CHAPTER 11 Lower Limb Pain: Hip, Thigh, Knee, Leg, Ankle, and Foot
INTRODUCTION
The lower limb consists of four major parts:
It is important to stress again that acupuncture practitioners must treat the whole body, not only the local symptoms. When treating the lower limb, a practitioner must examine the lower back. If there are tender points in the lower back, a practitioner must examine the upper back and the neck. This is why it is so important for an acupuncture practitioner to understand basic anatomy as it relates to acupuncture therapy and why so many chapters in this book emphasize anatomical descriptions from this standpoint.
BASIC ANATOMY OF THE LOWER LIMB: ITS RELATION TO PAIN AND ACUPUNCTURE THERAPY
The Bones of the Lower Limb
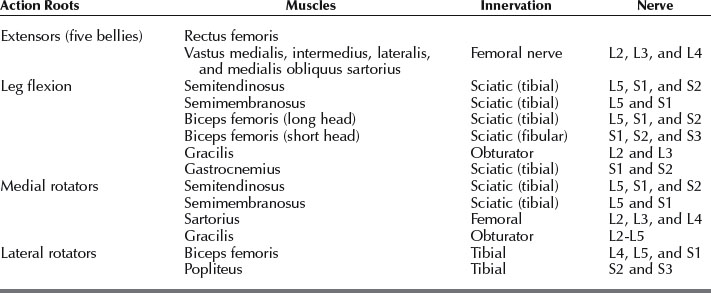
The large, irregular hip bone (os coxae) is composed of three bones: ilium, ischium, and pubis. These bones begin to fuse at 15 to 17 years of age and the fusion is complete by age 23. Thus, the hip bone is indistinguishably joined in an adult (Figure 11-1). A cup-shaped socket (named acetabulum, after a shallow cup used in ancient Rome for vinegar) is formed where the three bones fuse. The acetabulum and head of the femur form the hip joint.
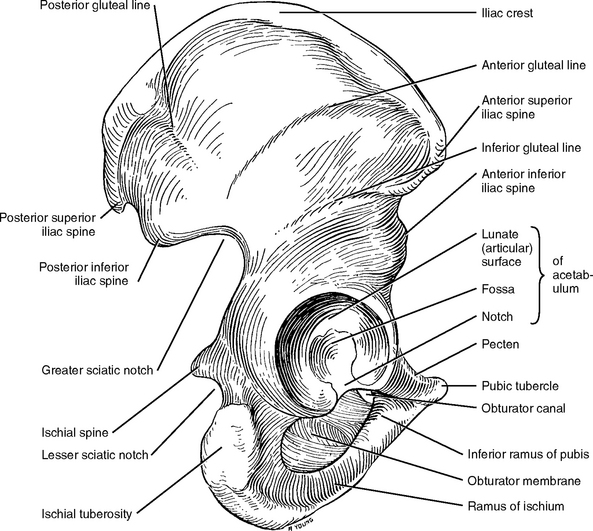
Figure 11-1 Hip bone and its articular surfaces. Lateral view.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 264.)
The femur is the longest, strongest, and heaviest bone in the body (Figure 11-2). A person’s height is about four times the length of the femur. The femur consists of a rounded head, neck, and greater and lesser trochanters at the proximal portion of the shaft, and two broadened lateral and medial condyles at the distal portion. The two condyles articulate with the tibia and patella to form the knee joint.
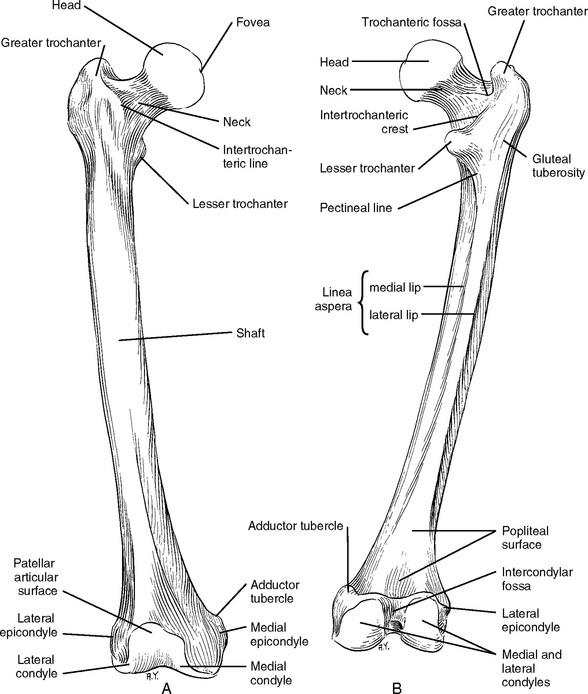
Figure 11-2 Anterior (A) and posterior (B) views of the femur.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 269.)
The leg consists of two bones, the tibia (shin bone) and the fibula (splint bone, calf bone). The tibia is the second largest bone in the body and is located on the anteromedial side of the leg. The tibia supports most of the body weight. The proximal end of the tibia is large and its lateral and medial condyles articulate with the corresponding condyles of the femur. The patellar ligament from the thigh muscles inserts into the prominent tibial tuberosity. The distal end of the tibia is small and has articular surfaces for the fibula and talus (Figure 11-3). Here the tibia forms the medial malleolus to stabilize the ankle. The shaft of the tibia is triangular in cross section.
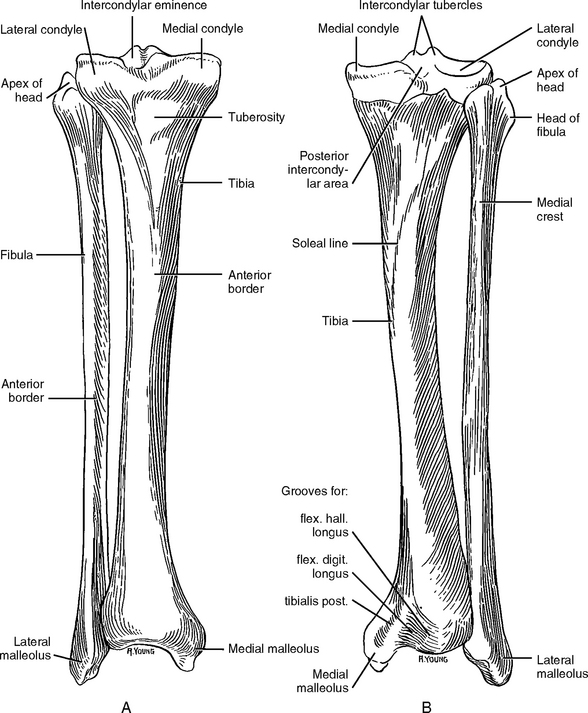
Figure 11-3 Anterior (A) and posterior (B) views of the right tibia and fibula.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 329.)
The fibula is a long, pinlike bone (fibula means “pin” in Latin) that articulates with the tibia posterolateral. The fibula serves mainly as an attachment for muscles and gives stability to the ankle joint. The proximal end of the fibula is its head, which has a facet to articulate with the inferior surface of the lateral tibial condyle. The distal end of the fibula is the lateral malleolus, which helps to hold the talus in its socket (see Figure 11-3).
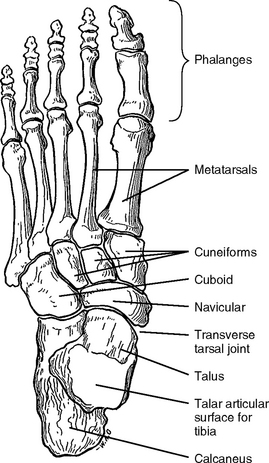
The foot consists of 7 tarsal bones, 5 metatarsal bones, and 14 phalanges (Figure 11-4). Of the seven tarsal bones, only the talus articulates with the leg bones. When treating ankle and foot pain, the practitioner needs to understand the anatomy and biomechanics of the foot to know where to find the symptomatic acupoint(s) (SAs). This chapter will focus only on cases that are commonly seen in acupuncture clinics, such as ankle sprain and plantar fasciitis, and will therefore not describe the complete anatomy and biomechanics of the foot, although readers may consult the available professional literature for more detailed knowledge.
Muscles
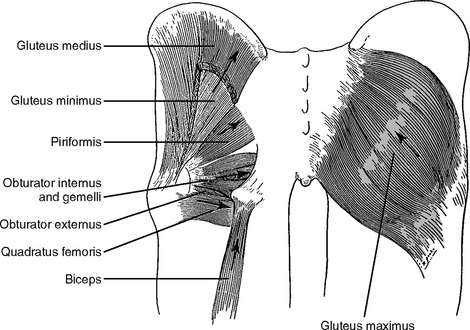
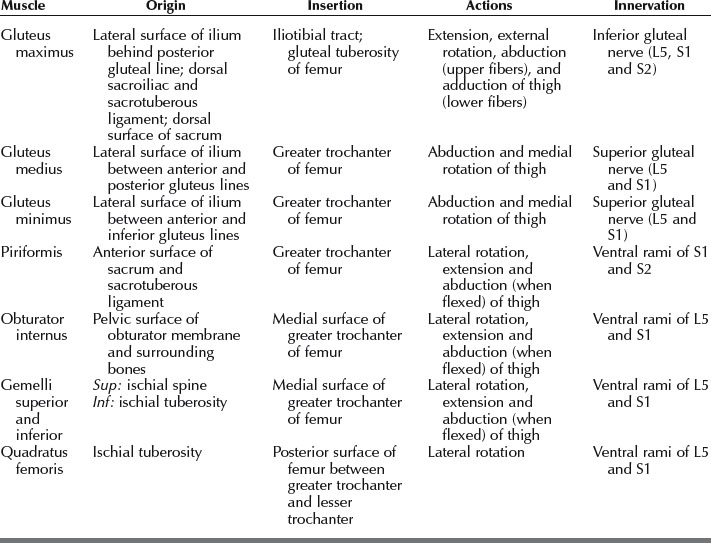
The Gluteal Muscles
The gluteal muscles include (1) the three large glutei (gluteus maximus, medius, and minimus) and (2) four deeper small muscles (piriformis, obturator internus, gemelli, and quadratus femoris) (Figure 11-5). The three large glutei are extensors and abductors of the thigh at the hip joint and they also stabilize the pelvis. The small muscles are lateral rotators of the thigh at the hip joint and stabilize the femoral head in the acetabulum. Table 11-1 shows a summary of the muscles of the gluteal region.
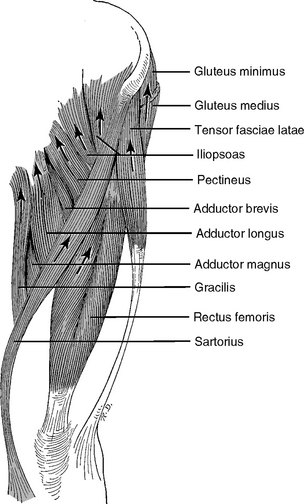
The Anterior Thigh Muscles (Flexor Group)
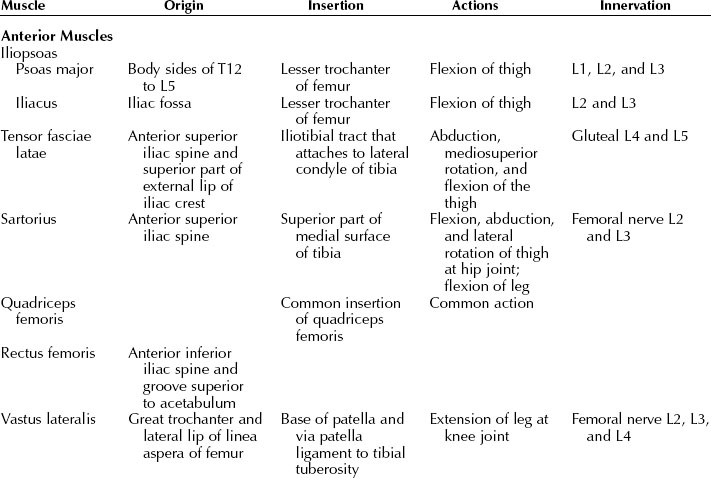
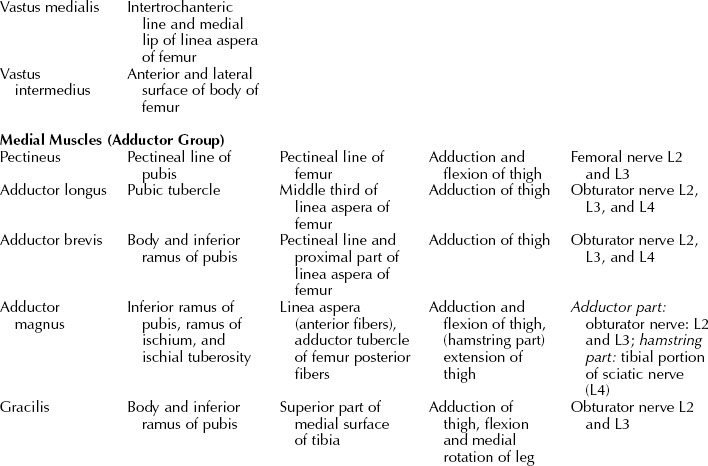
The major muscles of the anterior group are iliopsoas, tensor fasciae latae, sartorius, and quadriceps femoris (Figure 11-6). They are accessible to acupuncture needling. Their anatomic function is summarized in Table 11-2.
The Medial Thigh Muscles (Adductor Group)
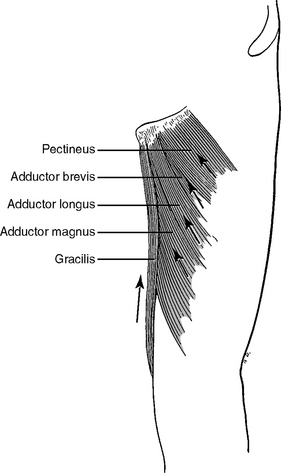
The medial thigh muscles (the pectineus, adductor longus, adductor brevis, adductor magnus, gracilis, and obturator externus) are adductors of the thigh (Figure 11-7). All of these muscles are supplied by the obturator nerve (L2, L3, and L4) except pectineus, which is supplied by the femoral nerve (L2 and L3). The “hamstring” part of the adductor magnus is supplied by the sciatic nerve (L4).
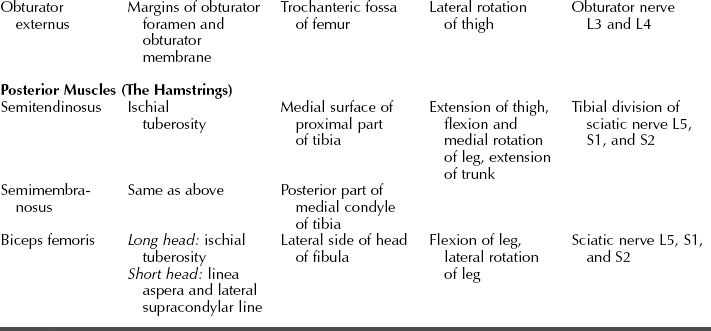
The Posterior Thigh Muscles (The Hamstrings)
Three large muscles (semitendinosus, semimembranosus, and biceps femoris) of the posterior aspect are collectively known as the hamstring muscles (Figure 11-8). These muscles have the same origin on the ischial tuberosity, but the short head of the biceps femoris has an additional origin on the shaft of the femur. These long muscles extend from the hip joint and across the knee joint so they are all extensors of the thigh and flexors of the leg. In addition, they are all supplied by the same sciatic nerve.
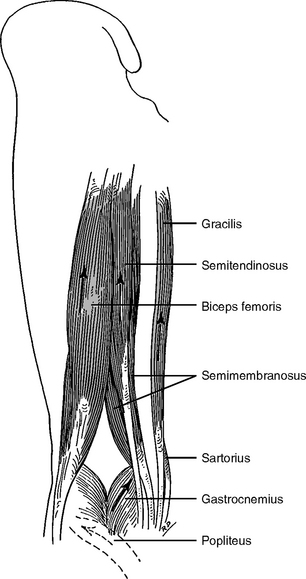
Figure 11-8 The hamstrings: the flexors of the leg.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 320.)
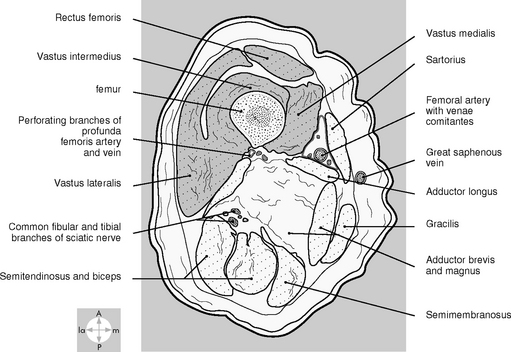
The topography of the three groups of thigh muscles is shown in Figure 11-9.
The Leg Muscles
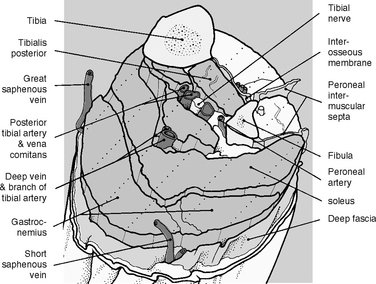
Anatomically and functionally the leg muscles are divided into three compartments by (1) the tibia, the fibula, and the interosseous membrane between them and (2) the anterior and posterior crural intermuscular septa (Figure 11-10): the anterior, lateral, and posterior. The muscles in the same compartment perform similar functions and share the same nerve and blood supply.
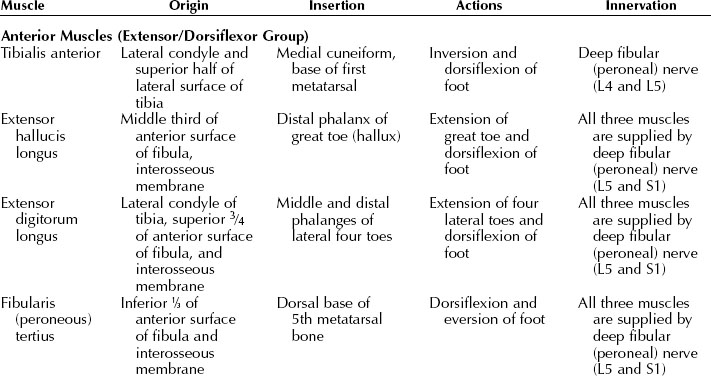
The anterior compartment is between the tibia and the anterior crural septum. The muscles of this compartment function as extensors of the toes and effect dorsiflexion of the ankle joint (Figure 11-11).
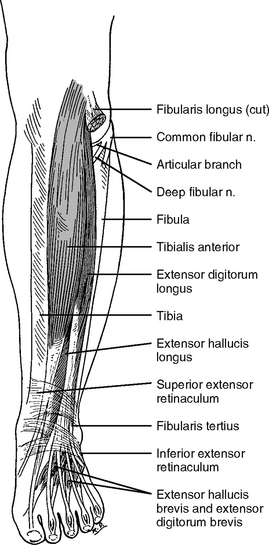
Figure 11-11 The anterior muscles of the leg.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 339.)
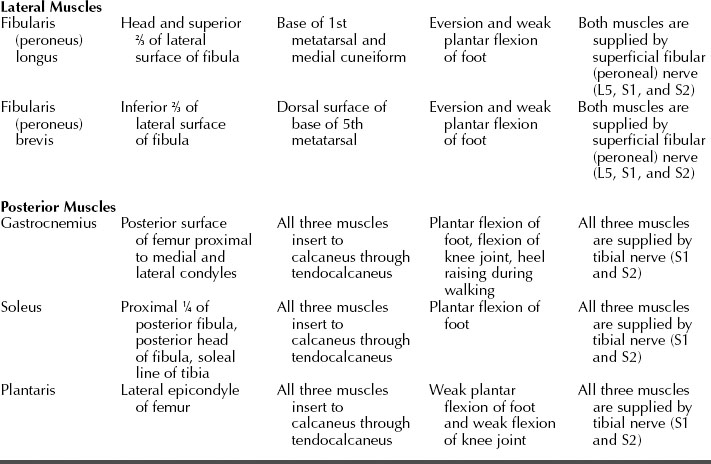
The lateral compartment is surrounded by the lateral aspect of the fibula and anterior and posterior crural intermuscular septa. The two muscles in this compartment are responsible for plantar flexion and eversion of the foot (Figure 11-12).
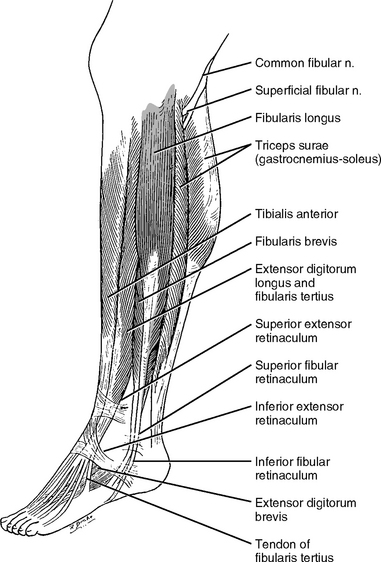
Figure 11-12 The lateral muscles of the leg.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 338.)
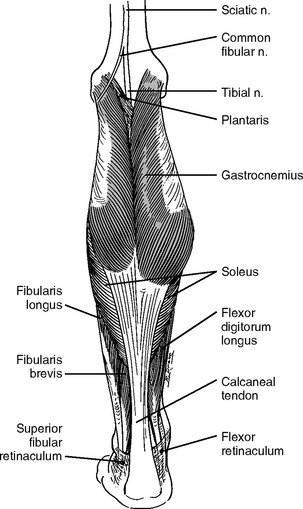
The posterior compartment contains both superficial and deep muscles (Figure 11-13). The three powerful superficial calf muscles affect plantar flexion of the foot. These large muscles support and move the weight of the body. Four smaller deep muscles of the posterior compartment act on the knee joint (popliteus) and ankle and foot joints. These four smaller muscles are not important in acupuncture therapy and therefore are not listed in Table 11-3.
Nerves of Clinical Importance
The Superior Cluneal Nerves
The superior cluneal nerves are branches of the dorsal rami of L1, L2, and L3. They emerge from the deep fascia just superior to the iliac crest and innervate the skin on the superior two thirds of the gluteal region (buttocks). An important homeostatic acupoint, H14 superior cluneal, is formed at the location where the nerves penetrate the deep fascia. Most patients feel tenderness or even pain upon palpation at H14. In patients with chronic lower back or leg pain, the pain may spread over the entire skin area that is supplied by the superior cluneal nerves. In such cases, H14 and adjacent areas should be needled together.
The Inferior Gluteal Nerve
The Sciatic Nerve and Its Terminal Branches: the Tibial, Common Fibular (Peroneal), and Sural Nerves
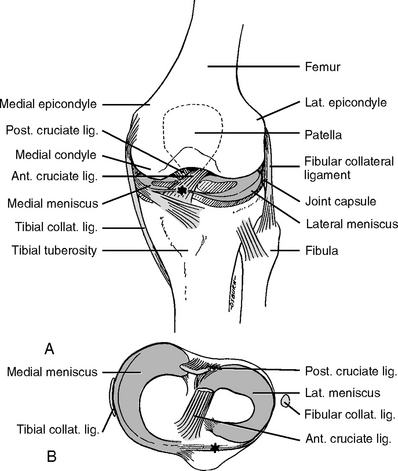
We have discussed this nerve in Chapter 5 and here we emphasize its relation to HAs and pain in the lower limb. The sciatic nerve is the largest nerve in the body. The ventral rami of L4, L5, S1, S2, and S3 converge at the inferior border of the piriformis muscle to form the sciatic nerve (Figure 11-14). Structurally the sciatic nerve consists of two nerves: the tibial and the common fibular (peroneal) nerve. The sciatic nerve leaves the pelvis through the greater sciatic foramen of the hip bone and enters the gluteal region inferior to the piriformis muscle (Figure 11-15). It runs deep below the gluteus maximus muscle, and does not supply any structure there. The sciatic nerve continues down the thigh covered by the hamstring muscles and ends in the lower third of the thigh, at which point the tibial and the common fibular (peroneal) nerves separate from each other.
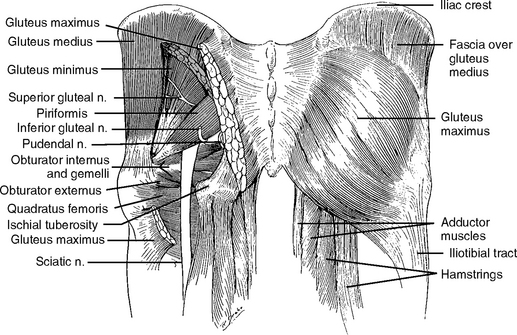
Figure 11-14 Sciatic nerve and the piriformis muscle.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 300.)
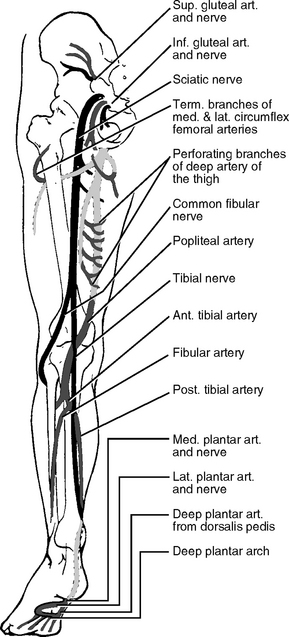
Figure 11-15 The distribution of the sciatic nerve.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 259.)
The common fibular (peroneal) nerve arises from the sciatic nerve just above the popliteal fossa as a lateral branch. It descends to the lateral aspect of the leg and winds around the lateral surface of the head of the fibula where acupoint H24 common fibular (peroneal) is formed. The common fibular (peroneal) nerve enters the lateral compartment of the leg and divides into two cutaneous branches: the superficial and the deep fibular (peroneal) nerves. The superficial fibular (peroneal) nerve innervates the anterior aspect of the skin in the lower leg and ankle area. The deep fibular (peroneal) nerve descends down to the foot and becomes the cutaneous nerve at a point approximately 2 cm proximal to the web between the great and second toes. Here acupoint H5 deep fibular (peroneal) is formed.
Femoral and Saphenous Nerve
The femoral nerve is the largest nerve formed in the abdomen by the branches of the lumbar plexus (L2, L3, and L4) (Figure 11-16). In the thigh area, the femoral nerve gives off muscular branches to supply the anterior thigh muscles. When affected by injury or overuse, these muscles become tender or painful and form SAs.
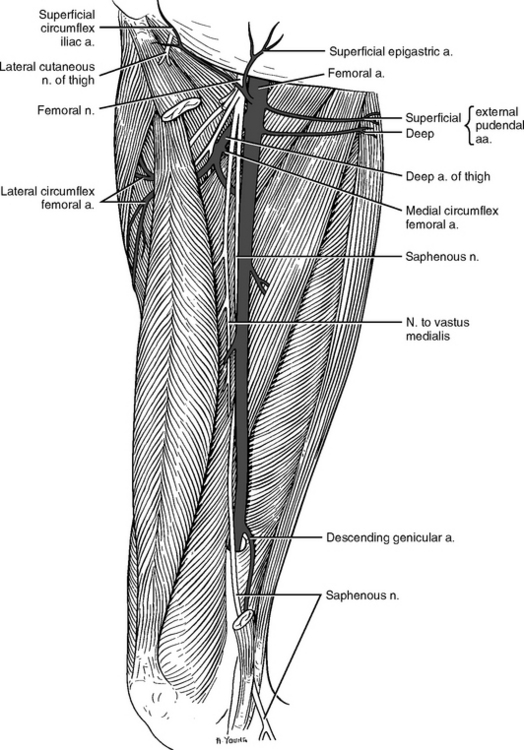
Figure 11-16 The femoral and saphenous nerves of the right thigh.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 289.)
The cutaneous branch of the femoral nerve, called the saphenous nerve, runs down to the medial aspect of the knee. It passes anteroinferiorly to supply the skin of the anterior and medial aspect of the knee, leg, and foot. As the saphenous nerve pierces the deep fascia on the medial side of the knee just below the medial condyle of the tibia, an important HA, H4 saphenous, is formed. You may remember that H4 saphenous and H1 deep radial are used as diagnostic acupoints for quantitative evaluation of acupuncture patients.
Obturator Nerve
The obturator nerve is derived from the same spinal segments as the femoral nerve (L2, L3, and L4). The obturator nerve leaves the pelvis through the obturator foramen and enters the thigh to supply the adductor muscles (Figure 11-17).
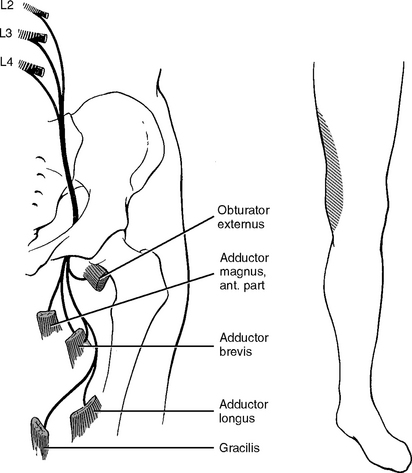
Figure 11-17 The obturator nerve.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 292.)
The adductor muscles are involved in many painful conditions of the thigh, especially in athletic persons, but are often ignored by healthcare professionals. Whenever treating patients with leg pain, particularly pain in the hamstring muscles, the adductor muscles should be carefully palpated and the tender points in the adductor muscles should be needled.
Joints of the Hip and Lower Limb
The Hip Joint
The human hip joint is a well-constructed multiaxial joint that has the function of bearing weight, maintaining posture, and facilitating walking. The hip joint is a closely fitting ball-and-socket synovial joint in which the globular head of the femur articulates with the cup-like acetabulum of the hip bone (see Figure 11-1). However, the movement of the femur is limited by the close articular surfaces and strong ligaments of the hip joint. In the case of the shoulder, dislocation of the joints will occur if they are not stabilized by the surrounding muscles. In contrast, the hip joint is able to support the body weight on the head of the femur with little or no muscular energy.
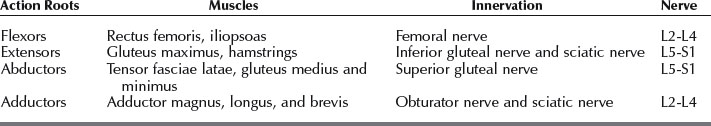
Understanding the nerve supply to the hip joint helps us to treat the nerve(s) associated with hip pain (Table 11-4). The articular branches of the femoral nerve supply the anterior part of the joint capsule and the iliofemoral ligament. The obturator nerve sends branches to the anteroinferior part of the joint and the medial portion of the capsule. The superolateral aspect of the capsule is innervated by the superior gluteal nerve. The sciatic nerve is believed to supply the posterior portion of the capsule.
General Considerations of Hip Pain Pathology
Hip pain and limping are the chief complaints presented by patients in an acupuncture clinic.
Hip joints sustain enormous stress in daily activities such as walking. For example, during walking, when the left limb is lifted, the right hip joint is subjected to compression forces several times greater than the body weight (Figure 11-18). A person does not feel this huge force of compression because there are no nerves in the articular cartilage. When the cartilage is eroded by degenerative disease or aging, the bony head of the femur, which is richly supplied by sensory nerves, produces pain during every step because of this compression force. As a person ages, the articular cartilage becomes thinner and hip pain may gradually develop.
A limp without pain is usually caused by mechanical abnormalities such as a shortened leg, muscle contracture, or muscle paralysis. Careful palpation of the hip, thigh, and leg of the affected limb will reveal that the muscles harbor some tender points. Needling of these tender points relaxes the shortened muscles and helps improve the discrepancy between the two legs.
Piriformis Syndrome
The exact cause underlying the piriformis syndrome is unknown, but many healthcare professionals believe that the piriformis muscle compresses the sciatic nerve where the nerve passes under or through the belly of the piriformis muscle.1
We have successfully treated patients who were diagnosed with piriformis syndrome by medical doctors. The most important acupoint is H16 inferior gluteal because it is just on top of the piriformis muscle. A long needle is needed to reach all the way down to the hip bone. This needling relaxes the piriformis muscle, improves blood supply to the muscle, and reduces inflammation (see Chapter 3).
Degenerative Arthritis
Degenerative arthritis is the most common painful and disabling condition of the hip joint. It is generally believed that the pain is caused by (1) degenerative changes in the hip cartilage, causing the bone tissue to directly sustain the huge force of compression and (2) abnormal articular orientation between the head of the femur and the surface of the acetabulum. As noted in the above discussion of hip pathology, the acetabulum is only incompletely covered by cartilage, so the cartilaged surface of the head of the femur must articulate with the cartilaged surface of the acetabulum of the hip bone. During walking, if a person’s knees come too close together or too far apart, the orientation of the head of the femur in the joints will change, resulting in hip pain because the heads of the femurs will articulate with the noncartilaged surface of the acetabulum.
Stress Fracture
In cases of stress fracture, acupuncture can be used as a supplementary therapy to reduce muscle and periosteum pain and to promote bone healing.
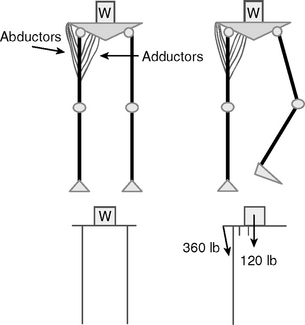
The Two Joints and Three Articulation Compartments of the Knee
The knee is the largest joint in the body and consists of three bones: the femur, tibia, and patella. The knee joint proper is formed by two joints: the femorotibial and the patellofemoral within the common cavity (Figure 11-19). The joint complex consists of three articulation compartments:
The patella is located within the quadriceps tendon and enhances the extension force of the quadriceps muscle. The patella and its surrounding soft tissues, such as the patellar ligament and bursae, are often a source of knee pain. The quadriceps muscle that is inserted in the patella has five bellies (Table 11-5). Any injury to one of the five bellies will misalign the five extension forces exerted on the patellar ligament and will cause knee pain.
The stability of the knee is maintained by ligaments, muscles, tendons, menisci, and the joint capsule. The bony architecture of the knee depends on the soft tissues for its stability, making the knee the most vulnerable structure in the body to soft tissue injury, and the resulting pain and functional impairment.
Muscles Responsible for Knee Movement
The muscles and their functions are summarized in Table 11-5. The extensor quadriceps femoris is composed of four heads. The rectus femoris originates from the anterior iliac spine, and the other three heads come from the shaft of the femur. All of the muscles share the same tendon that attaches to the tibial tubercle.
The muscles are the most dynamic elements among the possible causes of knee pain. They are the movers of the knee joint and are indispensable components of the knee, and thus they are liable to injuries from repetitive motion or stress due to overuse. Our experience in treating knee pain shows that most of the pain that is related to soft tissue injuries derives from disorders of the muscle, unless the pain is caused directly by physical trauma to the knee joint. If the muscles are tired or injured, they become tight and resistant to further motion. If they are forced to move under such conditions, it causes overstretching of other soft tissues of the knee such as the ligaments, capsule, bursae, and meniscus, which results in soft tissue inflammation.
Bursae of the Knee
There are four bursae anterior to the knee:
The Ankle Joint (Talocrural Joint)
The ankle joint articulates the leg with the foot. The ankle comprises three bones and two articulations. The distal ends of the tibia and fibula form the tibiofibular joint. The inferior ends of the tibia and fibula articulate with the superior part of the talus and form the ankle or talocrural joint (Figure 11-20). The foot itself consists of numerous joints of different types among its 26 bones, the description of which is beyond the scope of this book.
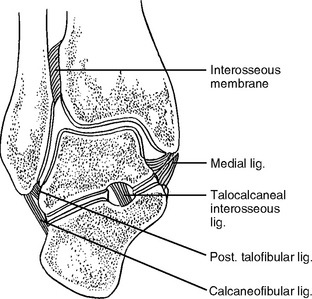
Figure 11-20 Frontal section through the ankle and subtalar joints. Ligaments and interosseous membrane are illustrated.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 357.)
The ankle joint is supported by the strong medial and weak lateral collateral ligaments. The MCL is known as the deltoid ligament. Superiorly the ligament attaches to the margin and tip of the medial malleolus. It fans out downward in a delta shape and its broad base attaches from the navicular bone anteriorly to the talus and calcaneus posteriorly. The lateral collateral ligaments consist of three discrete bands that attach the lateral malleolus to the talus and calcaneus: the anterior and posterior talofibular ligaments, and between these two short ligaments—a long, cordlike calcaneofibular ligament (Figure 11-21).
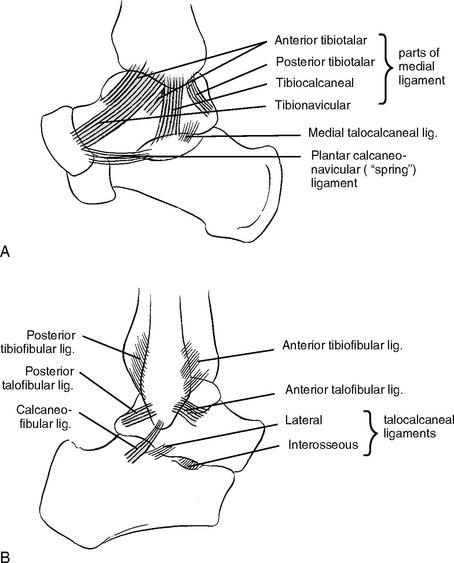
Figure 11-21 Diagram of the ligaments of the ankle and subtalar joints in medial and lateral views.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 358.)
Of the three lateral collateral ligaments, the anterior talofibular ligament is the weakest ligament, and the most commonly injured. Ligament injuries are discussed later in this chapter.
Ankle Strains
When an ankle strain occurs, a person feels a sudden sharp pain. This initial pain may soon subside, so that the person may not seek immediate treatment, but if it is possible to apply acupuncture treatment immediately after the injury, the inflammation reaction can be effectively controlled and the healing process is greatly quickened. In the first 6 to 12 hours after injury the ankle gradually becomes swollen and tender points or areas appear on both lateral and medial aspects. Bruising (ecchymosis) also develops in the foot and the lower leg. The patient is then no longer able to perform activities such as running or to bear normal weight on the injured ankle.
Rupture of the Calcaneal Tendon (Achilles Tendinitis)
The practitioner should carefully palpate the calcaneal tendon, the whole calf muscle, and both sides of the leg to find the tender points. At the rupture site, a few needles should be inserted deep into the ruptured tissue (Figure 11-22). The tender points on the calf muscles should also be needled. The procedure should be repeated every 3 or 4 days for the first 2 weeks. Pain relief can be achieved almost immediately in acute and fresh cases but recovery of function takes longer. In chronic cases, both pain relief and recovery of function will take longer. During the period of treatment, the patient should use a heel insert to elevate the heel about 2 cm, which will reduce the stretch of the Achilles tendon and the gastrosoleus muscles and thereby facilitate healing.
Plantar Fasciitis
Palpation of the foot reveals a deep tender area beneath the anterior portion of the heel, especially at the anteromedial area of the calcaneus, the attachment point of the plantar fascia (see Figure 11-22). In some patients with acute or chronic heel pain, calcium can be deposited at this attachment site to form bone spurs, although most bone spurs will not result in pain. Other conditions causing a similar pain pattern include bursitis under the fascial attachment, atraumatic periostitis, and entrapment of the calcaneal branch of the tibial nerve.
In our clinic we have successfully treated both acute and chronic plantar fasciitis. The practitioner should perform a systemic examination of HAs, especially in the lower back area, posterior thigh, and calf muscles. It is necessary to carefully palpate the sole of the foot and the whole foot, paying attention to the heel bone (calcaneus), to find the most sensitive area. Two or three needles of 4 cm in length should be used to needle this tender area, as well as other tender points on the sole. In addition, it is advisable to needle HAs on the leg, thigh, buttock, and lower back. After treatments, a patient should resume mild lower limb activities and wear an orthopedic shoe or insert to support the foot arch and to avoid stretching the plantar fascia during walking.
TREATMENT PROTOCOL FOR LOWER LIMB PAIN
Symptomatic Acupoints
Thigh Pain
Carefully palpate the hamstring, the iliotibial band, and the quadriceps and adductor muscles including their attachments to the hip bone and the knee. Figure 11-23 shows the treatment of adductor muscle strains.
Knee Pain
Knee pain is always related to the muscles attached to the knee. First examine the knee area to understand the location of the pain and the possible tendons, ligaments, and bursae involved in this condition. Then carefully examine the muscles. For example, if pain is felt at the area of the MCL and the attachment of semitendinosis, the adductor muscles and semitendinosis should be palpated. The tender and painful points in the knee area and related muscles should be needled (Figure 11-24).