CASE 100
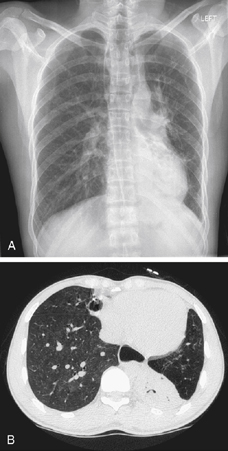

History: A 24-year-old man presents with recurrent episodes of pneumonia.
1. Which of the following should be included in the differential diagnosis of the imaging finding shown in Figures A and B? (Choose all that apply.)
A. Epidermolysis bullosa dystrophica
B. Gastroesophageal reflux disease
C. Distal esophageal obstruction
D. Esophageal motility disorder
2. What is the etiologic basis for primary achalasia?
3. What radiographic finding on barium swallow is most commonly seen and useful to differentiate secondary achalasia due to malignancy from primary achalasia?
A. Narrowed segment nodularity
4. What is the most common etiology of secondary achalasia?
ANSWERS
CASE 100
Achalasia
1. B, C, and D
2. C
3. B
4. A
References
Ott DJ. Motility disorders of the esophagus. In: Gore RM, Levine MS, eds. Textbook of Gastrointestinal Radiology. 2nd ed Philadelphia: WB Saunders; 2000:316–328.
Cross-Reference
Gastrointestinal Imaging: THE REQUISITES, 3rd ed, pp 21-23.
Comment
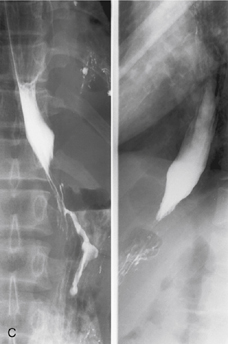
Achalasia is a fairly common but poorly understood disorder of the myenteric plexuses of the esophagus resulting in dilation, absence of peristaltic activity, and spasm at the gastroesophageal junction. It is more common in men and is usually seen in the third or fourth decade of life. In the images accompanying this case, a barium esophagogram demonstrates the classic area of tapered narrowing and spasm in the distal esophagus at the gastroesophageal junction (see figures). With chronic achalasia, the esophagus will over time become grossly dilated, with a sigmoid configuration. This may be confused with the appearance of esophageal resection and gastric pull-up or colonic interposition.
Other conditions, such as scleroderma and other collagen vascular disorders, can mimic achalasia. They are described as secondary achalasia. In these patients, the underlying condition is usually of long standing and well known to the patient. There have been reports of patients with diffuse esophageal spasm with dilated esophagus, minimal peristaltic activity, and spasm at the gastroesophageal junction. In fact, some investigators feel that achalasia and diffuse esophageal spasm may be part of the same spectrum of diseases. Although this is occasionally seen, it is not the usual pattern of presentation seen in most cases of achalasia. Primary and secondary achalasia may be identical in imaging appearance and presentation.
An important and common cause of secondary achalasia occurs where the underlying condition is esophageal or gastric cardiac carcinoma, which has infiltrated the wall of the lower esophagus or gastroesophageal junction and destroyed the myenteric plexuses. This is usually seen in an older age group, with a short history of dysphagia and weight loss. The differentiating feature on a barium swallow may be some mucosal irregularity at the site of spasm, proximal shouldering, or a mass at the gastric cardia. The length of the segment narrowing is a key differentiating feature, with malignant achalasia having a narrow segment greater than 3.5 cm. Endoscopic ultrasound and, in many cases, CT are more sensitive methods for making the diagnosis of secondary achalasia. Some authors refer to this etiology for secondary achalasia as pseudo-achalasia, recognizing that unlike the other secondary causes where the etiology is known, the patient and clinician might not be aware of the underlying malignancy when the patient presents with dysphagia.







