CASE 100
1. Which walls show extensive abnormality? (Choose all that apply.)
A. Anterior
B. Septal
C. Lateral
D. Apical
2. What vascular territory is involved?
A. Left main
D. Right
B. Infarction
C. Myocarditis
4. What is the most appropriate management?
A. No treatment
ANSWERS
Reference
Reddy GP, Pujadas S, Ordovas KG, et al. MR imaging of ischemic heart disease. Magn Reson Imaging Clin N Am. 2008;16(2):201–212.
Cross-Reference
Cardiac Imaging: The REQUISITES, ed 3, pp 74–76.
Comment
Clinical Issues
In a patient with impaired regional function in the left ventricle, determination of viability can be important for management decisions. In the setting of chronic poor functioning, viable but poorly functioning myocardium is termed “hibernating myocardium.” Nonviable myocardium represents infarction. A revascularization procedure such as balloon angioplasty or stent or coronary artery bypass graft surgery can improve contractility in hypofunctioning but viable tissue (hibernating myocardium). However, nonviable myocardium would not benefit from a revascularization procedure.
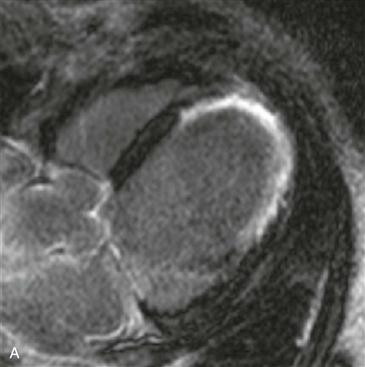
Imaging and Implications for Management
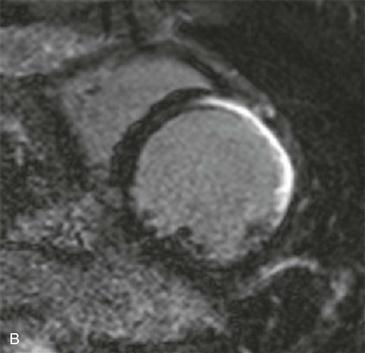
Viability imaging with MRI is performed approximately 10 minutes after intravenous administration of gadolinium chelate contrast medium. The myocardium enhances shortly after administration of the contrast agent, but the agent washes out of viable areas. Only nonviable myocardium enhances on the delayed (10-minute) images (Figs. A and B). Revascularization would not be beneficial if the nonviable area involves more than 50% of the myocardial thickness. However, revascularization may be beneficial if the area of nonviability involves less than 50% of the myocardial thickness (e.g., if it is limited to the subendocardial region). MRI often can distinguish whether the area of nonviability involves greater than or less than 50% of the myocardial wall thickness, an advantage over positron emission tomography (PET) in the determination of viability.