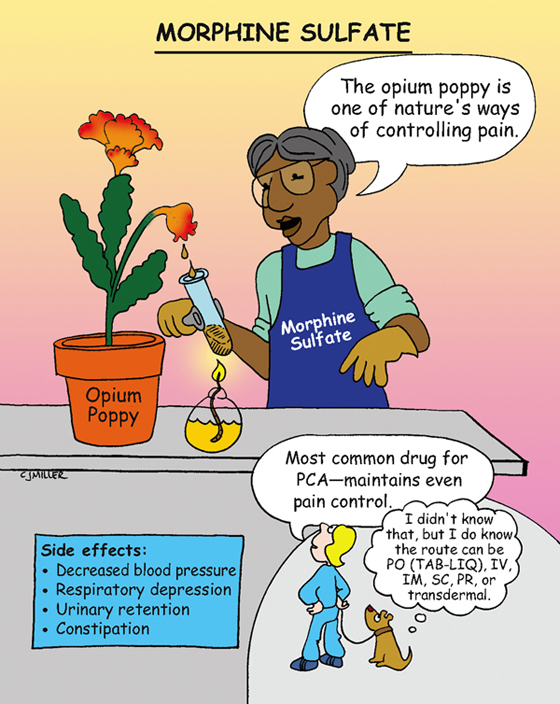
Morphine Sulfate
CLASSIFICATION
Analgesic, opioid agonist
ACTIONS
Interacts at a specific receptor-binding site. Agonist activity at the receptor site can result in analgesia, euphoria, depression, hallucinations, miosis, and sedation. Alters pain at the spinal cord and higher levels in the central nervous system (CNS) (Schedule II on Controlled Substances Act).
USES
• Relieves mild-to-severe pain.
CONTRAINDICATIONS
• Hepatic and renal dysfunction
PRECAUTIONS
• Seizures, asthma, and severe respiratory depression
SIDE EFFECTS
• Urinary retention, **confusion**
• **Constipation,** nausea and vomiting
• Tolerance and physical dependency with long-term use
• Toxicity: coma, respiratory depression, and pinpoint pupils
NURSING IMPLICATIONS
1. Perform strict documentation and inventory assessment of narcotic.
2. *Assess pain and vital signs (especially respirations) before and after the dose; do not administer if respirations are below 12 breaths per minute.*
3. Infants and older adults are very sensitive to depression of respirations.
4. *Naloxone (Narcan) reverses the effect of morphine.*
5. Medication of choice for patient-controlled analgesic (PCA).
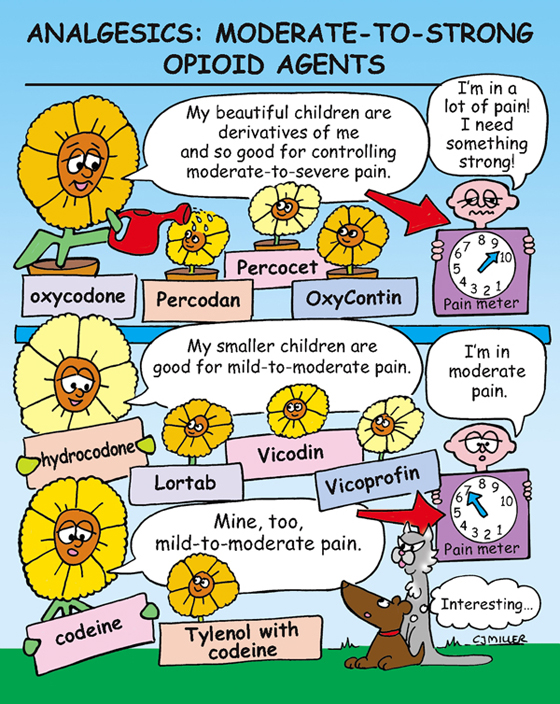
Analgesics: Moderate-to-Strong Opioid Agents
ACTIONS
Bind with receptors in the brain and spinal cord that are associated with pain. Moderate opioid analgesics are similar to morphine; however, pain control is less effective, and the potential for respiratory depression is less.
OPIOID ANALGESICS
• Percodan—combined with aspirin.
• Percocet—combined with acetaminophen.
• Combunox—combined with ibuprofen.
• Lortab—combined with acetaminophen.
• Vicodin—combined with acetaminophen.
• Vicoprofen—combined with ibuprofen.
• May also be combined with antihistamines and nasal decongestants for cough suppression.
codeine—PO, IV, IM, SQ Schedule II
• Tylenol with codeine (PO) for mild pain relief.
• Frequently combined with various agents for suppression of cough.
NURSING IMPLICATIONS
1. *Assessment is critical to effective pain control. Carefully assess patient’s level of pain and administer analgesic as ordered.*
2. Follow institution procedure for Controlled Substance Act.
3. Reassess patient 1 hour after administering medication.
4. *Administer medication before pain returns; fixed schedule of dosing may be more efficient than “as needed” dosing.*
5. *The majority of hospitalized patients do not receive adequate medication to relieve pain; therefore concern for addiction while hospitalized is usually not warranted.*
Narcotic Antagonists: Naloxone (Narcan)
ACTIONS
Opioid antagonists block (or antagonize) opiate-receptor sites. Principle use is the treatment of opioid or analgesic overdose.
USES
• Reverse the opiate effects of narcotic overdose and respiratory depression.
CONTRAINDICATIONS AND PRECAUTIONS
• Patients who are using nonopioid drugs
• Patients with a history of dependency; may precipitate acute withdrawal
SIDE EFFECTS
• Too rapid reversal of narcotic depression—nausea, vomiting, tremors, hypertension
• Minimal pharmacologic effects in absence of narcotics
NURSING IMPLICATIONS
1. *Preferred route of administration is intravenously; response is within 1 to 2 minutes, and peak action is within 20 to 60 minutes.*
2. *Patient should be frequently assessed; if the narcotic analgesic lasts longer in the system than the action of the Narcan antagonist, then respiratory depression may reoccur.*
5. *Not effective against barbiturates or other central nervous system depressant medications.*
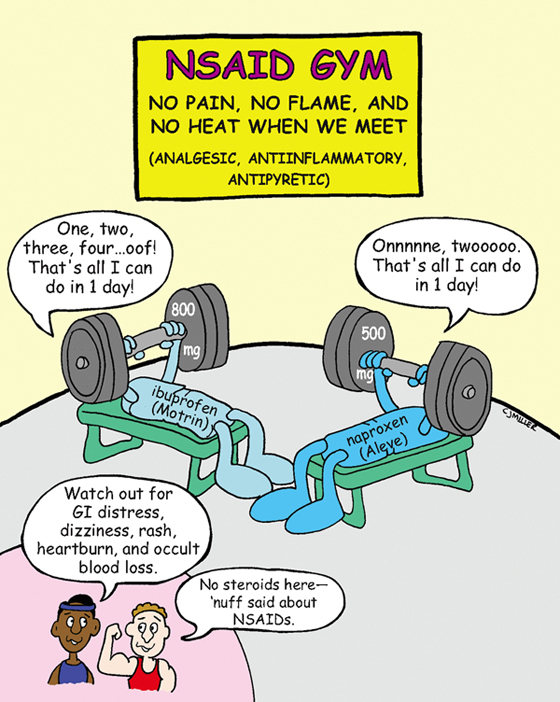
Nonsteroidal Antiinflammatory Drugs (NSAIDs)—Nonaspirin
ACTIONS
Suppress inflammation by inhibiting cyclooxygenase, an enzyme that is responsible for the synthesis of prostaglandins. NSAIDs inhibit the formation and release of prostaglandin.
USES
• Primary use is for rheumatoid and osteoarthritis.
• Reduce inflammation, pain of dysmenorrhea, and headache.
CONTRAINDICATIONS AND PRECAUTIONS
• History of gastrointestinal (GI) inflammation, ulceration, and bleeding are present.
• Is not recommended for use during pregnancy.
• Do not take before or immediately after coronary artery bypass graft (CABG) surgery.
• Increased risk of renal insufficiency in older patients with other chronic conditions.
SIDE EFFECTS
• **Dyspepsia, anorexia, nausea** and vomiting
• Rash, dizziness, **heartburn,** †GI bleeding†
NURSING IMPLICATIONS
1. ‡Take with food or milk to reduce GI distress.‡
2. ‡Instruct patient to use correct concentrations for age groups (infants, children).‡
3. *Do not crush or chew enteric-coated tablets.*
4. ‡Teach patient to avoid alcohol and aspirin products while taking NSAIDs.‡
5. ‡Patient should avoid all NSAIDs for a least 1 week before surgery or invasive diagnostics.‡
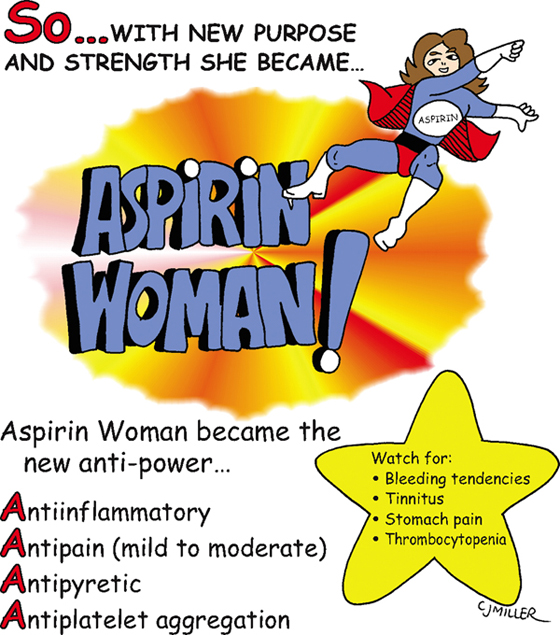
Acetylsalicylic Acid (ASA)—Aspirin
CLASSIFICATION
• Analgesic, antipyretic, antiplatelet; nonsteroidal antiinflammatory drug (NSAID)
ACTION
Cyclooxygenase inhibitors decrease the formation of prostaglandins involved in the production of inflammation, pain, and fever. Inhibits platelet aggregation.
USES
• Relieves low-to-moderate pain.
CONTRAINDICATIONS AND PRECAUTIONS
• Hypersensitivity to salicylates
• History of gastrointestinal (GI) ulceration, peptic ulcer disease (PUD), or any bleeding disorder
• †Children with a recent history of viral infection (e.g., influenza, chickenpox) that has been associated with Reyes syndrome†
SIDE EFFECTS
• Decreases platelet aggregation; **increases bleeding potential**
• **Epigastric distress,** heartburn, and nausea
• Aspirin overdose or toxicity—respiratory alkalosis that progresses to respiratory depression and acidosis; hyperthermia, sweating, and dehydration with electrolyte imbalance; **tinnitus,** headache
NURSING IMPLICATIONS
1. ‡Give with milk or full glass of water to decrease gastric irritation.‡
2. ‡Teach safety measures to parents regarding medications at home.‡
3. *The potential for toxicity is high in older adults and children.*
4. ‡Teach patient to avoid concurrent use of alcohol to decrease GI irritation.‡
5. ‡Patient should not take aspirin for at least 1 week before surgery.‡
6. *Evaluate patient to determine purpose of medication—pain, inflammation, or antiplatelet action.*
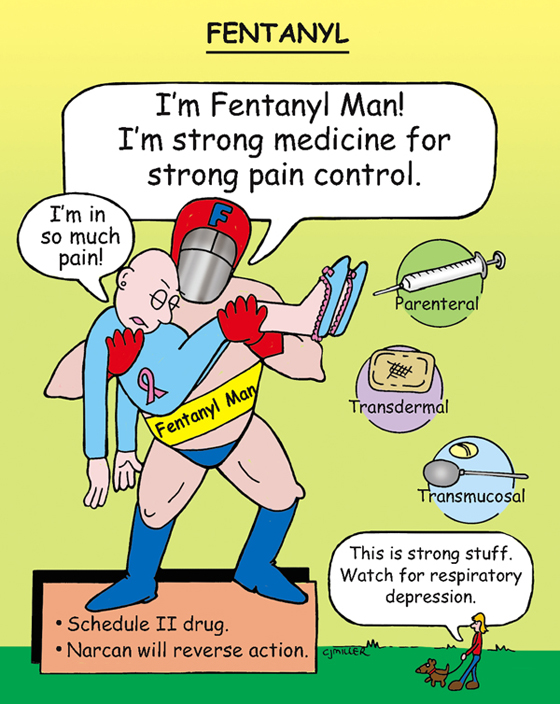
Fentanyl
CLASSIFICATION
• Strong narcotic analgesic; Schedule II of Controlled Substances Act
USES
• Fentanyl (Sublimaze) (IM, IV)—facilitates the induction of anesthesia; may be used with droperidol.
CONTRAINDICATIONS
• Is only indicated for the relief of severe pain.
SIDE EFFECTS
• **Sedation, euphoria, and constipation**
• **Hypotension,** pupillary miosis
• Tolerance and physical dependency with long-term use
NURSING IMPLICATIONS
1. *Perform strict documentation and inventory assessment of narcotic.*
2. *Assess pain and vital signs (especially respirations) before and after the dose; do not administer if respirations are below 12 breaths per minute.*
3. *Pay close attention to guidelines for administration.*
4. Patch is used for opioid-tolerant patients, not for control of postoperative pain.
5. *Respiratory depression can be reversed with nalozone (Narcan).*
6. ‡Teach patients to avoid exposing the patch to external heat sources (e.g., heating pads, hot baths, electric blankets); doing so can accelerate the release of the medication, as can fever, sunbathing, and strenuous exercise.‡