Allergy and Respiratory Medications
Objectives
1. Identify major antihistamines used to treat breathing problems caused by allergies.
2. Describe the action of antitussive medications.
3. List medications used to treat and prevent asthma attacks.
4. Describe the major actions and adverse reactions of the two main categories of bronchodilators.
5. Identify at least six medications commonly used as decongestants.
6. Describe the mechanism of action for expectorants.
7. List the major contraindications to the use of nasal steroids.
Key Terms
antihistamines (ăn-tĭ-HĭS-tă-mēnz, p. 138)
antitussives (ăn-tĭ-TŬS-ĭvz, p. 142)
bronchodilators (brŏn-kō-DĪ-lā-tŏrz, p. 145)
bronchospasm (BRŎN-kō-spăzm, p. 144)
contraindications (kōn-tră-ĭn-dĭ-KĀ-shŭns, p. 139)
expectorants (ěk-SPĔK-tŏr-ănts, p. 155)
histamine (HĬS-tă-mēn, p. 138)
leukotriene receptor inhibitors (lū-kō-TRĭ-ēn, p. 150)
ototoxic (ŏ-tō-TŎK-sĭk, p. 139)
perennial allergic rhinitis (PAR) (ă-LĔR-jĭk rī-NĪ-tĭs, p. 138)
perennial nonallergic rhinitis (PNAR) (NŎN-ă-lěr-jĭk, p. 138)
precautions (prē-CĂW-shuns, p. 139)
prophylaxis (prŏ-fĭl-ĂK-sĭs, p. 144)
rebound effect (p. 140)
rebound vasodilation (vā-sō-dĭ-LĀ-shŭn, p. 152)
refractoriness (rē-FRĂK-tŏ-rĭ-něs, p. 147)
seasonal allergic rhinitis (SAR) (ă-LŬR-jǐk, p. 138)
sympathomimetics (SĬM-păth-ō-mĭ-MĔT-ĭks, p. 145)
wheezing (p. 144)
xanthines (ZĂN-thēnz, p. 145)
Overview
![]() http://evolve.elsevier.com/Edmunds/LPN/
http://evolve.elsevier.com/Edmunds/LPN/
This chapter looks at medications that affect the respiratory system. The first section, Antihistamines, describes medications used to treat breathing problems caused by allergies. The second section discusses antitussives, or medications used to control coughing. The third section describes the several different categories of medications used for the prophylaxis (prevention) and treatment of asthma and chronic obstructive pulmonary disease (COPD). The fourth and fifth sections cover decongestants and expectorants. The final section discusses nasal steroids used to treat respiratory problems.
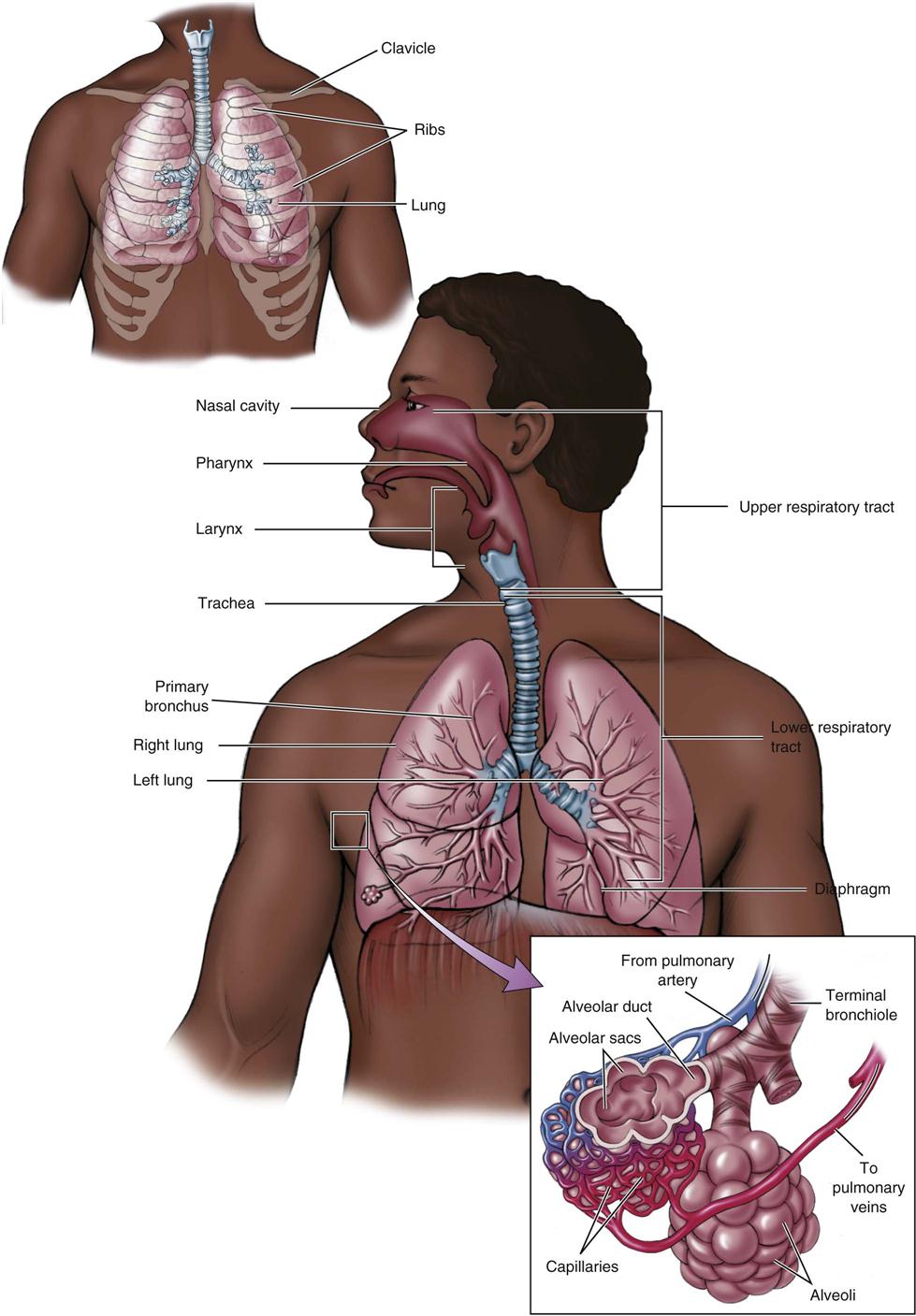
Respiratory System
The respiratory system is made up of the lungs and the respiratory passages (Figure 11-1). The upper respiratory system—the oral and nasal cavity, sinuses, pharynx, larynx, and trachea—provides the passages for air to move into the bronchi and lungs (the lower respiratory system). The lungs are divided into lobes. The respiratory system acts to exchange gases (oxygen and carbon dioxide) between the blood and the air and regulates blood pH.
When you take a deep breath (inspiration), the diaphragm drops down; at the same time, the intercostal muscles contract, raising the ribs, increasing the size of the chest, and creating a negative pressure. The negative pressure causes air to rush into the lungs through the respiratory passages. When you breathe out (exhalation), the muscles relax, the pressure increases in the chest, and air is passively forced out of the lungs. Thus, the chest works when breathing in and rests when breathing out.
Any part of the respiratory passages or structures and the lungs themselves may be abnormal. Common problems requiring medication are strictures (narrowed openings) or obstructions (blockage) caused by infection or mucus, collapse of the bronchioles caused by asthma, or infectious masses or tumors. The upper airways are often the site of allergic reactions and bacterial and viral infections.
Antihistamines
Overview
Histamine is a chemical the body produces that causes the inflammatory response. Mast cells found near capillaries and white blood cell basophils contain large amounts of histamine. When the body is injured, histamine is released, and it causes the smooth muscle and vascular system to increase blood flow by opening up the capillaries. This also makes the skin turn red. Fluid then escapes from the capillaries into the tissues, causing swelling. The amount of histamine released after an injury or an allergic reaction varies. Antihistamines relieve the effects of histamine on body organs and structures.
Action
There are two types of antihistamines. Histamine H1— receptor antagonists do not prevent the release of histamine, but rather compete with free histamine for binding at H1-receptor sites on the “effector structures” (e.g., vascular and nonvascular smooth muscles, salivary glands, and respiratory mucosal glands). This blocking action limits the vasodilation (opening) and bronchoconstriction, and increased capillary permeability and reduces the edema (swelling) caused by histamine. Antihistamines also limit the release of acetylcholine, producing an anticholinergic (drying) effect, particularly in the bronchioles and gastrointestinal (GI) system. Antihistamines also have a sedative effect on the central nervous system (CNS). Histamine H2 antagonists compete with histamine at the H2 receptor sites also, but only at the H2 receptors located in the GI tract and so will be discussed later in the text.
Uses
Antihistamine H1 receptor antagonists are used to treat seasonal allergic rhinitis (SAR) and perennial allergic rhinitis (PAR). Allergic rhinitis is a condition in which the patient has a reaction to either outdoor allergens (SAR) or indoor allergens (PAR). Histamine plays a central role in producing most of the typical eye and nasal signs and symptoms such as sneezing, nasal stuffiness, and postnasal drip. These signs and symptoms are also found in patients with perennial nonallergic rhinitis (PNAR), which involves inflammation of the mucous membranes of the nose caused by problems other than allergies. Antihistamines are also used to treat nausea and vomiting, vertigo, insomnia, and to prevent motion sickness, and relieve symptoms of other allergic disorders (particularly urticaria [hives], angioneurotic edema, serum sickness, and prophylactically or to treat reactions to blood or plasma) and as an adjunctive (additional) therapy in anaphylactic (shock) reactions. Antihistamines are used in combination cold-remedy capsules to decrease mucus secretion. First-generation drugs may also be used at bedtime for sedation so people can sleep. Some antihistamines are powerful enough to help treat allergic bronchoconstriction that interferes with breathing.
Antihistamines are classed as either first-generation drugs or second-generation drugs. First-generation drugs are usually those products available over-the-counter (OTC) that patients use before they see a health care provider. Most of these products cross the blood-brain barrier and cause sedation (sleepiness) and are used in particular for helping older adult patients sleep. These products are very effective in helping remove some symptoms of sneezing, itching, and watery rhinorrhea when used for a short time. Because of the high incidence of overdosage of some of these drugs in combination products in children’s cough and cold medications, the FDA has issued a recommendation that OTC cough and cold products not be used in infants and children less than 2 years old. Some products should not be used in children younger than 6 years.
Second-generation antihistamines are newer, more effective, and usually have a more rapid onset of relief of sneezing, pruritus (itching), and watery rhinorrhea. These drugs do not cross the blood-brain barrier and so do not cause significant sedation. These products lack the antimetic effect so their use is limited to allergies. Some are available only by prescription and some OTC. In general, they are less effective against nasal congestion. As newer drugs, they may also be more expensive. Several second generation drugs have been removed from the market because they cause lethal arrhythmias of the heart.
It is important to understand what symptoms the patient is having so that the correct medicine can be taken. This is sometimes a challenge the way OTC products are marketed.
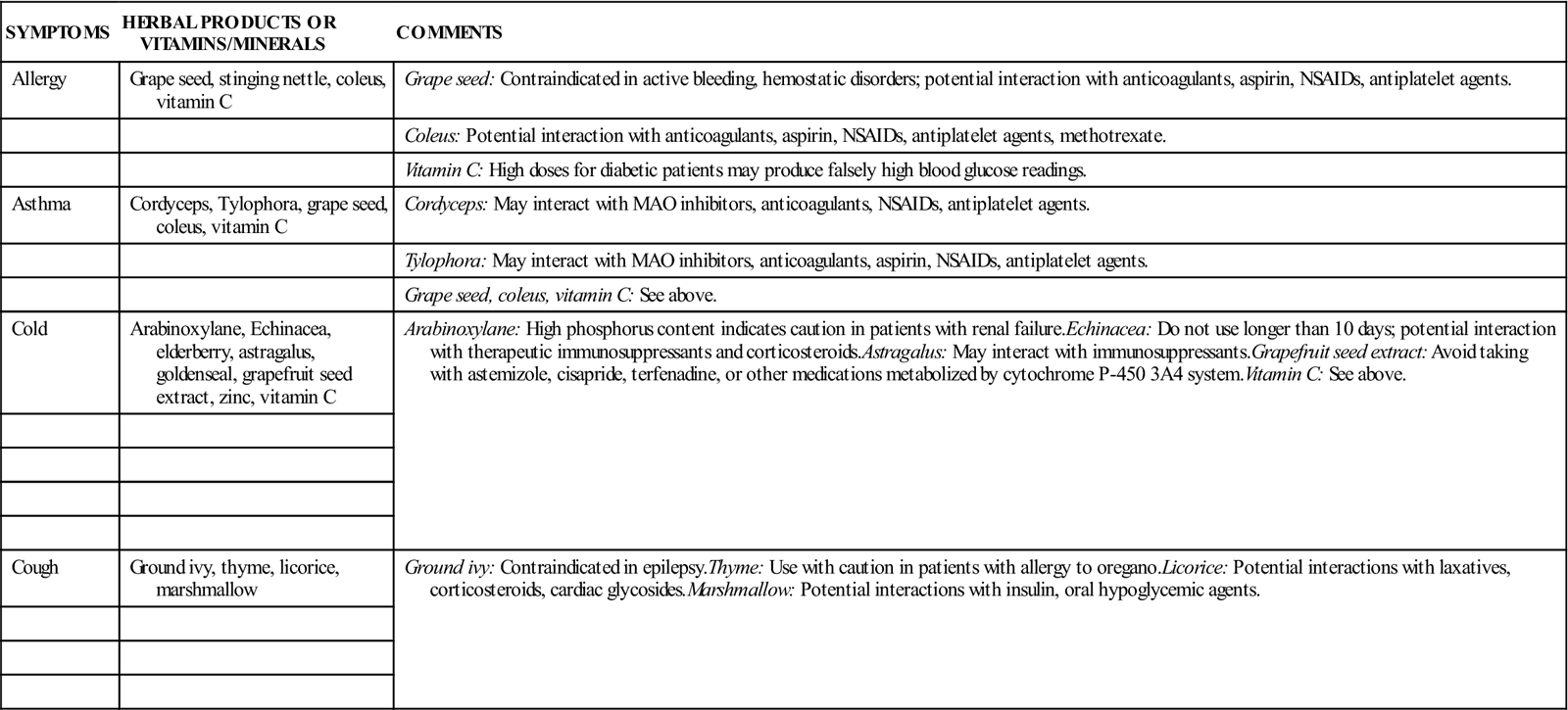
These two generations are further divided into six main groups of antihistamines, depending on their various characteristics and actions. These groups and some specific drugs within each group are listed in Box 11-1.
Adverse Reactions
The most common adverse reactions are due to the anticholinergic activity of the drugs: constipation, blurred vision, dry mouth, urinary retention, and dried thickened secretions due to mucosal drying. Patients may also develop hypertension (high blood pressure), hypotension (low blood pressure), tachycardia (rapid heartbeat), confusion, dizziness, drowsiness, excitation, insomnia (inability to sleep), paradoxic excitation (when a patient shows stimulation rather than the usual sedation), restlessness, sedation, tinnitus (ringing in the ears), anorexia (lack of appetite), diarrhea, nausea, vomiting, difficult or painful urination, impotence, urinary frequency, photosensitivity (abnormal response to exposure to sunlight), rash, urticaria (itching), and nasal congestion.
Antihistamine overdosage is potentially fatal, particularly in children. Any of these products should be used with caution in children and care taken to follow recommended dosages. The symptoms of overdosage occur when the CNS is being stimulated and depressed at the same time.
Drug Dosages
The dosage and delivery system for these medications should be determined based on the weight of the patient, the presence of other medical conditions, and the product. The dose will be carefully determined, based on many factors. Consult a drug handbook for common dosage recommendations.
Drug Interactions
The sedative effect commonly seen with antihistamines is increased when other CNS depressants (such as hypnotics, sedatives, tranquilizers, depressant analgesics, and alcohol) are used along with the antihistamine. The sedative effect of antihistamines also adds to the effect of anticholinergic drugs, and they can strengthen the anticholinergic side effects of monoamine oxidase (MAO) inhibitors, as well as tricyclic antidepressants. When antihistamines are used along with ototoxic drugs (drugs that may damage hearing, such as large doses of aspirin or other salicylates, or streptomycin), the ototoxic effects on the ear may be masked. Antihistamines can decrease the effect of corticosteroids and many hormones. They may also interfere with the effects of anticholinesterase drugs.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including the presence of drug allergy, other drug use, and the presence of asthma, glaucoma, peptic ulcer, prostatic hypertrophy, bladder neck obstruction, respiratory or cardiac disease, and the possibility of pregnancy. Assess the patients work and activities to see if drowsiness might be a problem. A patient with thyroid disease or migraine headaches may be unable to take antihistamines because of the tachycardia (rapid heartbeat) produced. These conditions are either contraindications (factors that rule out the use of a drug) or precautions (factors that indicate a drug should be used with great care) for the use of antihistamines.
As you listen to the patient describe respiratory symptoms, think about whether the problem might be SAR, PAR, or PNAR. The patient may have a history of allergic reactions with allergic nasal congestion (usually seasonal in onset), runny nose, or cough related to a cold or allergy. You may observe symptoms of rhinitis: sneezing, nasal discharge, and inflamed nasal mucosa. The patient may also have edema, dermatographism (wheals, or a raised surface of the skin where it has been scratched), conjunctivitis (inflammation of the inner eyelid and eye), eczema (a chronic condition producing irritation of the skin), insect bites, or contact dermatitis. The nasal mucosa may be swollen, boggy (soft), and pale, and there may be nasal plugging or a clear, watery discharge. Increased sinus pressure may be found when pushing on or palpating the frontal or maxillary sinuses.
These drugs are so common that it is important to learn the drug effects of antihistamine use. In young children, antihistamines may cause hallucinations, convulsions, and even death. Older adult patients are also extremely sensitive to these drugs. Some products may cause teratogenic effects (deformities) in a fetus, although most first and second generation drugs are Category B drugs with a few Category C drugs. Antihistamines should be used with caution in children with a family history of sleep apnea or sudden infant death syndrome (SIDS), or in children with symptoms of Reye syndrome.
n Diagnosis
Through reading the patient’s chart, you will learn why the patient is taking this drug: they may have SAR, PAR, or PNAR, or whether the medication is being given for some other type of allergic reaction. The severity of the symptoms will help in making the nursing diagnosis and deciding what additional nursing actions need to be taken (for example, hydration of the patient [giving additional fluid]).
n Planning
The sedative effect is common to most first generation antihistamines like diphenhydramine (Benadryl), less so with loratadine (Claritin) which is a second-generation antihistamine. The drowsiness caused by antihistamines makes it dangerous for the person taking them to operate heavy machinery or drive.
Some antihistamines may be given parenterally to treat hypersensitivity to blood products, as adjunctive therapy to analgesia, or in treating motion sickness. Most antihistamines are administered orally. Many are available in OTC preparations, although the forms with the highest dosage are available only by prescription. Most drug companies have at least one preparation available by prescription, so that people with Medicare or Medicaid benefits are able to get these drugs with their cards. Antihistamines may be administered rectally, or topically via nasal inhalation or ophthalmic solutions also.
Products that are used when a patient is hospitalized for severe respiratory difficulty are often administered by inhalation therapy by a respiratory therapist—an individual especially trained to use respiratory equipment and to assist the patient to get the most air into and out of their lungs. Watching and working with these respiratory therapists can help nurses increase their own skills to help patients breathe better.
n Implementation
Antihistamines should be taken only when needed. The type and dosage should be chosen for the desired effect and the person being treated. For example, one of the first-generation ethanolamine derivatives makes people very sleepy, and people who do tasks that require alertness probably should not use them. Sometimes a patient is having trouble sleeping and so the doctor may want to give them a drug that will make them drowsy so they might give them a drug from the ethanolamine category. Some drugs cause less drowsiness but may not be as effective in getting rid of the symptoms.
If tolerance (increased resistance to a drug caused by repeated use) to one type of antihistamine develops, the patient might be told to switch to another type to see if it is more helpful. Medications also might be changed or rotated to keep symptoms under control.
Giving oral doses with meals or milk can limit GI side effects however, the nurse should make sure that the medication can be given with foods or milk or if they need to be taken on an empty stomach. Antihistamines given orally are usually well absorbed; parenteral administration is rarely needed. When an intramuscular (IM) preparation such as diphenhydramine is used, it should be injected deep into the muscle to prevent tissue irritation. Intravenous (IV) injection of these agents should be done slowly, with the patient lying down because of the risk of the drug causing a low blood pressure. Long-term use of topical nasal antihistamines increases the risk of sensitization, often causing a rebound effect, or an increase in the symptoms you are trying to stop.
Table 11-1 presents additional information on antihistamines.
![]() Table 11-1
Table 11-1
| GENERIC NAME | TRADE NAME | COMMENTS |
| FIRST GENERATION DRUGS | ||
| Alkylamines | Effective at low dosages, practical for daytime use; may cause both CNS stimulation (excitation) and depression (drowsiness); individual response varies | |
| brompheniramine | P-Tex Dimetapp |
|
| chlorpheniramine | Chlor-Trimeton | Low incidence of side effects; available OTC; sustained-release forms not for use in children younger than 6 yr |
| dexchlorpheniramine | Polaramine |
|
| Ethanolamines | Highest incidence of drowsiness, but GI side effects are infrequent | |
| Clemastine | Tavist | |
| diphenhydramine | Benadryl Genahist Diphenhist Banophen |
Anticholinergic, antitussive, antiemetic, and sedative properties; high incidence of CNS depressant effects; drowsiness increases with use |
| Phenothiazine | Strong CNS depressant effect (drowsiness); may suppress cough reflex or mask signs of intestinal obstruction, brain tumor, or overdosage from toxic drugs (see additional information on phenothiazines in third section of this chapter). Comes as oral, parental, rectal preparations. | |
| promethazine | Phenergan | High incidence of side effects, including severe drowsiness; potent drug with prolonged action; use cautiously in ambulatory patients |
| Piperazine | ||
| hydroxyzine | Vistaril | For pruritus, sedation, adjunct to analgesia, antiemetic |
| Miscellaneous | ||
| azelastine | Astelin nasal spray | For SAR; avoid spraying in eyes |
| SECOND-GENERATION DRUGS | ||
| Piperidines | ||
| azatadine | Optimine | For SAR and PNAR. Comes as a spray |
| cetirizine | Zyrtec | For SAR and PAR; safe for patients with hypersensitivity to hydroxyzine |
| May be taken with or without food | ||
| Patients with renal or hepatic dysfunction require smaller doses | ||
| cyproheptadine | Periactin | For SAR, PAR, and hypersensitivity reactions |
| fexofenadine | Allegra | For SAR; analogue of terfenadine (Seldane) but not associated with cardiac dysrhythmias |
| Allegra D | Patients with renal dysfunction require special dosing | |
| Watch for problems common to decongestants. | ||
| loratadine | Claritin | Place rapidly disintegrating tablets under the tongue |
| Claritin D | Patients with renal or hepatic dysfunction require special dosing every other day. Watch for problems common to decongestants. | |
n Evaluation
The therapeutic effects of antihistamines should decrease the allergy symptoms. Watch for any adverse reactions, which are common but usually mild. Antihistamine use in children and infants is discussed in the Lifespan Considerations box.
Older adult patients are more likely to develop side effects such as dizziness, syncope (light-headedness and fainting), confusion, dyskinesia (difficulty in movements of the body), and tremor. These are called extrapyramidal reactions. Considerations for antihistamine use in older adults are discussed in the Lifespan Considerations box.
The respiratory tract may become dry and mucus may thicken when using an antihistamine. Unless there is some reason for a fluid restriction, the patient should be encouraged to drink large amounts of water to thin secretions and keep the mucous membranes moist.
If any skin reactions occur, the patient should stop taking the drug at once and notify the health care provider. The CNS depressant effects of antihistamines may be increased if the patient takes more than the recommended dosage or drinks alcohol while using the product. This could be dangerous.
n Patient and Family Teaching
Antitussives
Overview
Drugs used to relieve coughing are called antitussives. These drugs may either: (1) act centrally on the cough center in the brain, (2) act peripherally by anesthetizing stretch receptors in the respiratory tract, or (3) act locally, primarily by soothing irritated areas in the throat. Products vary in their effectiveness. Antitussives are commonly com-bined with other drugs and are usually sold as OTC drugs. Antitussives containing controlled substances and usually require a prescription, although some states may allow codeine combination products to be sold OTC if the patient signs for them.
Action
The main action of an antitussive depends on whether an opioid antagonist is included. Narcotic or opioid antitussives suppress the cough reflex by acting directly on the cough center in the medulla of the brain. Nonopioid antitussives reduce the cough reflex at its source by anesthetizing stretch receptors in respiratory passages, lungs, and pleura, and by decreasing their activity.
Uses
Antitussives are used for the relief of overactive or nonproductive coughs.
Adverse Reactions
Adverse reactions to antitussives include constipation, drowsiness, dry mouth, nausea, and postural hypotension (low blood pressure resulting in dizziness when a person suddenly stands up).
Drug Interactions
Opioid antitussives have an additive effect with other CNS depressants, so the dosage should be reduced. Most antitussives increase the analgesic effect of aspirin, which may be helpful.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including allergy to antitussives, presence of COPD that may influence the patient’s response to an opioid, possibility of pregnancy, and the use of other drugs or alcohol that may cause drug interactions. These conditions may be contraindications or precautions to the use of antitussives.
Ask about a history of a nonproductive cough or a prolonged and productive cough, which may keep the patient awake at night or cause muscular pain.
n Diagnosis
Take care to learn why the patient has a productive cough. Signs of infection, allergy, or other problems might suggest the source of the cough.
n Planning
Patients with hypersensitivity (allergy) to these drugs or patients with COPD who have problems with breathing are not usually given opioid antitussives. Opioid antitussives may cause drug dependence. Some of the antitussives are Schedule II controlled substances.
These preparations may cause drowsiness, so the patient should be cautioned to avoid tasks requiring alertness after taking the medication.
n Implementation
Antitussives come only in oral forms. They should be used only for short periods. Short therapy decreases the risk of rebound symptoms from prolonged use or the possibility of addiction to opioid products.
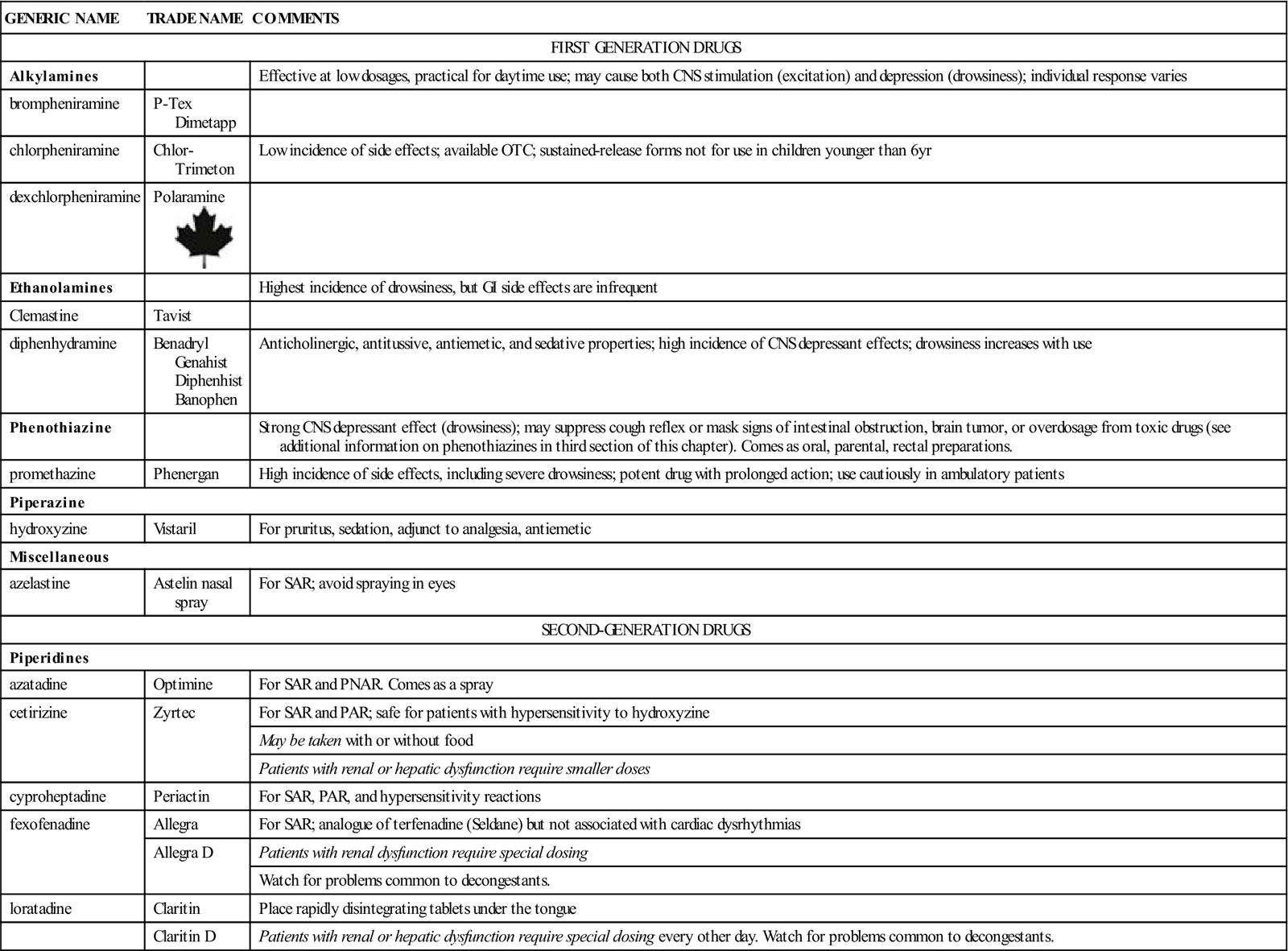
Table 11-2 provides additional information on antitussives.
![]() Table 11-2
Table 11-2
| GENERIC NAME | TRADE NAME | COMMENTS |
| Opioid Antitussives | ||
| codeine |
NOT FOR USE IN CHILDREN YOUNGER THAN 12 YEARS | |
| codeine phosphate | ||
| codeine sulfate | ||
| hydrocodone | Hycodan | |
| Nonopioid Antitussives | ||
| benzonatate | Tessalon Perles (capsules) | Anesthetizes stretch receptors; drug should not be chewed—local anesthesia of the mouth will develop |
| dextromethorphan | Benylin DM | Centrally depresses cough center |
| Robitussin DM | ||
| Vicks Formula 44 | ||
| diphenhydramine |
Tusstat | Potent antihistamine; safe and effective antitussive |
![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
Watch for therapeutic effects: the cough stops or there is a decrease in frequency and duration of coughing spells, and the patient is able to sleep better at night. Also watch the patient for adverse reactions and drug tolerance.
n Patient and Family Teaching
Asthma Medications 
Overview
Asthma is a condition in which there is increased airway inflammation and mucus production, leading to bronchiolar constriction or narrowing. The patient has no trouble breathing air into the lungs, but the lumens (spaces inside the bronchial tubes) become smaller as the patient attempts to breathe out. This traps air inside the lungs. The patient feels a lack of oxygen and acts by breathing faster, trapping even more air inside the lungs. As some air is forced out through the small, mucus-lined passages during respiratory expiration, a musical respiratory sound called wheezing is heard.
The development of asthma involes the interplay between host factors, particularly genetics, deficiencies of some respiratory enzymes, and environmental exposures (reaction to an allergy, reflex response to cold, dry air, or hard exercise). For some individuals with a genetic tendency, asthma often starts in childhood. For some individuals, it becomes a chronic condition. For others, asthma may be seen only with acute illnesses or exercise.
The National Heart, Lung, and Blood Institute of the National Institutes of Health has published Guidelines for the Diagnosis and Management of Asthma. These guidelines recommend a stepwise plan for using asthma drugs that puts a heavy emphasis on the treatment based on the diagnostic classification. Asthma is grouped into classes of asthma severity. These classes are: (1) intermittent, (2) mild persistent, (3) moderate persistent, and (4) severe persistent. In each category, the severity and frequency of daytime symptoms, nighttime symptoms, and lung function are evaluated. The health care provider should work with the patient on prevention, identification of allergens, patient education regarding self-care, and effects of cultural and ethnic influences on asthma management. Because asthma is primarily a disease of inflammation, corticosteroids (both oral and inhaled) are also used in treatment. Some of the steroids used in treating respiratory problems are discussed briefly here and in greater detail in Chapter 20.
COPD is a slowly worsening, disabling disorder identified by abnormal tests of expiratory flow (air that is breathed out) that do not change very much over several months. The damage to the lungs results from gradual destruction of the alveolar walls (small airway disease), and parenchymal destruction, creating unequal areas of ventilation and perfusion. Thus circulating blood and inhaled air may not come together so that oxygen can be transferred to the blood, and waste products in the blood can be removed. COPD attacks or exacerbations are seen with increases in inflammation from pulmonary infections and in response to pollution and allergic or nonallergic triggers. Unlike patients with asthma, those with COPD are seldom symptom free, and the damage to the lungs is not totally reversible with COPD. Medications that dilate or open the bronchioles and help thin secretions are helpful in reducing symptoms of dyspnea (shortness of breath, difficulty or distress in breathing).
Asthma Prophylaxis (Prevention) Medication
Action
Many drugs treat the symptoms of asthma but few of them prevent the development of it. Cromolyn sodium is an asthma prophylaxis drug that works at the surface of the mst cell as a mast cell stabilizer to prevent the release of histamine, leukotrienes, and slow-reacting substances of anaphylaxis.
Uses
Cromolyn is used to manage bronchial asthma in some patients. How this drug should be used is clearly described in the national guidelines. This drug has no independent, antiinflammatory, or bronchodilator activity, so they are effective primarily for prophylaxis (prevention of or protection against disease) and should not be used in an acute attack of asthma. They are also used in some patients with food allergies to prevent GI and systemic reactions; in patients with allergic rhinitis, eczema, and other forms of dermatitis; for patients with chronic urticaria; and for those with exercise-induced bronchospasm (narrowing or collapse of bronchial airways). The different formulations have different uses. A nasal inhalation (NasalCrom) of the drug is used in the treatment of the nasal symptoms associated with allergic rhinitis including runny/itching nose, sneezing, and allergic nasal congestion; and for allergic rhinitis prophylaxis. As an ophthalmic product it is used for the treatment of allergic ocular disorders such as allergic conjunctivitis, allergic keratoconjunctivitis, giant papillary conjunctictivitis, vernal keratitis, and veral keratoconjunctivitis or the product Gastrocrom is used in the treatment of systemic mastocystosis, and chronic inflammatory bowel disease such as ulcerative colitis.
Adverse Reactions
Adverse reactions to cromolyn include dizziness, headache, vertigo (feeling of dizziness or spinning), rash, nausea, bad taste in the mouth, throat irritation, damage to teeth, dysuria (painful urination), urinary frequency, bronchospasm, cough, nasal congestion, wheezing, anaphylaxis, tearing of eyes, and swollen parotid glands. Because these drugs are rapidly eliminated from the body, they are nontoxic, except to those who have a hypersensitivity to the drug.
Drug Interactions
No drug interactions with cromolyn have been reported.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including specific respiratory signs and symptoms, other medications, allergy, possibility of pregnancy, and presence of infection.
The patient may have a history of allergies, asthma, bronchitis, emphysema, recurrent acute or chronic attacks of wheezing, cough with or without mucoid sputum, dyspnea, fatigue, intolerance to exercise, and in severe cases, cyanosis (bluish color to the skin). Acute upper or lower respiratory tract infections may precede the onset of acute symptoms.
n Diagnosis
Confirm that the patient’s condition is stable. These products are not effective in an acute asthma attack. The patient should have no signs or symptoms of illness.
n Planning
The patient should begin taking these drugs when an acute attack of asthma is over, the airways are clear, and the patient can breathe easily.
The amount of drug the lungs are able to use depends on proper use of the nebulizer or if using an inhaler with spacer, the degree of bronchospasm present, and the amount of secretions in the tracheobronchial tree. It has been estimated that approximately 5% to 10% of the inhaled drug reaches the lungs using a standard inhaler. A spacer will increase this percentage.
n Implementation
Cromolyn is taken by standard inhaler. Two inhalations four times daily at regular intervals is the standard regimen.
Occasionally, cough and bronchospasm may follow administration of cromolyn. Some patients may not be able to continue using this drug, even when taking bronchodilators at the same time.
Patients must be careful when decreasing the dosage or stopping the use of cromolyn or nedocromil; this decrease in dosage can cause asthmatic symptoms to recur.
Gastrocrom is an oral concentrate which should be emptied into a half glass of water. Do not mix the solution with fruit juice, milk, or food. Medicine should be taken at least 30 minutes before meals and at bedtime.
n Evaluation
Symptoms of asthma should improve within 4 weeks of using cromolyn or nedocromil. The therapeutic effect is shown when the frequency of asthma attacks decrease and the intensity of the episodes lessen. Because the drug should be given when a patient’s condition is stable, a visit is typically scheduled 2 weeks after the first dose and at least once more within the first 4 weeks to see how effective the medication has been.
Watch the patient carefully when the dose is being reduced or stopped. The drug regimen must be checked if there is no effect within 4 weeks.
n Patient and Family Teaching
Bronchodilators
Several types of bronchodilators may be given to open the bronchi and allow air to pass out of the lungs more freely; these include the sympathomimetics and the xanthine derivatives. The sympathomimetics are beta-adrenergic agents, and they dilate the bronchi through their action on beta-adrenergic receptors. They are also known as adrenergic stimulants. The xanthines act directly to relax the smooth muscle cells of the bronchi, thereby dilating or opening up the bronchi.
Sympathomimetics
Action
The main action of sympathomimetic bron-chodilators like albuterol (Vospire ER, Preventil HFA) in asthma and other respiratory diseases is to relax the smooth muscle cells of the bronchi by stimulating beta2-adrenergic receptors. Sympathomimetic bronchodilators also stimulate beta1 receptors, which results in an increased rate and force of the heart’s contractions. The sympathomimetic drugs vary in their actions on beta receptors. Some act primarily on beta1 receptors that are considered cardioselective; others act primarily on beta2 receptors, and others have beta1 and beta2 effects. If the drug action is specific to beta2 receptors, there are fewer side effects.
Uses
Rapid-acting beta 2 agonists are used to prevent or treat symptoms of bronchospasm occurring in acute and chronic asthma, bronchitis, and emphysema (COPD). Longer-acting beta2 agonists are given twice daily for the long-term treatment of asthma and emphysema. They are also useful in the prevention of nocturnal asthmatic attacks. Longer-acting beta2 agonists are not indicated for the treatment of acute bronchospasm.
Adverse Reactions
Adverse reactions to sympathomimetic bronchodilators include symptoms related to stimulation of other beta receptors throughout the body: dysrhythmias (irregular heartbeats), hypotension, tachycardia, anorexia, anxiety, headache, insomnia, nausea, pallor, perspiration, polyuria (excretion of a large amount of urine), restlessness, vomiting, weakness, and urinary hesitancy and retention. These symptoms get worse if there is an over dose.
Drug Interactions
Drug interactions may occur with MAO inhibitors, tricyclic antidepressants, beta blockers (beta adrenergic antagonists), other antihypertensive agents, digoxin, potassium-losing diuretics, and caffeine-containing herbs The combination of two or more of these agents may produce an additive effect.
Many general anesthetics may cause dysrhythmias when they are used with these drugs. Nonselective beta blockers and beta-adrenergic blocking agents such as propranolol (Inderol) may block the bronchodilating effects of these beta receptor–stimulating drugs. Sympathomimetics can interfere with the action of some antihypertensive medications.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as you can about the health history of the patient, including whether the patient is pregnant or breastfeeding or has a history of hyperthyroidism, heart disease, hypertension, diabetes, glaucoma, seizures, or psychoneurotic disease. Ask whether the patient is taking other drugs that may interact with bronchodilators or has a history of allergy. Any of these conditions may present contraindications or precautions to the use of sympathomimetic bronchodilators.
The patient may have a history of allergies, asthma, bronchitis, emphysema, recurrent acute or chronic attacks of wheezing, and cough. The patient may have had an acute upper or lower respiratory tract infection before the onset of acute symptoms.
n Diagnosis
As you work with the patient, you will confirm that the patient is having an asthma attack or has respiratory difficulty from COPD. The asthma pattern shows the severity of asthma, and national treatment guidelines suggest that the severity of asthma determines the treatment. For example, the first-line therapy for any asthma attack is a short-acting beta2 agonist. In addition, you may discover the patient needs hydration, strategies to reduce anxiety, or education about the condition.
n Planning
To relieve bronchial spasm, beta2 receptors in bronchial smooth muscle cells must be stimulated. One of the drawbacks of beta2 adrenergic bronchodilators is that their effects are not limited to beta2 receptors. Some agents also stimulate beta1 receptors, which increase the rate and force of cardiac contraction.. Thus these beta2 bronchodilator drugs should be given with extreme caution to individuals who already have cardiovascular, endocrine, or convulsive disorders that may be affected by these drugs.
n Implementation
The routes of administration of bronchodilators vary, according to how sick the patient is (the diagnostic classification) and the preparation to be used. Drugs may be given parenterally, orally, or by oral inhalation (nebulizers, or metered-dose inhalers [MDIs]). The medications selected depend on established guidelines and whether short-term treatment or long-term management is required. A patient who is using an inhaler for the first time should be shown how to use the inhaler and given written instructions to refer to later. Research shows that many patients do not use inhalers correctly, so every time the patient comes in for health care, the nurse should ask for a demonstration of how the MDI is being used.
Use of more than one sympathomimetic agent at a time is contraindicated although a rapid-acting drug might be used when a long-acting drug taken on a regular basis is not effective
With many bronchodilators, if the drug is used too frequently, refractoriness, or lack of response to a drug that a patient has used before with good effectiveness, may develop. Patients also may get less relief from aerosols if they are used too often. Irritation of the bronchial tree and oropharynx may occur with use of powdered drug forms or other inhalted agents. Rinsing the mouth with water after each treatment helps reduce this problem.
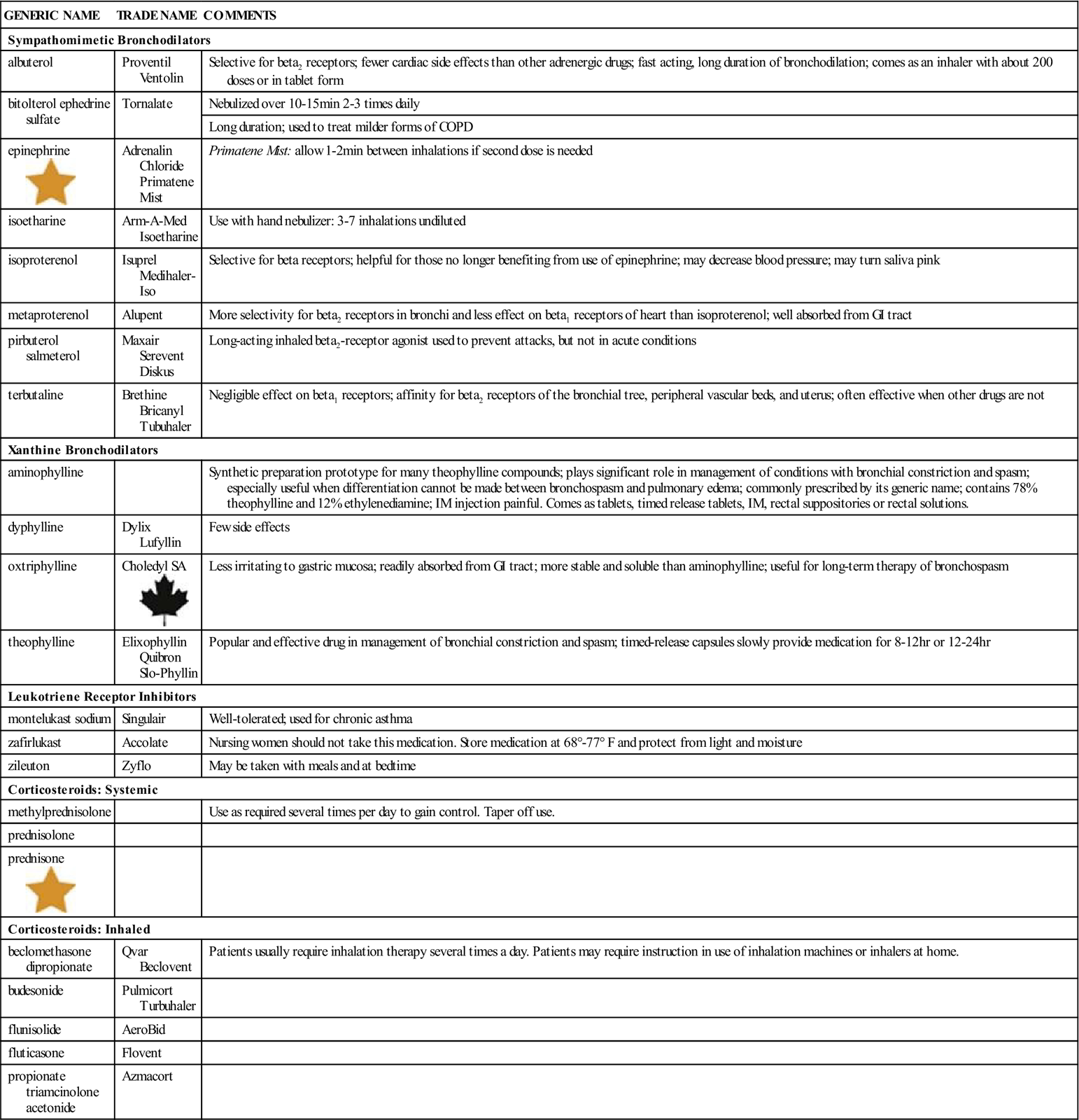
Table 11-3 provides a list of sympathomimetics and other medications used for the treatment of asthma and COPD.
![]() Table 11-3
Table 11-3
Medications for Asthma and Chronic Obstructive Pulmonary Disease
| GENERIC NAME | TRADE NAME | COMMENTS |
| Sympathomimetic Bronchodilators | ||
| albuterol | Proventil Ventolin |
Selective for beta2 receptors; fewer cardiac side effects than other adrenergic drugs; fast acting, long duration of bronchodilation; comes as an inhaler with about 200 doses or in tablet form |
| bitolterol ephedrine sulfate | Tornalate | Nebulized over 10-15 min 2-3 times daily |
| Long duration; used to treat milder forms of COPD | ||
| epinephrine |
Adrenalin Chloride Primatene Mist |
Primatene Mist: allow 1-2 min between inhalations if second dose is needed |
| isoetharine | Arm-A-Med Isoetharine | Use with hand nebulizer: 3-7 inhalations undiluted |
| isoproterenol | Isuprel Medihaler-Iso | Selective for beta receptors; helpful for those no longer benefiting from use of epinephrine; may decrease blood pressure; may turn saliva pink |
| metaproterenol | Alupent | More selectivity for beta2 receptors in bronchi and less effect on beta1 receptors of heart than isoproterenol; well absorbed from GI tract |
| pirbuterol salmeterol |
Maxair Serevent Diskus |
Long-acting inhaled beta2-receptor agonist used to prevent attacks, but not in acute conditions |
| terbutaline | Brethine Bricanyl Tubuhaler |
Negligible effect on beta1 receptors; affinity for beta2 receptors of the bronchial tree, peripheral vascular beds, and uterus; often effective when other drugs are not |
| Xanthine Bronchodilators | ||
| aminophylline | Synthetic preparation prototype for many theophylline compounds; plays significant role in management of conditions with bronchial constriction and spasm; especially useful when differentiation cannot be made between bronchospasm and pulmonary edema; commonly prescribed by its generic name; contains 78% theophylline and 12% ethylenediamine; IM injection painful. Comes as tablets, timed release tablets, IM, rectal suppositories or rectal solutions. | |
| dyphylline | Dylix Lufyllin |
Few side effects |
| oxtriphylline | Choledyl SA |
Less irritating to gastric mucosa; readily absorbed from GI tract; more stable and soluble than aminophylline; useful for long-term therapy of bronchospasm |
| theophylline | Elixophyllin Quibron Slo-Phyllin |
Popular and effective drug in management of bronchial constriction and spasm; timed-release capsules slowly provide medication for 8-12 hr or 12-24 hr |
| Leukotriene Receptor Inhibitors | ||
| montelukast sodium | Singulair | Well-tolerated; used for chronic asthma |
| zafirlukast | Accolate | Nursing women should not take this medication. Store medication at 68°-77° F and protect from light and moisture |
| zileuton | Zyflo | May be taken with meals and at bedtime |
| Corticosteroids: Systemic | ||
| methylprednisolone | Use as required several times per day to gain control. Taper off use. | |
| prednisolone | ||
| prednisone |
||
| Corticosteroids: Inhaled | ||
| beclomethasone dipropionate | Qvar Beclovent |
Patients usually require inhalation therapy several times a day. Patients may require instruction in use of inhalation machines or inhalers at home. |
| budesonide | Pulmicort Turbuhaler | |
| flunisolide | AeroBid | |
| fluticasone | Flovent | |
| propionate triamcinolone acetonide |
Azmacort | |
GI, Gastrointestinal; IM, intramuscular.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
Check the patient’s pulse and blood pressure to see if the heart is affected by the drug. Response to therapy varies among patients. The patient should be watched carefully to see if breathing problems have improved.
Patients should be watched for the development of tolerance, which is shown by less response to the drug.
n Patient and Family Teaching
Tell the patient and family the following:
• Overuse of these drugs may result in severe side effects.
• The health care provider should be contacted if the drug is not helping the patient.
• The drug should be protected from light; colored solutions should be thrown away.
• Give oral medications with meals to minimize gastric irritation.
• Tell patient to shake the inhaler well before administering.
• Patient should rinse their mouth with water after each administration to decrease dry mouth.
Xanthine Derivatives
Action
The main action of xanthine-derivative bronchodilators such as aminophylline and theophylline (Theo-24) is to relax the smooth muscle cells in the bronchi and blood vessels in the lungs. These drugs also act directly on the kidneys to produce diuresis (increased production and excretion of urine). These drugs cause CNS effects. Other actions are myocardial stimulation, increased rate of breathing, effects on metabolism, and release of epinephrine from the adrenal medulla.
Uses
Xanthine derivatives are used as an alternative or adjunctive therapy to treat the symptoms of bronchospasm in acute and chronic bronchial asthma, bronchitis, and emphysema and in treating neonatal apnea. The correct way to use them is carefully described in the National Institutes of Health Guidelines for the Diagnosis and Management of Asthma (available at http://www.nhlbi.nih.gov/guidelines/asthma/index.htm).
Adverse Reactions
Adverse reactions to xanthine derivatives include dysrhythmias, flushing, marked hypotension, tachycardia, headache, insomnia, restlessness, diarrhea, epigastric pain, nausea, vomiting, and rash.
Overdosage causes serious adverse reactions that increase in severity, including confusion, respiratory failure, shock, bizarre behavior, extreme thirst, deliruium (extreme confusion, often with delusions or disorientation), and hyperthermia (abnormally high body temperature). Excessive overdosage may lead to seizures and death without warning. Children are particularly at risk for this problem.
Drug Interactions
Xanthines may increase the CNS stimulation caused by ephedrine, sympathomimetics, and amphetamines. Cytochrome P-450 interactions between xanthines and erythromycin, lincomycin, and clindamycin may increase blood levels of theophylline. Beta-blocking agents may interfere with (antagonize) the effect of xanthines. Xanthines also increase the action of some types of diuretics. Xanthines may increase the risk of toxicity when taken with digitalis glycosides. Large doses of these agents may reverse the effect of oral anticoagulants. Lithium carbonate is excreted more rapidly in the presence of xanthines. The use of furosemide with theophylline increases the serum levels of theophylline and may cause toxicity. Xanthine derivatives shorten prothrombin and clotting times.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including whether the patient is pregnant or has a history of smoking, allergy, renal or liver dysfunction, heart disease, cardiac dysrhythmias, peptic ulcer, severe hypertension, or glaucoma. These conditions are contraindications or precautions to the use of xanthines.
n Diagnosis
The severity of asthma or COPD is determined by history and is linked to the treatment. Look for any other problems that may require your help: need for increased hydration, insomnia, or feelings of anxiety.
n Planning
The half-life of xanthine bronchodilators is shorter in smokers than in nonsmokers, which may make it necessary to use a higher dosage for smokers.
Some xanthine bronchodilators come in a liquid formulation with alcohol. It is not necessary to use drug formulations that contain alcohol; the addition of alcohol may be harmful to some patients.
n Implementation
Xanthine products are available in a number of forms: capsules, sustained-release tablets and capsules, aqueous solutions and suspensions, hydroalcoholic elixirs, suppositories, rectal solutions, and IV and IM injections.
The amount of the theophylline base varies in xanthine products, and the preparations are not therapeutically equal. This inequality may cause difficulty when the patient is switched from one product to another. The health care provider will want to get blood theophylline levels to make sure that the patient is getting the right amount of medicine.
The rate of absorption of oral theophylline depends on the dosage form used. Oral liquids have the fastest absorption rate, followed by uncoated tablets. Sustained-release tablets and capsules produce inconsistent blood levels and should usually be used only at night. Food does not influence the absorption of theophylline. Absorption of rectal suppositories is slow and sometimes unpredictable. The rate of absorption for rectal solutions and IM injections is usually equivalent to that of an oral solution.
The rates of metabolism and excretion of theophylline are also variable. Xanthines are metabolized in the liver and excreted by the kidneys. The serum half-life of the drugs can range from 3 to 12 hours in adults and  to 9 hours in children. Heart failure, liver dysfunction, and pulmonary edema can slow excretion, and smoking can increase excretion. Children younger than 9 years of age actually require larger doses of theophylline than adults to maintain the same therapeutic blood levels of the drug. Thus the dosage must be prescribed on an individualized basis and be carefully monitored. It is common for an initial loading dose to be indicated.
to 9 hours in children. Heart failure, liver dysfunction, and pulmonary edema can slow excretion, and smoking can increase excretion. Children younger than 9 years of age actually require larger doses of theophylline than adults to maintain the same therapeutic blood levels of the drug. Thus the dosage must be prescribed on an individualized basis and be carefully monitored. It is common for an initial loading dose to be indicated.
Because of the need to increase or decrease the amount of medication based on the symptoms as well as the serum drug levels, the use of fixed-combination bronchodilator products (that is, a sympathomimetic, a xanthine, and an expec-torant combined in one product) is not recom-mended. Fixed-combination products do not make it possible to change the doses of each individual drug, and a fixed-combination drug may lead to toxicity from some of the drugs. Use of selected sympathomimetic and xanthine bronchodilators administered at the same time, however, may have a synergistic effect. These combination products, once common, are rarely used today.
For more information about the xanthine derivatives, see Table 11-3.
n Evaluation
The patient’s breathing status and symptoms should be watched for any change. Be alert for signs of toxicity, such as tachycardia or dysrhythmias, vomiting, dizziness, and irritability. Therapeutic blood levels of theophylline and the amount of theophylline base in each preparation will affect the patient’s clinical response.
Children and older adult patients are highly sensitive to these drugs and should be carefully watched for CNS stimulation. Notify the health care provider if you suspect the drug dosage may need to be changed.
To minimize GI symptoms, administer the drug with food and water. Rectal irritation may develop from use of suppository forms.
n Patient and Family Teaching
Leukotriene Receptor Inhibitors
Action
The leukotriene receptor inhibitors such as montelukast (Singulair), zafirlukast (Accolate), and ziluton (Zyflo CR) belong to the newest category of drugs used in treating asthma. These drugs are not bronchodilators but act to block receptors for the cysteinyl leukotrienes C4, D4, and E4. Cysteinyl leukotrienes (leukotrienes bound to the amino acid cysteine) are potent bronchoconstrictors. By blocking receptors that control bronchoconstriction, vascular permeability, and mucus secretion, the leukotriene receptor inhibitors can reduce the symptoms of asthma.
Uses
These products are substitutes for inhaled glucocorticoid therapy in patients with mild, persistent asthma who cannot take the inhaled medications. These drugs may also be added to regular therapy, because they have a different type of action. They provide medication options for patients with aspirin sensitivity. They are used for prevention and chronic asthma therapy, management of seasonal allergic rhinitis, prevention of exercise-induced bronchoconstriction in patients who are 15 years and older, and may be continued during acute attacks, although they will not reverse bronchospasm.
These drugs are rapidly absorbed orally. While it is often recommended that for pediatric dosing these products be mixed with food, food interferes with the absorption of many of these products, so they should be taken on an empty stomach. The safety of all these drugs has not been established in pregnancy. Montelukast (Singular) and zafirluklast (Accolate) are pregnancy category B(montelukast has dosing for infants from 6 months and zafirlukast has dosing for children from 5 years.) Zileuton (Zyflor CR) is category C and should not be used in breastfeeding mothers or in children younger than age of 10 .
Adverse Reactions
These drugs are generally safe and well tolerated. Headache is the most common side effect. A few individuals may have infection, nausea, and diarrhea. Singulair has quite a few minor side effects, including upper respiratory infection (URI) and otitis media for children.
Drug Interactions
These drugs interact with warfarin, erythromycin, theophylline, MAOIs, sedative/hypnotics, barbiturates, tricyclic antidepressants, antihistamines, phenytoins, atropine/scopolamine, rifampin, and aspirin.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient to determine the status of the patient’s asthma and what other medications the patient might be taking. Ask about the possibility of pregnancy, breastfeeding, or liver disease.
n Diagnosis
Carefully evaluate the patient to determine the possibility of infection, the presence of anxiety (which may cause more rapid breathing), a lack of knowledge, or anything else that may complicate the asthma treatment regimen.
n Planning
These drugs are not started if the patient is having an acute asthma attack. They are adjunctive drugs given as part of an asthma treatment regimen. Watch to see if there might be adverse drug interactions with other medications the patient is taking. Some of these medications involve special storage requirements.
n Implementation
Most of these medications are given once or twice daily. They are usually well tolerated, and no significant problems are associated with them.
See Table 11-3 for specific information on the drugs in this category.
n Evaluation
Therapeutic effect is seen with a reduction in number and severity of asthma attacks. Patients should report to their health care provider if they have an increase in asthma attacks.
n Patient and Family Teaching
Corticosteroids 
Action
Corticosteroids are the most potent (powerful) and consistently effective medications for the long-term control of asthma. Their action on the inflammatory process may account for their effectiveness. They block the reaction to allergens and reduce airway hyperresponsiveness. They inhibit cytokine production, protein activation, and inflammatory cell migration and activation.
Uses
Inhaled corticosteroids such as fluticasone (Flovent HFA) are used in the long-term control of asthma. They are often used to reduce the need for oral corticosteroids. Systemic corticosteroids are often used to get the fastest control of the disease when beginning long-term therapy although the maximum response may take up to 8 weeks. They are also used to speed recovery from moderate to severe episodes and prevent more of these episodes.
Adverse Reactions
Inhaled steroids may produce bronchospasm, cough, dysphonia (hoarseness), and oral thrush. These drugs may also produce CNS and GI side effects. In long-term or high doses, systemic effects such as slowing of growth in children and osteoporosis in adults may occur. Systemic steroids used for a short time may cause many problems, such as brief abnormalities in glucose metabolism, increased appetite, fluid retention, weight gain, mood alteration, hypertension, and peptic ulcer. Long-term use suppresses the adrenal axis and may produce serious and systemic symptoms.
Drug Interactions
The inhaled products have a local effect and do not interact to a great extent with other drugs. However, systemic products interact with many drugs (see Chapter 20). The drugs should be used with caution with antifungals and macrolide antibiotics.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn everything you can about the severity of the patient’s asthma. Look for symptoms of other respiratory infection, allergens, or stress that might have triggered an asthma attack. Collect information about whether the patient takes the asthma medication correctly and as prescribed. Does the patient have other conditions that could be made worse by systemic corticosteroids?
n Diagnosis
Classify symptoms of asthma by severity, and identify asthma triggers. Diagnose needs for patient teaching. Does the patient need to take in more fluids? Does the patient need more education?
n Planning
Develop a teaching plan to meet the educational needs that have been discovered. The health care provider will order oral products at the lowest effective dose for the shortest time possible, so plan to be watchful for adverse effects that may develop from the medication.
n Implementation
Sometimes patients can reverse an asthma attack by controlling their breathing. Patients who learn these techniques may be fearful and unable to breathe slowly when the attack begins. Stay with the patient and offer reassurance and help with breathing exercises during an acute asthmatic attack. Also begin giving the patient extra water to reduce the thickness of secretions and help the patient cough them up and spit them out. Show the patient the proper way to hold the medication canister, take a breath, and compress the canister so that the medication is released into the lungs and not into the mouth. To insure that the medicine is at the proper angle to go into the lungs and not the throat, if the patient can stand, they should be able to see their feet while using the inhaler. (If they cannot see their feet, they are holding the inhaler at the wrong angle). Begin teaching the patient about the disease process, the medication regimen, equipment, and procedures. Using a spacer or holder chamber device and washing out the mouth after inhalation will improve systemic absorption and decrease local side effects.
For more information about these products, see Table 11-3.
n Evaluation
Have the patient show you how the inhaler is used. Watch for improvement in the patient’s breathing. Wheezing should decrease.
n Patient and Family Teaching
Education should focus on the disease process, triggers to asthma attacks, and appropriate therapy.
The patient and family should learn about taking the medicine and knowing when it is not effective. Make sure the patient understands when to contact the health care provider.
Explain how corticosteroid medications are used together with other products. This information should be put in writing so the patient can refer to it later.
Children need to be taught as much as possible and given the responsibility of helping to determine when they need medication, what type of medication they need, and whether it is effective.
Decongestants
Overview
Action
Decongestants directly affect the alpha receptors of blood vessels in the nasal mucosa, causing vasoconstriction. This action reduces blood flow in the edematous nasal area, resulting in decrease of the engorged turbinates and mucous membrane, which will encourage sinus drainage, improve nasal air passage, and relieve the feeling of nasal stffiness and mucosal edema. Many agents also act on beta receptors, which may cause rebound vasodilation, or an increase in blood flow, leading to further congestion. This problem is commonly seen with prolonged use of the medication.
Uses
Decongestants are used to relieve nasal congestion that accompanies allergic rhinitis, sinusitis, and upper respiratory tract infections (URTIs). These drugs may also be used as additional therapy for middle ear infections and to decrease congestion around the eustachian tubes. Ear blockage and the pressure and pain caused by air travel may respond to nasal decongestants. Most of these products are now OTC.
Adverse Reactions
Stinging and burning as a result of mucosal dryness sometimes follow administration via nasal spray of decongestants. Rebound congestion may occur after prolonged use of topical agents. When the drugs are administered orally and absorbed from the GI tract, systemic effects such as nervousness, nausea, dizziness, tachycardia, dysrhythmia, and a transient increase in blood pressure may occur. Rarely, a severe shocklike syndrome with hypotension and coma has been reported in children. Psychologic dependence and toxic psychoses have been reported with long-term, high-dose therapy. The severity of overdosage varies, resulting in a variety of symptoms. Because of problems with inadvertent overdosage in infants and toddlers, the makers of all OTC oral cough and cold products announced in 2007 that they would remove these products from the market. This action proceeded from Food and Drug Administration regulations that these products are not to be used in infants and toddlers.
Drug Interactions
The systemic effects of decongestants may be made stronger if they are given with other sympathomimetics, MAO inhibitors, tricyclic antidepressants, antihistamines, and thyroxine. Decongestants should be used with caution in stable hypertensive patients on guanethidine, bethanidine, or debrisoquine sulfate. Use of decongestants at the same time as high doses of digitalis or use of other drugs that may sensitize the heart to dysrhythmias should be avoided because anginal pain may result when there is coronary insufficiency.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the patient’s health history. The patient may have a history of nasal congestion, postnasal drip, nasal discharge, sneezing, sore throat, headache, itchy eyes, lacrimation (excess tear production), nasal polyps, earache, decreased hearing, URTI, or allergies.
Ask about allergy to adrenergic agents, narrow-angle glaucoma, concurrent MAO inhibitor or tricyclic antidepressant therapy, and loss of sensation in the fingers and toes. These are contraindications to the use of decongestants. Decongestants should be used cautiously by patients with hypertension, dysrhythmias, heart disease, angina, hyperthyroidism, diabetes, advanced arteriosclerotic conditions, glaucoma, prostatic hypertrophy, or chronic cough because of the possibility of systemic vasoconstriction and tachycardia. Patients with a long history of asthma and emphysema who also have degenerative heart disease should also be cautioned about the use of decongestants. Excessive use of topical decongestants may result in GI absorption that causes systemic effects. The safe use of decongestants in pregnancy has not been established.
Decongestants should be used with caution in patients with hypertension, hyperthyroidism, diabetes, cardiac disease, glaucoma, or prostatic hyperplasia. Drugs containing pseudoephedrine are used in the manufacture of methamphetamines. Many states have regulations regarding the purchase of decongestants where they track and limit the number of purchases by an individual. The drugs containing decongestants are placed behind the counter at the pharmacy and individuals have to sign for them.
n Diagnosis
To make certain the treatment is appropriate, the exact cause of the patient’s problem must be found. Determine if rhinitis is related to allergy or infection.
n Planning
Frequent and continual use of topical decongestants or use at dosages greater than recommended may result in a rebound effect. Topical decongestants should be used only in acute states, for no longer than 3 to 5 days, and should be used very carefully at low doses in older adults.
n Implementation
Oral decongestants are considered to be more effective and longer lasting than nasal preparations because they can reach all parts of the mucous membrane in the nasal passages. The disadvantage of systemic agents is that their effects may not be limited to the nasal mucosa; they may also affect other parts of the body. This is why caution is advised for patients with certain medical conditions.
Topical forms may be supplied as drops, sprays, jellies, and oral inhalation agents. The advantage of topical administration is the rapid onset of action and direct stimulation of the nasal mucosa. Drops have a tendency to pass into the hypopharynx and then be swallowed, thus passing into the GI tract. Sprays deliver a fine mist that is easily trapped in the upper respiratory tract, so they are less likely to reach the GI tract. Topical preparations should not be used for more than 3 to 5 days because of the risk of a rebound effect. Oral preparations are more appropriate for long-term use in the rare occasions where required.
To prevent swallowing of the drug, the patient’s head should be tipped back when giving nose drops. Use care not to touch the skin while administering solutions. Solutions can become contaminated with use and result in growth of bacteria and fungi.
Table 11-4 lists various nasal decongestant products.
![]() Table 11-4
Table 11-4
| GENERIC NAME | TRADE NAME | COMMENTS |
| Sympathomimetic Bronchodilators | ||
| ephedrine |
Pretz D | May produce burning, stinging, dryness of nasal mucosa, and sneezing |
| epinephrine | Adrenalin | Stimulates both alpha and beta receptors |
| Inhalers | ||
| naphazoline | Privine | Rapid, prolonged effect; produces CNS depression when swallowed |
| oxymetazoline | Afrin Dristan 12 Hr Duration |
Prolonged decongestant effect; often overused by patients, leading to rebound congestion when used longer than 3 days in succession |
| phenylephrine | Neo-Synephrine Sinex |
Drug ineffective if exposed to air, strong light, or heat; very effective topical preparation but may cause marked local irritation |
| pseudoephedrine sulfate | Sinex Sudafed |
|
| tetrahydrozoline | Tyzine | |
| xylometazoline | Otrivin | Overdose can cause extreme CNS depression in children. |
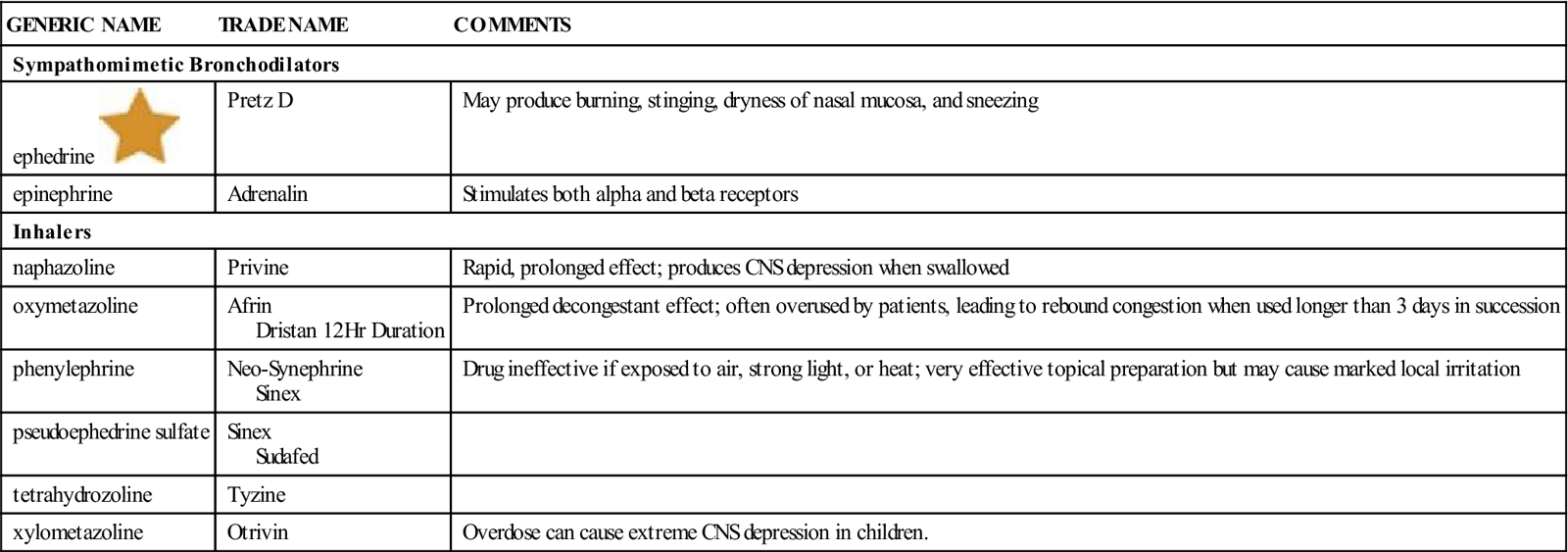
CNS, Central nervous system.![]() Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
Indicates “Must-Know Drugs,” or the 35 drugs most prescribers use.
n Evaluation
Expect to see symptoms disappear. However, symptoms may return if there is rebound congestion following overly long use. If headache and nervousness occur, stop the treatment and contact the health care provider.
n Patient and Family Teaching
There are many decongestants on the market that are available OTC. A lot of these OTC products contain combinations of medications to make them attractive to the patient with several symptoms. These products may contain a decongestant and one or more antihistamine, analgesic, antitussive, expectorant, or anticholinergic products. Each additional medication increases the precautions for use of the product and the adverse effects that may occur. For example, drugs that contain anticholinergics cause drying of mucus secretions. They should be avoided in patients with asthma or COPD. The patient should consider whether there is a need for all of the drugs listed on the label of these combination products. Also, the types of drugs that make up even well-known products change frequently. Pharmacists are excellent sources of information about OTC medications, and patients should be encouraged to seek their professional advice before self-treating with a decongestant product.
Expectorants
Overview
Action
Expectorants are agents that decrease the thickness of respiratory secretions and aid in their removal. It is believed they work by increasing the amount of fluid in the respiratory tract. These thinner secretions promote ciliary action and decrease the amount of coughing while increasing the amount of sputum produced. Guaifenesin has been on the market since the 1950’s but its efficacy has only recently been documented. Guaifenesin is an ingredient contained in many combination OTC cough and cold products. It is available as a single agent in both OTC medications (such as Mucinex, Robitussin, Organidin NR) and in prescription-only products (such as Humibid LA, Touro EX tablets). The drug is available in immediate-release (e.g. oral solutions), extended-release, and combination immediate/extended release formulations. Mucinex was approved in 2002 and is the only FDA-approved OTC extended-release guaifenesin product.
Uses
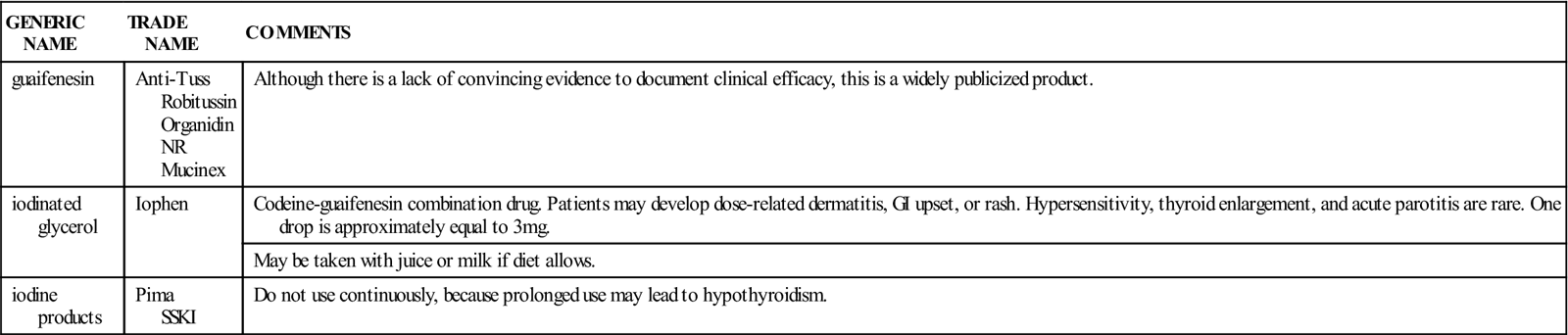
Guaifenesin is used to treat symptoms of productive cough. These products may be useful in chronic respiratory disease when thick mucus is a complication and are indicated in patients with coughs associated with viral URIs. Table 11-5 provides a summary of expectorants. Because of cases of overdosage, the FDA has ruled that these products should not be given to children under 2 years old, and some products not to children under 6 years old. Drug companies have voluntarily removed many of these risky preparations from the market to reduce the potential for inadvertent overdose.
![]() Table 11-5
Table 11-5
| GENERIC NAME | TRADE NAME | COMMENTS |
| guaifenesin | Anti-Tuss Robitussin Organidin NR Mucinex |
Although there is a lack of convincing evidence to document clinical efficacy, this is a widely publicized product. |
| iodinated glycerol | Iophen | Codeine-guaifenesin combination drug. Patients may develop dose-related dermatitis, GI upset, or rash. Hypersensitivity, thyroid enlargement, and acute parotitis are rare. One drop is approximately equal to 3 mg. |
| May be taken with juice or milk if diet allows. | ||
| iodine products | Pima SSKI |
Do not use continuously, because prolonged use may lead to hypothyroidism. |
Adverse Reactions
GI upset is a common adverse reaction to expectorants. Dizziness, headache, and rash may also occur.
Drug Interactions
There are no drug interactions of clinical significance with guaifenesin.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including the history of cough, presence of other respiratory disease, allergy, and other medications that may cause drug interactions.
n Diagnosis
Are there needs for hydration? Is the patient able to take water by mouth, or is he or she receiving IV fluid? Diagnose any lack of knowledge the patient may have.
n Planning
Expectorants are not to be used for persistent cough without the advice of a health care provider.
n Implementation
The patient should take an increased amount of fluid each day and breathe humidified air. This will help liquefy secretions. Medication should be taken with at least one full glass of water. (See Table 11-5.)
n Evaluation
Monitor to see that secretions become thinner and are decreased. If the patient uses more than the recommended dosage, adverse reactions may occur.
n Patient and Family Teaching
Topical Intranasal Steroids
Overview
Action
The main action of topical intranasal steroids is an antiinflammatory effect, which decreases local congestion.
Uses
Topical intranasal steroids such as flunisolide (Nasarel) are used to treat allergic, mechanical, or chemically induced local nasal inflammation or nasal polyps only when the more usual treatment has been tried and found to not work. Some patients get good allergy relief from these products and require no other medications. Although not every patient is able to take these medications, in general the medications have been found to be safe. Some patients have been able to use them for years without adverse or systemic effects.
Adverse Reactions
Adverse reactions to topical intranasal steroids include inducing an asthma attack, headache, light-headedness, loss of sense of smell, nasal irritation and dryness, nausea, nosebleeds, perforation of the nasal septum, bad taste and smell, rebound congestion, and skin rash.
Drug Interactions
Intranasal steroids may interact with many products. Consult the earlier section on corticosteroids for more information.
 Nursing Implications and Patient Teaching
Nursing Implications and Patient Teaching
n Assessment
Learn as much as possible about the health history of the patient, including allergy, fungal infections, tuberculosis, ocular herpes simplex, local infections (especially of the nose, sinus, or throat), and the possibility of pregnancy. These conditions are contraindications or precautions to the use of topical nasal steroids. Ask about the patient’s past experience with and response to nasal sprays.
n Diagnosis
Learn why the patient requires intranasal medication. Identify any other problem secondary to medication use or misuse, such as presence of adverse effects or patient education deficits.
n Planning
The patient receiving topical intranasal steroids should not be given smallpox vaccination or immunizations, because the immunologic response may be decreased. In the patient with latent tuberculosis or reactivated tuberculosis, close observation and possible chemoprophylaxis may be indicated. The effects of these drugs are increased in patients with hypothyroidism and cirrhosis.
n Implementation
The recommended dosage must not be exceeded. The dosage should be decreased when the patient begins to improve.
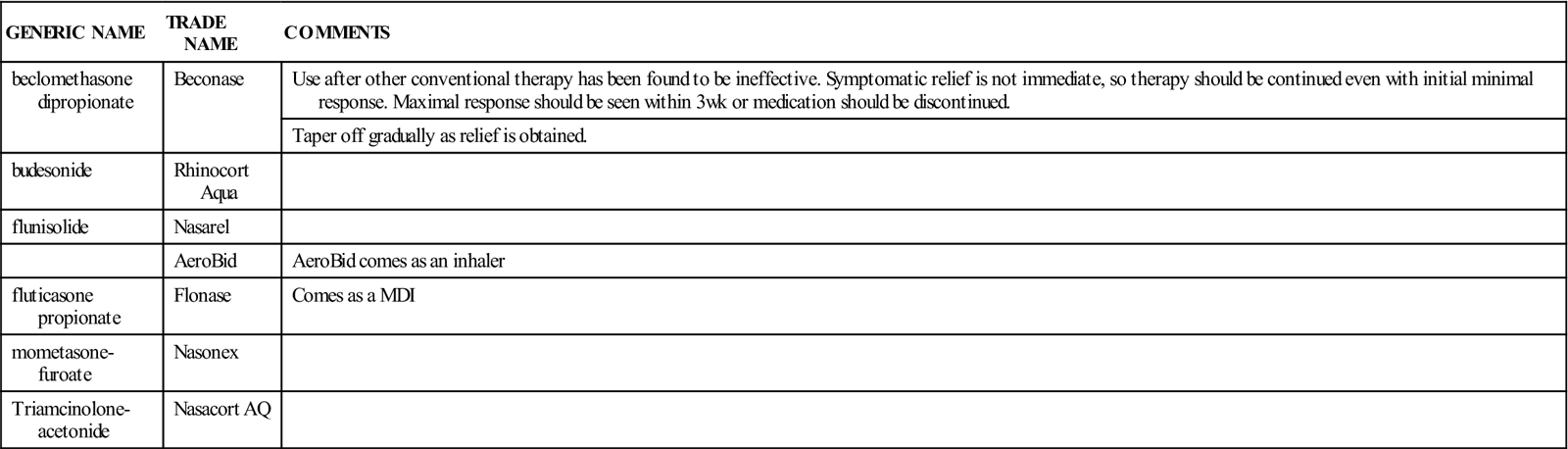
Table 11-6 provides a list of intranasal steroids.
![]() Table 11-6
Table 11-6
| GENERIC NAME | TRADE NAME | COMMENTS |
| beclomethasone dipropionate | Beconase | Use after other conventional therapy has been found to be ineffective. Symptomatic relief is not immediate, so therapy should be continued even with initial minimal response. Maximal response should be seen within 3 wk or medication should be discontinued. |
| Taper off gradually as relief is obtained. | ||
| budesonide | Rhinocort Aqua | |
| flunisolide | Nasarel | |
| AeroBid | AeroBid comes as an inhaler | |
| fluticasone propionate | Flonase | Comes as a MDI |
| mometasone-furoate | Nasonex | |
| Triamcinolone-acetonide | Nasacort AQ |
n Evaluation
Watch for a reduction in nasal stuffiness, obstruction, and discharge, and for relief of sinus headaches. Also monitor how often the medication is used and what dosage is used. Watch for cracked or bleeding nasal mucosa. Be alert for adverse reactions such as signs of systemic absorption and fluid retention, increased blood pressure, weight gain, ankle edema, or evidence of local infection.
Nasal dryness and irritation are side effects and do not usually require stopping the drug. The dosage of these drugs should be gradually reduced to avoid adrenocortical insufficiency.
These drugs may decrease resistance to infection, as well as mask some common signs of infection. Elevation of blood pressure, retention of salt and fluid, and increased potassium and calcium loss may occur if the patient takes large doses. This may be treated with dietary salt restriction and potassium supplementation. Loss of the ability to smell, shortness of breath, unrelieved stuffy nose, chest tightness, or wheezing all indicate a need for intervention by a health care provider.
The patient should be watched for signs of sys-temic absorption, because fluid retention and temporary inhibition of pituitary-adrenal function may develop.
n Patient and Family Teaching
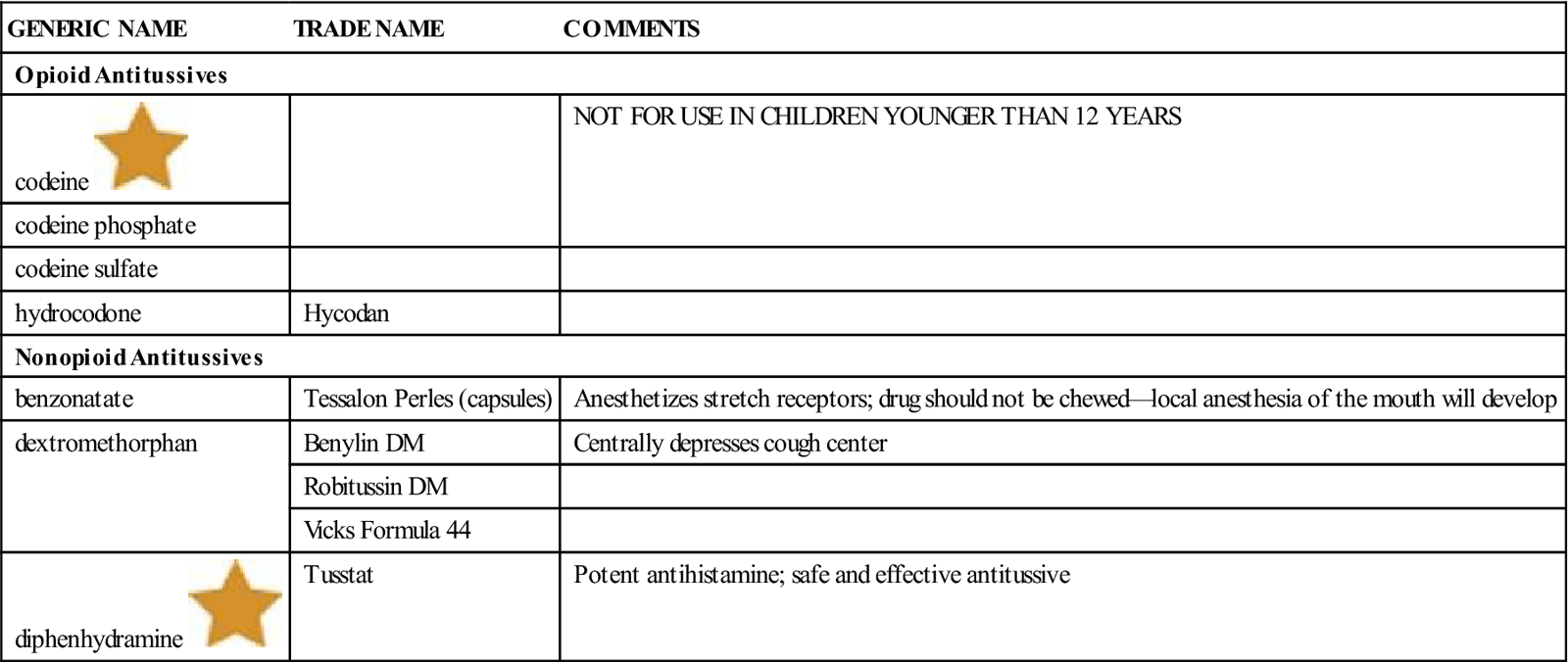
Complementary and Alternative Therapies
Allergies, asthma, and coughs and colds are some of the conditions frequently treated with alternative products. See the Complementary and Alternative Therapies box for some of the most common preparations and their use.