related absences even after their first return to work. Time off work has proved to be a powerful predictor of disability pension; fully following work-related restrictions can ensure that the patient remains a productive employee by going to work [20].
Unfortunately, there is little evidence for the effectiveness of any specific medical intervention for RSI. Clinical treatment is usually targeted at relief of pain and acute inflammation as well as restoration of range of motion. Inflammatory conditions are often treated with the PRICE regimen: protection (preventing further injury, perhaps by bracing), rest or activity modification (as mentioned before), ice, compression, and elevation to minimize swelling.
Icing of the limb for about 20 minutes three times daily in conjunction with wrist or elbow splinting can decrease symptoms. Other modalities that may be helpful in controlling pain symptoms in the acute phase of treatment include ultrasound, iontophoresis, and transcutaneous electrical nerve stimulation applied to the region of soft tissue pain. Manual therapy, spray and stretch techniques with a vapocoolant spray, and paraffin baths may also alleviate pain in some patients, although evidence for efficacy is lacking.
Medications may also be used to control pain and inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) are usually the first-line pharmaceuticals for acute inflammation. There are many NSAIDs on the market from which to choose, and some can easily be purchased over-the-counter. It is often useful to try several different types of NSAIDs because patient responses can be idiosyncratic. Anticonvulsant medications, such as gabapentin, pregabalin, and carbamazepine, are also often used for pain. They are generally most effective for neuropathic pain. There is currently no evidence suggesting that they are specifically indicated in treatment of RSI. Local anesthetic patches (e.g., lidocaine) may be helpful if they are placed over a localized area of arm pain. Trigger point injections with local anesthetic or dry needling can also be considered to relieve myofascial pain. Oral narcotics are generally avoided.
Restoration of sleep can be helpful in reducing pain perception as well as in decreasing the risk for development of depression. The use of low-dose tricyclic antidepressants (e.g., nortriptyline or amitriptyline) can be effective. A randomized controlled trial found that low-dose amitriptyline did not significantly decrease arm pain compared with placebo among participants with RSI. However, low-dose amitriptyline did significantly improve arm function and well-being [21]. In addition, the antidepressant duloxetine that is indicated for treatment of fibromyalgia pain may be also be considered for treatment of pain associated with RSI. If signs of depression are present, appropriate comprehensive treatment and referral to a psychiatrist or psychologist may be indicated.
Rehabilitation
The rehabilitation of a patient with RSI is best achieved by a multidisciplinary approach with the physician overseeing the treatment plan and following the progress of the patient. A review of evidence-based management strategies suggests that biomedical treatment should not be ignored, but the psychosocial management approach appears to be more influential for occupational outcomes [22]. A referral to skilled physical and occupational therapy is essential [23]. Therapists may provide several therapeutic modalities (mentioned previously) to decrease pain and to facilitate an active stretching and strengthening program. The focus is not only on the affected limb but also on total body biomechanics and postural control at the workstation and at home. Progressive resistive exercise programs can be used, but worsening of pain symptoms with increasing exertion is often an issue. Progressive resistive exercises may have more benefit if they are introduced with small increments in resistance, allowing the patient to slowly adjust. This approach can improve participation of the patient and thus increase strength gains. Further physical conditioning with regimented aerobic training, catered to the patient’s personal interests, and institution of a home exercise program may reduce pain, improve stress management, and increase work capacity. It is important to encourage physical activity as much as possible. General aerobic conditioning can be effective in encouraging a positive health perception.
Relaxation training may also be helpful for chronic, nonspecific regional arm pain [24]. Continued surveillance and treatment of mental health problems can be imperative in recovery. Cognitive-behavioral therapy techniques can be used to treat the maladaptive beliefs and misconceptions that may accompany upper extremity dysfunction [25]. Moreover, weight reduction, if needed, and smoking cessation should also be included in any plan to improve overall health.
Other rehabilitative measures for RSI include the fabrication of splints and the introduction of adaptive equipment that may assist in functional activities at home and in the workplace. Some therapists are specially trained to perform work site analysis and to suggest ergonomic modifications. Modifications can range from adjustment in chair height and computer mouse position to the substitution of large-handled tools, depending on the occupation. For computer users, it is generally recommended that chair height be such that the forearms are relatively horizontal to the floor and the wrists are in a neutral position. The volar aspect of the wrist can be supported during typing by a wrist support placed on the desktop or support tray in front of the keyboard. The keyboard should be located in a position directly in front of the typist, minimizing ulnar deviation of either wrist. The mouse should be placed close to midline. Split keyboards and those that provide a trackball can help with forearm and hand positioning. Voice-activated software is also available for those patients whose symptoms are refractory to these modifications [18]. Ergonomically designed computer touch pads, a foot-controlled mouse, and document holders are other tools that can help decrease symptoms in RSI.
There is limited evidence in published literature to confirm the usefulness of ergonomic interventions [26]. A systematic review by Goodman and colleagues [27] investigated the most effective interventions for upper extremity cumulative trauma disorders in computer users. The highest levels of evidence were found for education and training in ergonomics, forearm supports, ergonomic keyboards, ergonomic mice, and exercise and rest breaks. Most clinicians agree that such interventions are a worthwhile component of a comprehensive rehabilitation plan. Ergonomic interventions may make the workplace more comfortable, encouraging the patient to return to work and possibly preventing work disability [28]. Education about proper ergonomics should empower patients to make low-cost changes on their own at work and at home.
Many factors can limit the effectiveness of work hardening and work conditioning programs. Individuals who are having difficulty in returning to their previous level of work activity should be evaluated for alternative jobs. This can involve consideration of a new position with the current employer, if it is mutually agreed on. Job redesign that enriches career development opportunities may be effective. In fact, studies suggest that interventions aimed at altering workers’ perceptions of monotonous or tedious work, through better job development opportunities, an increase of latitude over working patterns, and the improvement of communication between employers and employees, may be beneficial and cost-effective to the employer [29-31]. However, in some instances, an entirely different vocation must be pursued. If this is the case, a consultation with a vocational rehabilitation specialist is advised.
Procedures
Procedures are rarely indicated in RSI. In a population of patients with such a nondefinitive diagnosis, treatment failures are frequent. Therefore, trigger point injections, lateral epicondylar injections, carpal tunnel injections, and the like can be attempted to see if symptoms improve. The risk and benefits of each procedure should be explained in detail, including the risk of no relief of pain.
Surgery
Surgery is not indicated for RSI.
Potential Disease Complications
The most feared complication of RSI is increasing functional impairment and disability in all aspects of life. Negative outcomes can occur if the patient feels incapable of using his or her arms and hands. This may result in the inability to participate in home, work, and recreational activities. Depression and social isolation may accompany prolonged periods of absence from work.
Potential Treatment Complications
Treatment complications are rare. Most complications are associated with pain medication side effects. Analgesics and NSAIDs have well-known adverse reactions that most commonly affect the gastric, hepatic, and renal systems. Anticonvulsants can cause fatigue, ataxia, edema, or nausea. Tricyclic antidepressants have a high profile of fatigue, dizziness, dry mouth, and constipation. Patients should be informed of the side effect profile of each medication before administration. The patient’s complete medication list should be reviewed to address potential adverse reactions between medications taken concurrently.







