CASE 101
History: A 48-year-old man presents with chronic hepatitis C and cirrhosis.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in Figure A? (Choose all that apply.)
2. What is the usual physiologic basis for the development of uphill varices?
B. Occlusion of the splenic vein
D. Superior obstruction of the vena cava
3. What is the most common cause of upper gastrointestinal bleeding?
4. Where do downhill varices occur?
ANSWERS
CASE 101
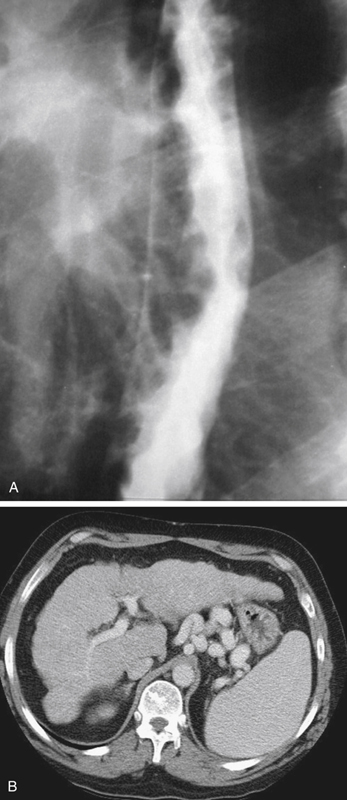
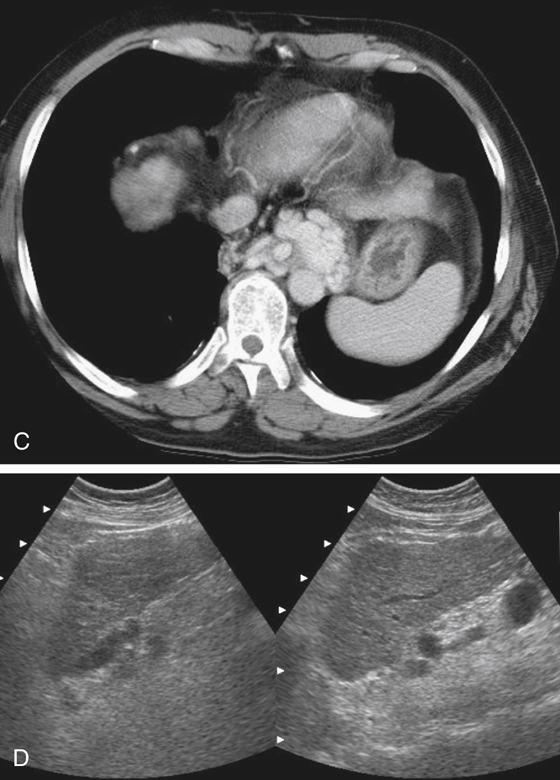
Esophageal Varices
1. B, C, and E
2. A
3. C
4. D
References
Kim SH, Kim YJ, Lee JM, et al: Esophageal varices in patients with cirrhosis: multidetector CT esophagography—comparison with endoscopy. Radiology. 2007;242:759–768.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, p 9.
Comment
In Western society the most common cause of portal hypertension and the formation of esophageal varices is hepatic cirrhosis (see figures). This is usually the result of chronic alcoholism. However, many other causes can lead to liver cirrhosis, especially chronic hepatocellular disease (such as hepatitis), chronic portal vein occlusion by thrombus, or parasitic infection. Chronic portal vein occlusion can also result in cavernous transformation of the portal vein, in which collateralization along the entire route of the former portal vein is seen. This results in less-evident esophageal varices, and indeed, the patient may be asymptomatic. Cavernous transformation in portal hypertension related to liver cirrhosis is uncommon. Esophageal varices can bleed. This most alarming complication of the condition carries a high morbidity rate.
At the other end of the esophagus, obstruction of the superior vena cava can result in downhill varices seen in the upper esophagus and representing prominent collateralization of the venous system in an attempt to bypass an occluded superior vena cava, usually secondary to marked adenopathy resulting from adjacent malignancy, most commonly small cell carcinoma of the lung. Lymphoma can also be the underlying condition. The diagnosis is usually not difficult from the patient’s physical appearance of congested facial features and engorged neck veins.







