CHAPTER 10 Upper Limb Pain: Shoulder, Elbow, Wrist, and Hand
INTRODUCTION
The wrist and hand are the de facto working units of the upper limb. The shoulder, upper arm, elbow, and forearm form a multijointed lever to place the wrist and hand in an appropriate working position. The hand with its pincer-like thumb serves for grasping and fine manipulation with exquisite sensation and delicate discrimination. The function of the hand is controlled by the brain. The physical activities that the wrist and hand are made to perform render these working units susceptible to accidental injuries and inflammation caused by wear and tear, and most of these injuries may produce pain. The fingers (the digits) are the most mobile parts of the body. The delicate and complex structures of the wrist and hand make recovery of function through acupuncture more difficult than in other parts of the body. However, good results can still be achieved with early treatment.
BASIC ANATOMY OF THE UPPER LIMB AS IT RELATES TO ACUPUNCTURE THERAPY
The Bones of the Upper Limb
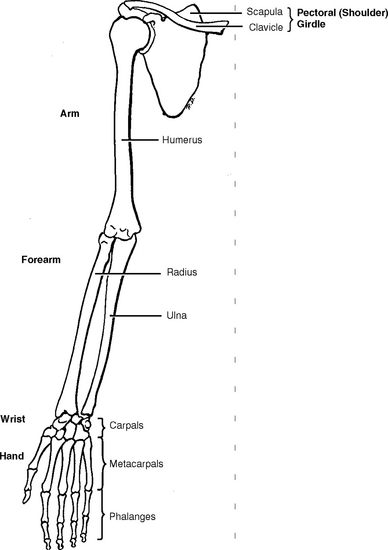
The bones comprising the upper limb include the clavicle (collar bone) and scapula (shoulder blade) in the pectoral girdle; the humerus in the arm; the radius and ulna in the forearm; the eight carpal bones in the wrist; the five metacarpal bones in the hand; and the 14 phalanges in the fingers (digits) (Figure 10-1).
The Brachial Plexus
At the root of the neck, the five anterior rami of the spinal nerves from C5 to C8 and T1 unite to form the brachial plexus in the posterior triangle of the neck. (Remember there are seven cervical spinal vertebrae and eight cervical spinal nerves because spinal nerves C1 and C2 originate from the superior and inferior sides of C1, respectively.) The union of the five anterior rami and the rearrangement of the five cervical spinal nerves allow the nerve fibers derived from different segments of the spinal cord to be arranged and distributed efficiently in different nerve trunks to the various parts of the upper limb. The plexus can be divided into roots, trunks, divisions, and cords (Figure 10-2).
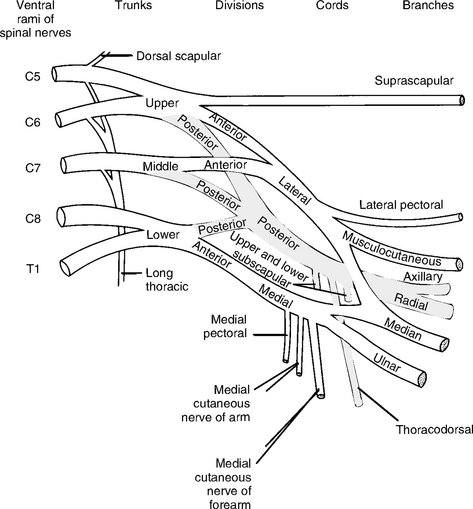
Figure 10-2 Diagram of the brachial plexus.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 80.)
Supraclavicular Branches of the Brachial Plexus
Infraclavicular Branches of the Brachial Plexus
The lateral cord of the brachial plexus includes three branches:
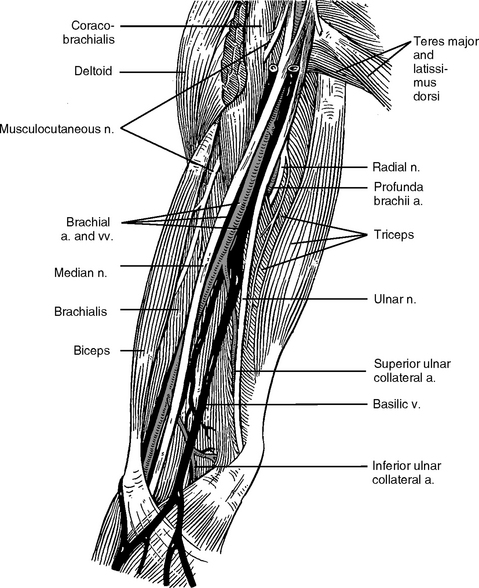
Figure 10-3 Nerves and vessels of the arm. Pay attention to the musculocutaneous nerve.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 125.)
The medial cord of the brachial plexus includes five branches:
Table 10-1 A Summary of Main Innervation of the Ulnar Nerve (C8 and T1)
| Upper Arm | Forearm | Hand |
|---|---|---|
| Elbow joint |
Table 10-2 A Summary of the Main Innervation of the Median Nerves (C5, C6, C7, C8, T1)
| Upper Arm | Forearm | Hand |
|---|---|---|
The posterior cord of the brachial plexus includes five branches:
Table 10-3 A Summary of the Main Innervation of the Radial Nerves (C5, C6, C7, C8, T1)
| Upper Arm | Forearm |
|---|---|
Sympathetic Supply of the Upper Limb
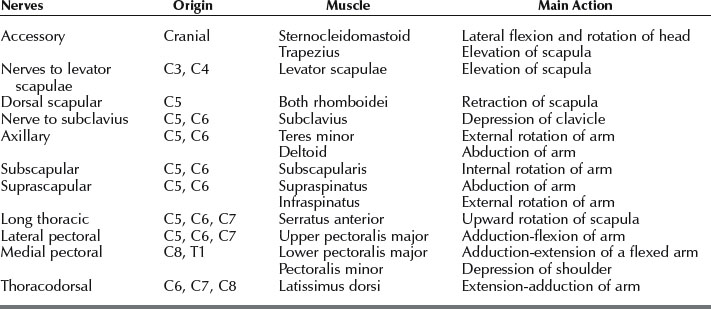
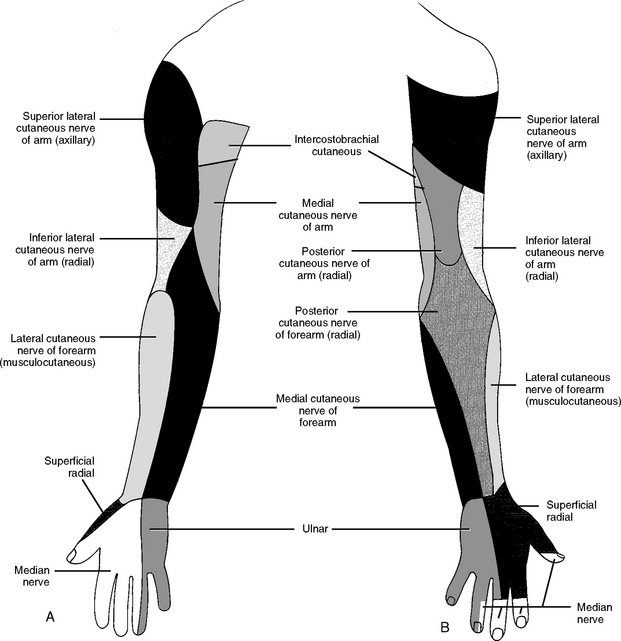
The brachial plexus supplies the cutaneous and muscular nerves of the upper limb (Table 10-4). The cutaneous nerves are responsible for skin sensations such as touch, pressure, pain, heat, cold, or chemical irritation. The muscular nerves control muscle movement, coordinated muscular contraction, and relaxation.
Table 10-4 A Summary of the Main Innervation of the Musculocutaneous Nerve (C5, C6, C7)
| Axilla | Upper Arm | Forearm |
|---|---|---|
| Coracobrachialis |
In addition to the cutaneous and muscular nerves mentioned above, the autonomic nervous system is also important for acupuncture therapy. We have discussed the anatomy of the autonomic nervous system in Chapters 1 and 2. Its purpose is to regulate physiologic functions and it consists of two subdivisions, sympathetic and parasympathetic. The sympathetic system activates emergency or survival-oriented physiologic reactions that include constriction of blood vessels (vasoconstriction) in the skin; sweating; contraction of arrector pili muscles (gooseflesh of the skin); increasing the rate and force of the heart beat (increasing blood supply to the muscles for physical activity); constriction of the sphincters of hollow viscera such as stomach and bladder; and relaxation of the muscles inside the visceral wall, such as bronchi (for more oxygen) and stomach (to reduce digestive activity). All these sympathetic functions are activated when survival appears to be threatened. This process is energy consuming and physiologically stressful, which explains why people are usually exhausted after such emergency or survival reactions.
The central autonomic neurons are located in the spinal cord. These neurons send nerve fibers (preganglionic fibers) to the autonomic ganglia outside the spinal cord. The preganglionic fibers communicate (via synapses) with ganglionic neurons. The ganglionic neurons send their nerve fibers (the postganglionic fibers) to blood vessels, glands, and organs.
ANATOMY OF THE SHOULDER
Anatomically, the shoulder is the junction of the arm and the trunk. Two bones, the clavicle (the collar bone) and the scapula (the shoulder blade), form the structure of the pectoral girdle and connect the humerus and the whole upper limb to the axial skeleton (the bones of the trunk and head) (see Figure 10-1). A number of joints are formed between the girdle bones and the axial skeleton.
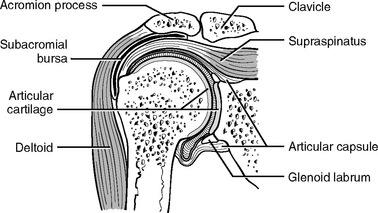
Glenohumeral Joint
Motion of the arm requires action at all joints of the shoulder complex. The glenohumeral joint has more freedom of motion than any other joint in the body. Therefore this joint is the most important member of the shoulder complex, as well as the most frequent site of pain and impairment. This synovial joint has an incongruous ball-and-socket articulation. The articulation is made up of the large head of the humerus and the small and shallow glenoid fossa. Rather than merely rotating about a fixed axis, the head of the humerus also slides against the glenoid articulation surface (Figure 10-4). This intrinsic weakness of the joint makes it susceptible to degenerative changes and derangement and also renders the stability of the joint dependent on the supporting soft tissues.
The concave pear-shaped glenoid fossa is located at the lateral tip of the scapula (see Figure 10-4), which allows little close contact of the two articular surfaces. The shallow glenoid fossa is deepened by a lip, the glenoid labrum, surrounding the fossa. The glenohumeral capsule is attached to the lip. The glenohumeral articulation is a multiaxial ball-and-socket joint that allows movement in three axes.
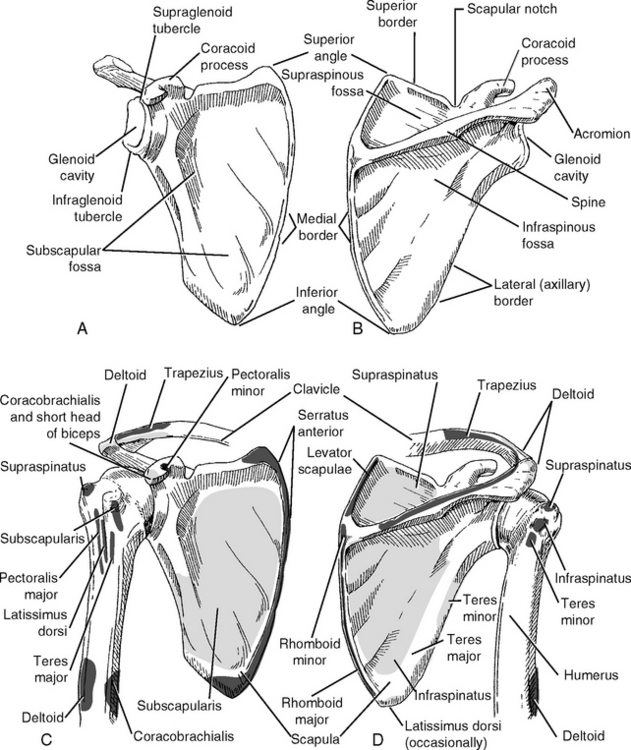
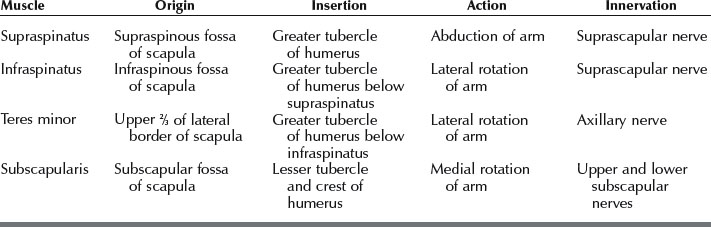
Four scapular muscles—supraspinatus, infraspinatus, teres minor, and subscapularis—form a musculotendinous rotator cuff to protect the glenohumeral joint and provide for its stability (Tables 10-5 and 10-6). All these rotator cuff muscles, except the supraspinatus, rotate the head of the humerus within the glenoid fossa. The tendons of these four muscles join the articular capsule of the glenohumeral joint and form a mass of tendons fused with the lateral part of the capsule. All the rotator cuff and deltoid muscles and their attachments to the head of the humerus should be carefully palpated and needled for any kind of shoulder disorder.
| Flexion | Deltoid (anterior fibers), pectoralis major (clavicular fibers) |
| Extension | Deltoid (posterior fibers), latissimus dorsi |
| Adduction | Pectoralis major, latissimus dorsi, teres major, subscapularis |
| Abduction | Deltoid, supraspinatus |
| Internal rotation | Pectoralis major, latissimus dorsi, teres major, subscapularis |
| External rotation | Deltoid (posterior fibers), infraspinatus, teres minor |
A bursa is a flattened sac filled with a lubricant called synovial fluid that enables the two flattened walls of the sac to slide freely over each other. The bursa eliminates the friction that would arise wherever a muscle or tendon could rub against another muscle, tendon, or bone. There are several bursae specifically associated with the glenohumeral joint (Figure 10-5). The important ones are the subacromial and subdeltoid bursae. These bursae separate the supraspinatus tendon and the head of the humerus from the acromion and the deltoid muscle. Frequently bursitis, the inflammation of the bursae, may occur with shoulder pain. Acupuncture needling is very effective in reducing bursitis. However, needling efficacy is slower if the walls of the bursa adhere to each other (adhesive bursitis). If a patient is diagnosed with adhesive bursitis, acupuncture needling is still recommended as a noninvasive therapy while the patient is seeking other medical modalities to alleviate the condition.
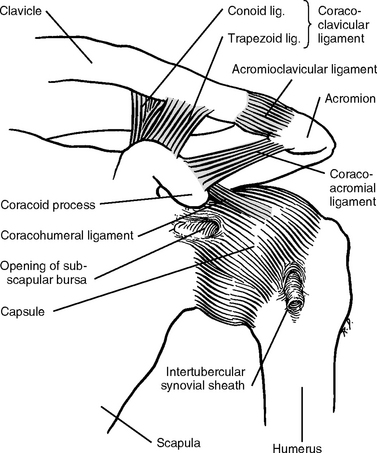
Acromioclavicular Joint
The acromioclavicular (AC) joint is a plane (flat) synarthrodial joint. It consists of the small convex facet on the lateral end of the clavicle and a small concave facet on the acromion of the scapula. This configuration allows rotation. The two bones are joined by fibrous tissue that gradually degenerates and forms a meniscus between them. The AC joint itself is not strong enough to hold the two bones together and is reinforced by the coracoclavicular ligament. This ligament consists of two smaller ligaments: the quadrangular trapezoid ligament and the cone-shaped conoid ligament. These two ligaments prevent separation of the clavicle and scapula. The primary function of the AC joint is to maintain coordination between the clavicle and the scapula during movements of the shoulder (Figure 10-6).
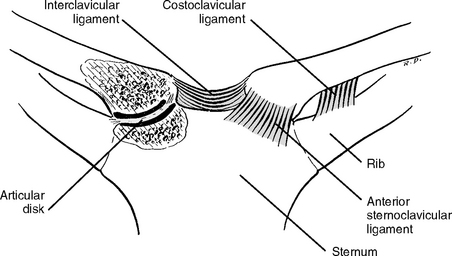
Sternoclavicular Joint
This joint is the only bony articulation between the upper limb and the axial skeleton. The sternoclavicular (SC) joint is formed by the articulation of the sternal end of the clavicle with the flat fossa of the clavicular notch on the superior lateral margin of the sternum and the cartilage of the first rib. A small articular disk is present between these bones with strong ligamentous support (Figure 10-7). The comparatively large sternal end of the clavicle rotates and forms the lateral boundary of the jugular notch. The SC joint allows the clavicle and shoulder to move up and down, forward and backward, or any combination of these movements.
The fibrous capsule of the SC joint is a key structure in supporting the weight of the entire upper limb. The SC joint is well supported and protected by anterior and posterior SC ligaments. The two clavicles are also joined to each other by an interclavicular ligament. Together these ligaments prevent the lateral and upward dislocation of the clavicle. The joint is further strengthened by the costoclavicular ligament that connects the first rib and the inferior surface of the clavicle.
Scapulothoracic Joint
Many patients complain of pain in the area between the upper spine and the medial border of the scapula. Our clinical experience indicates that about 70% of the patients have pain or tenderness in the levator scapulae, rhomboideus minor and major muscles, especially the parts of these muscles that are close to the medial border of the scapula. When administering acupuncture treatment, we use the following methods to avoid puncturing the lung: (1) use 1.5 cm long needles, (2) grasp and lift up the muscle for deeper needling, or (3) put the patient’s forearm on the back to raise the medial border of the scapula and then tilt and insert 4 cm needles to the attachment area of these muscles (see Figure 10-30).
Bicipital-humeral Joint
The biceps brachii muscle, as its name implies, has two heads, the long and the short (Figure 10-8). Here we focus on the tendon of the long head because it is frequently a source of shoulder pain. The long head has a long tendon that traverses the intertubercular groove on the humerus bone, passes through the glenohumeral jont, and finally attaches to the top of the glenohumeral joint (the supraglenoid tubercle).
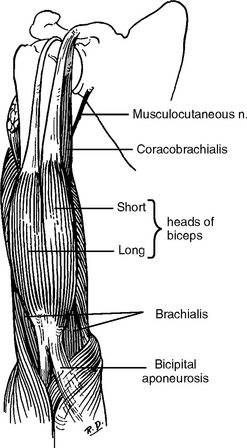
Figure 10-8 The biceps brachii muscle.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 121.)
Patients with shoulder pain always complain of tenderness or pain at this bicipital-humeral “joint” upon palpation. Thus, this area contains symptomatic acupoints for treating shoulder pain by acupuncture needling.
MOVEMENTS OF THE SHOULDER
Understanding the movement mechanism of the shoulder joint is necessary for knowing how and where to find symptomatic acupoints to treat shoulder pain. The movements of the shoulder are actually movements between the humerus and the scapula. Muscles, nerves, tendons, bursae, capsules, and articular surfaces of the joints are the elements involved in these highly coordinated movements (Table 10-7), and a disturbance in any of these elements may interrupt their coordination and result in shoulder pain. Knowing how patients move their shoulders greatly helps the practitioner to provide successful treatment.
Here we briefly discuss the major movements of the shoulder and the muscles involved. Shoulder movement involves two components of the glenohumeral joint, the scapula and the humerus. Scapular movements consist of elevation, depression, upward rotation, downward rotation, protraction, and retraction (Table 10-8). Humeral movements include flexion, extension, abduction, adduction, and internal (medial) and external (lateral) rotation. Any one muscle may perform more than one movement in coordination with other muscles.
| Elevation | Trapezius (upper fibers), rhomboids, levator scapulae |
| Depression | Latissimus dorsi, pectoralis major (costal fibers), trapezius (lower fibers) |
| Upward rotation | Trapezius, serratus anterior |
| Downward rotation | Rhomboids |
| Protraction | Serratus anterior, pectoralis major and minor |
| Retraction | Trapezius, rhomboids |
| Internal rotation | Subscapularis, pectoralis major, latissimus dorsi, teres major deltoid (clavicular fibers) |
| External rotation | Infraspinatus, teres minor, deltoid (posterior fibers) |
Scapular Movements
Elevation of the scapula is produced by four muscles (Figure 10-9). The medial border of the scapula is elevated by three muscles, the levator scapulae and the rhomboideus minor and major. The lateral angle of the scapula is changed by the upper fibers of the trapezius connected to the clavicle, acromion, and spine of the scapula. Often we examine patients with one shoulder higher than the other because of the tightness of these four muscles. The shoulder level returns to normal after proper needling of these muscles.
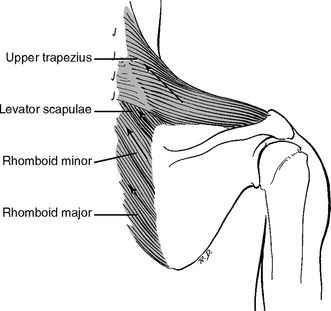
Figure 10-9 Elevators of the scapula.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 98.)
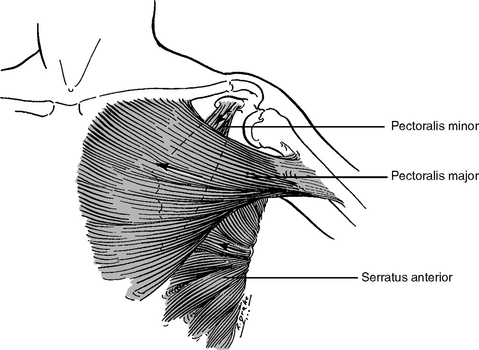
Muscles involved in depression of the scapula include the pectoralis minor and major, subclavius, latissimus dorsi, lower fibers of the trapezius, and serratus anterior (Figure 10-10). In some patients with upper or lower back pain, one shoulder is lower than the other and needling both the lower back muscles and the depressor muscles returns the shoulder to normal level.
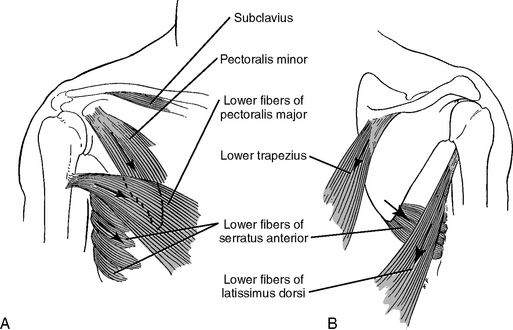
Figure 10-10 Depressors of the scapula. A, Anterior view. B, Posterior view.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 99.)
When abduction occurs, such as when raising an arm, the scapula rotates upward. Upward rotation is brought about by the combined action of the trapezius and the serratus anterior (Figure 10-11). When reaching down to pick up something from the floor, the scapula rotates downward. Downward rotation is carried out by the combined action of raising the medial border and lowering the lateral angle of the scapula. The levator scapulae and both rhomboids are responsible for raising the medial border, while the pectoralis major and minor and latissimus dorsi, aided by gravity on the free limb, are responsible for lowering the lateral angle of the scapula (Figure 10-12).
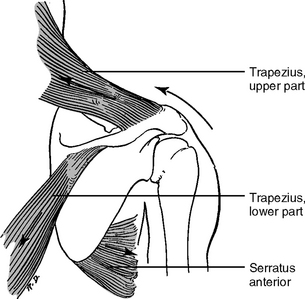
Figure 10-11 Upward rotators of the scapula.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 99.)
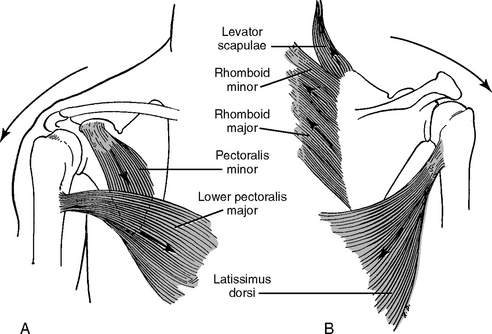
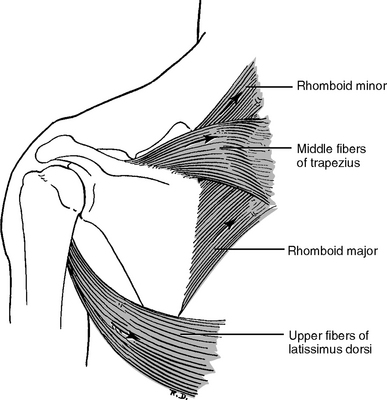
Figure 10-12 Downward rotation of the scapula. A, Anterior view. B, Posterior view.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 100.)
The pectoralis major, minor, and serratus anterior bring about protraction (Figure 10-13), while the middle fibers of the trapezius carry out retraction (Figure 10-14).
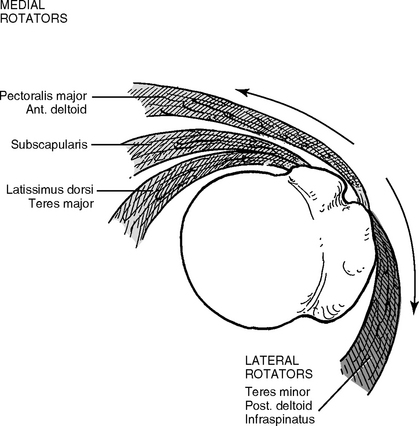
Humeral Movements
Internal (medial) rotation is brought about primarily by subscapularis. Other internal rotators include pectoralis major, latissimus dorsi, teres major, and clavicular fibers of the deltoid. External (lateral) rotation is performed by infraspinatus and teres minor, and also by the posterior fibers of the deltoid if extension and lateral rotation are combined. Figure 10-15 explains the topographic relationship between the internal and external rotators of the humerus.
SHOULDER PAINS AND THEIR LOCATIONS
Bicipital Groove
The bicipital groove can be involved in bicipital tendinitis and biceps tendon subluxation and tear.
Sternoclavicular Joint
Pain in this joint can be caused by trauma, infection, or degenerative changes.
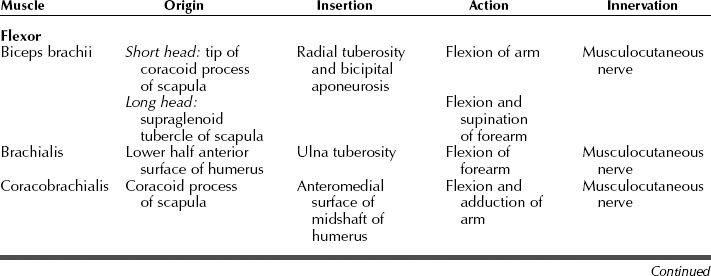
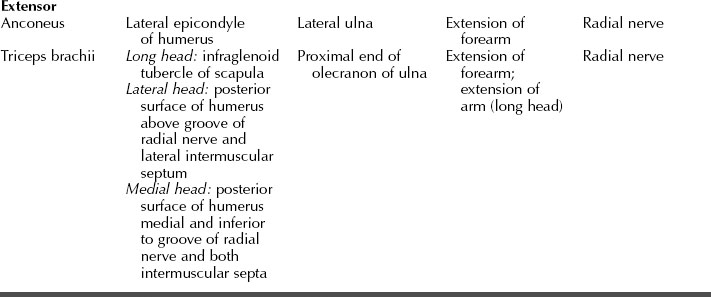
THE MUSCLES AND NERVES OF THE ARM
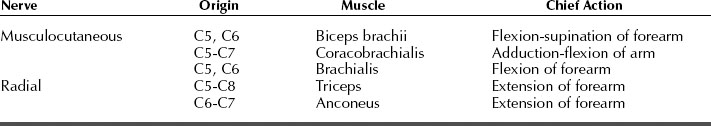
Muscles
The arm muscles consist of two groups: flexor and extensor (Table 10-9). The flexor muscles are coracobrachialis, biceps brachii, and brachialis. As discussed above, the biceps brachii has two heads, the long head being a common source of pain because of its long tendon, which spans the glenohumeral joint and is attached to the supraglenoid tubercle. Pain from the long head of the biceps brachii is palpable right on the region of the intertubercular groove on the head of the humerus.
THE ELBOW JOINTS: HUMERORADIAL, HUMEROULNAR, AND RADIOULNAR
The elbow is a joint complex that mechanically links the arm (the humerus) and the forearm (two bones: the radius and ulna) (see Figure 10-1). The articulating structures of the three bones provide great stability to the joint. The distal end of the humerus has two articular surfaces, the pulley-shaped trochlea and the spherical capitulum (Figure 10-16). The articular surfaces of each forearm bone, radius and ulna, correspond in shape to these two articular surfaces of the humerus. Medially, the trochlear notch of the ulna articulates with the trochlea, so the ulna bone, and in fact the whole forearm, rotates around the trochlea to perform two-dimensional flexion-extension movement. Laterally the articular surface of the head of the radius is shaped like a cup with a flat concavity that fits into the capitulum. This joint enables the radius bone to rotate along its own axis. The two joints are correspondingly named humeroulnar and humeroradial joints. The third joint, the proximal radioulnar joint, is formed at the proximal region between the head of the radius and ulna, thus allowing rotation of the head of the radius to produce movements of supination (turning the palms up) and pronation (turning the palms down).
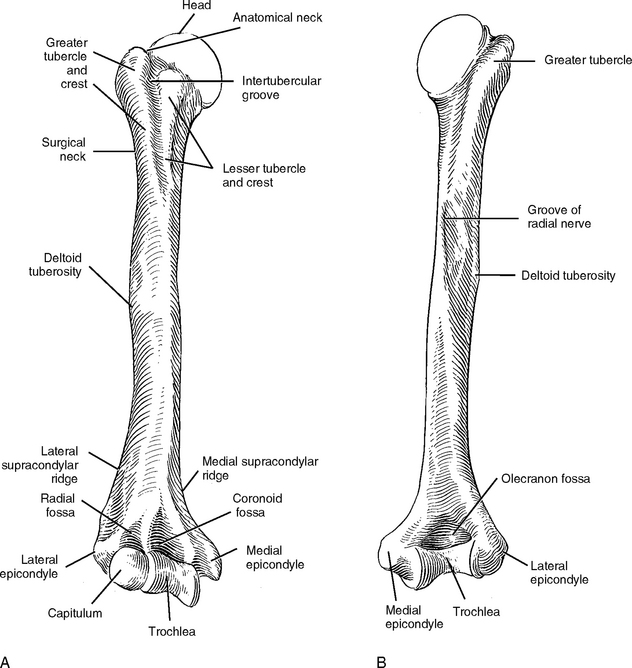
Figure 10-16 Anterior (A) and posterior (B) views of the humerus.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 115.)
The articular capsule of the joint is relatively thin, but strong collateral ligaments are located on the medial (ulnar) and lateral (radial) sides of the joint and the correspondingly named medial (ulnar) and lateral (radial) collateral ligaments. A ring-like ligament called the annular ligament covers the radioulnar joint (Figure 10-17).
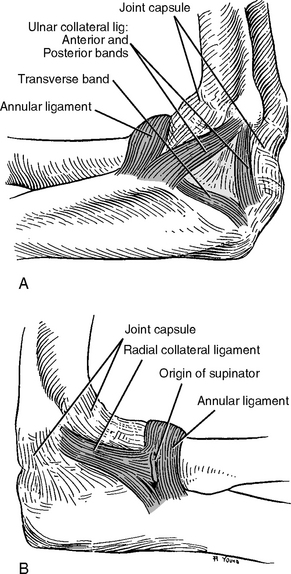
Figure 10-17 Medial (A) and lateral (B) views of the ligaments of the elbow joint.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 118.)
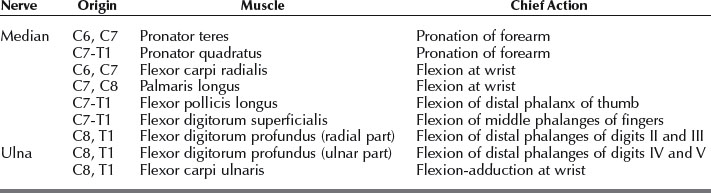
The elbow joint is supplied by four nerves: the musculocutaneous, median, ulnar, and radial.
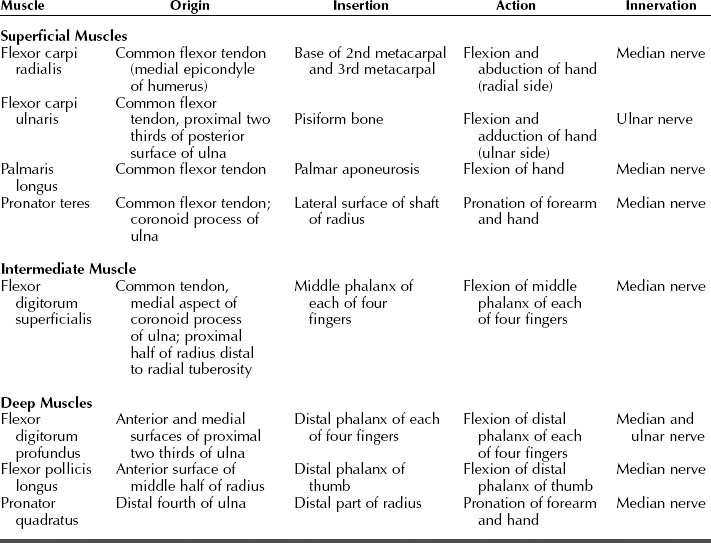
THE FOREARM
The forearm contains 19 muscles, divided into two groups: the 8 flexors (Table 10-11) and the 11 extensors. These muscles act across several joints: the elbow, the wrist, and the small joints of the hand.
Flexors and their Innervation
The eight flexor muscles are arranged into three layers (Figures 10-18 through 10-20). These muscles (Table 10-12) perform the following functions:
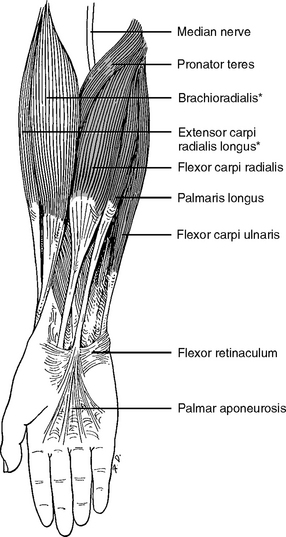
Figure 10-18 The superficial flexor muscles of the right forearm. The starred muscles are extensors.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 144.)
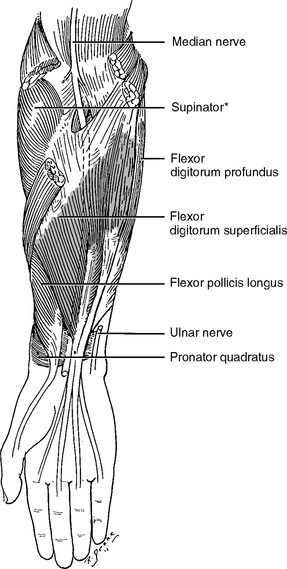
Figure 10-19 The intermediate muscle layer of the right forearm. Supinator is an extensor muscle.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 145.)
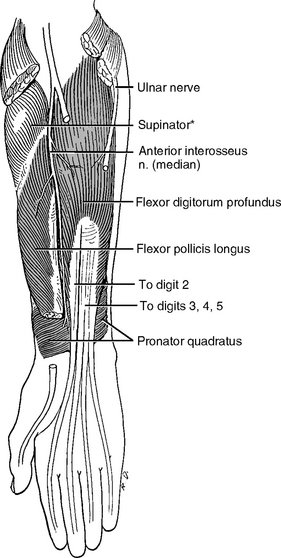
Figure 10-20 The deepest flexor muscles of the right forearm. The supinator (starred) is an extensor muscle of the forearm.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 145.)
The deep layer contains three muscles: flexor digitorum profundus, flexor pollicis longus, and pronator quadratus. The flexor digitorum profundus has an extensive origin from the proximal ulna and the membrane between the ulna and the radius (interosseous membrane). This muscle ends in four tendons that pass the flexor retinaculum and is inserted on the base of the distal phalanges of each of the four fingers.
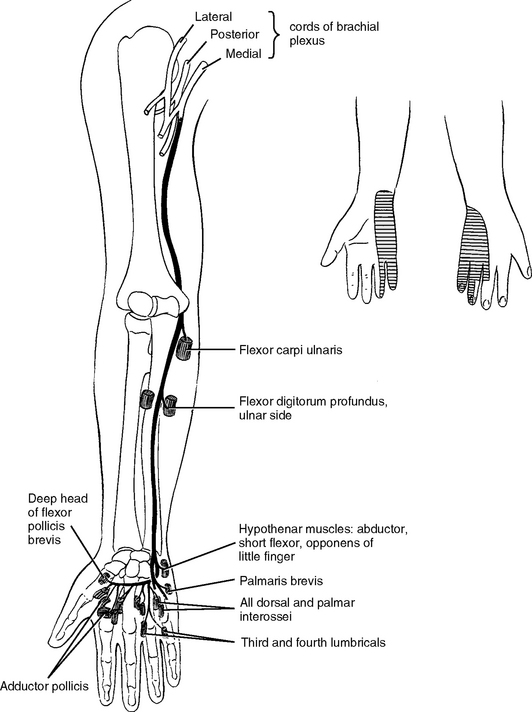
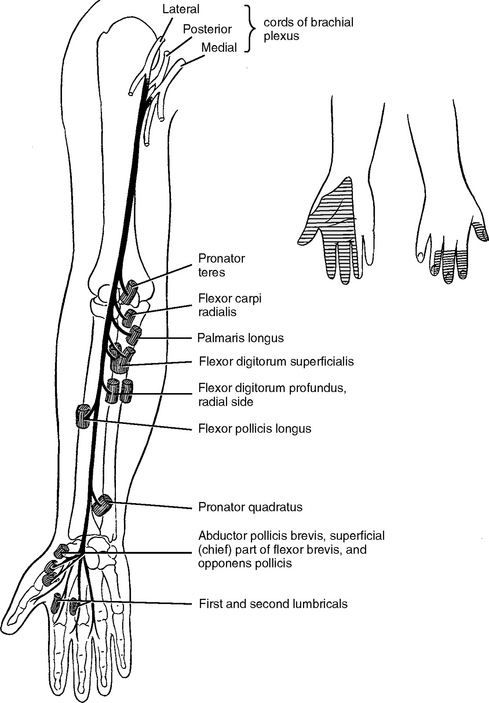
The ulnar nerve runs posterior to the medial epicondyle and enters the forearm (Figure 10-21). In the forearm, it runs along the bone of the ulna, emerges from the lateral side of flexor carpi ulnaris, and continues to the hand. The median nerve runs practically straight down the middle of the forearm (Figure 10-22).
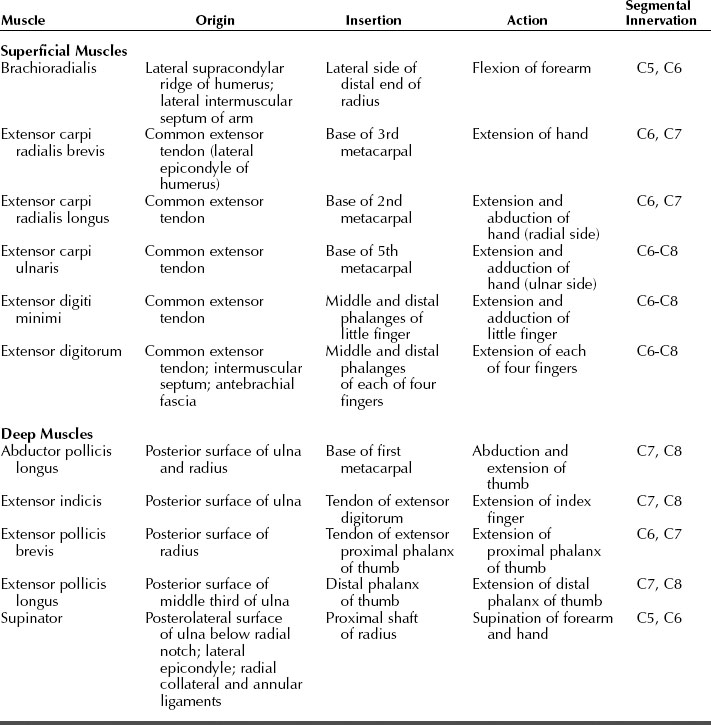
Extensors and their Innervation
The 11 extensor muscles of the forearm (Table 10-13) are arranged into superficial (Figure 10-23) and deep layers (Figure 10-24). The radial nerve innervates all 11 extensor muscles (Figure 10-25) and they perform the following functions:
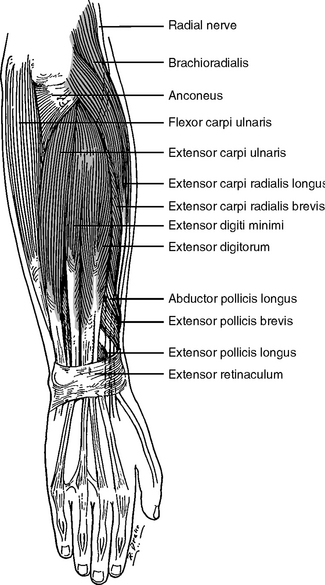
Figure 10-23 The superficial extensor muscles of the right forearm.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 161.)
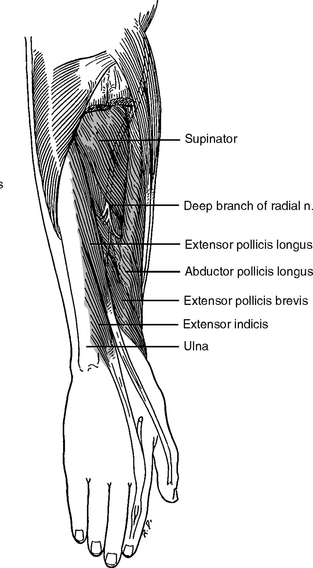
Figure 10-24 The deeper extensor muscles of the right forearm.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 161.)
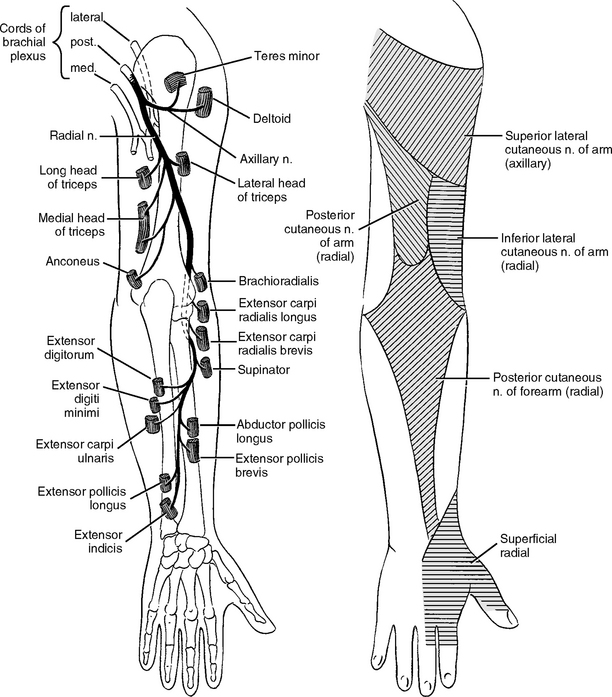
Figure 10-25 The innervation of the radial nerve.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 168.)
The superficial muscle group arises from the supracondylar ridge and the lateral epicondyle (common extensor tendon) of the humerus. Four muscles attach to this common extensor tendon: extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris. Repetitive wrist and finger extension such as in some sports and occupations may injure these muscles and cause inflammation of the common extensor tendon (e.g., lateral epicondylitis or tennis elbow).
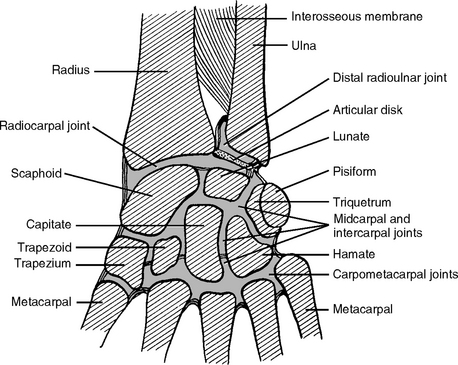
THE WRIST COMPLEX
Anatomically the wrist is not a single joint, for this region is the junction of the two forerarm bones (radius and ulna) and the eight wrist bones (carpal bones). Thus different joints are formed between the radius and ulna, among the eight carpal bones, and between the forearm bones and carpal bones. The wrist complex consists of the following joints (Figure 10-26): the distal radioulnar joint, the radiocarpal joint (“the wrist joint”), the intercarpal joints, and the midcarpal joint.
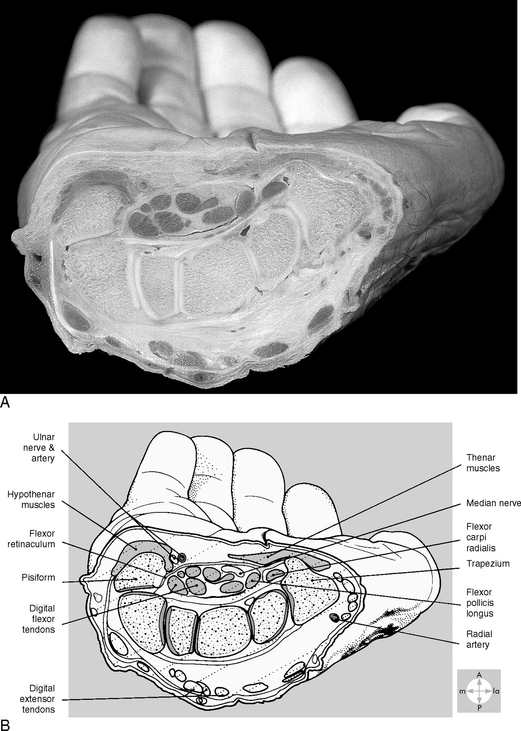
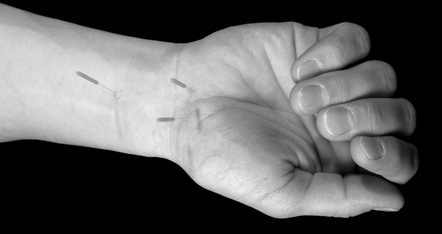
The tendons of the long flexor and extensor muscles, together with the nerves and blood vessels, are grouped around the distal ends of the radius and the ulna, the radiocarpal joint, and the carpal bones. To maintain the functional structure, the wrist complex is reinforced by tendons and specialized soft tissues. The forearm fascia (antebrachial fascia) is thickened on the dorsal wrist to form a transverse band called extensor retinaculum, which retains extensor tendons in their position. On the palmar side of the wrist, the deep fascia is also thickened anteriorly to form the flexor retinaculum, which covers the anterior concavity formed by the carpal bones. Thus, the flexor retinaculum converts the anterior carpal concavity into a so-called carpal tunnel through which the flexor tendons pass (see below: carpal tunnel syndrome). There are two creases at the wrist. The distal wrist crease indicates the proximal border of the flexor retinaculum. Synovial sheaths surround the long flexor tendons and they glide within the fibrous sheath to reduce the friction between the tissues during movement.
Anatomic relations around the wrist have clinical significance because direct and indirect trauma commonly damages structures around the wrist. Painful irritation of the synovial sheath is common at the point where the tendons of the extensor pollicis brevis and abductor pollicis longus cross over the tendons of the extensors carpi radialis longus and brevis. Inflammation caused by irritation or infection (tenosynovitis) will distend the flexor tendon sheaths. If the pressure of the carpal tunnel is not relieved, the tendons will die due to ischemia. Because of the slow turnover of collagen, tendon rupture may not occur for several weeks, but the median nerve will suffer damage in the carpal tunnel in a very short time.
THE HAND
The remarkable functions of the human hand are achieved by a combination of comprehensive mechanical movement and finely controlled accuracy and tactile sensitivity, which account for a greater area in the neocortex of the human brain than the functions of any other organ.
The base skeleton of the hand is composed of eight carpal bones arranged in two rows, proximal and distal (see the section on the wrist complex). The proximal row of the four carpal bones articulates with the radial to form the radiocarpal joint, the wrist joint. The distal row of carpal bones articulates with the elongated metacarpal bones (see Figure 10-26). Distal to the metacarpal bones are the 14 phalanges: two for the thumb and three for all the other four digits. Different joints are formed between the bones: intercarpal, carpometacarpal, metacarpophalangeal, and interphalangeal. An important acupoint H12 superficial radial is formed between metacarpals I and II.
The skin of the dorsum is loose and freely mobile with little soft tissue so the dorsal skin and fascia can slide freely over extensor tendons and bones. In contrast, the fibrous bands anchor and stabilize the skin of the palm with the underlying palmar aponeurosis. The soft tissues of the palm are arranged into four layers: just below the palmar aponeurosis is the thenar or lateral compartment containing short muscles of the thumb (thenar), the little finger (hypothenar), nerves, and vessels. The next layer is a central compartment containing vessels, nerves, and the long flexors of the fingers (flexor digitorum superficialis and profundus). The deeper layer contains the adductor muscle of the thumb, nerves, and vessels. The fourth layer includes the four dorsal interosseous muscles lying between the five metacarpal bones.
The tendons of the flexor digitorum superficialis and profundus reach the proximal phalanges and are invested with a synovial sheath. Each tendon of the flexor digitorum superficialis splits into two parts that lie on each side of the tendon of flexor digitorum profundus (Figure 10-27) and finally are inserted into the corresponding phalanx.
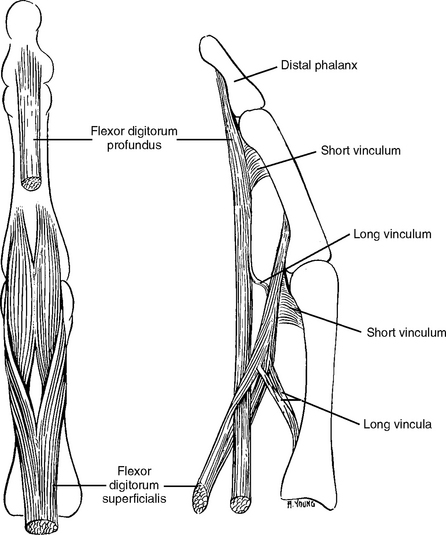
Figure 10-27 The flexor tendons of a finger, anterior and lateral views.
(From Jenkins D: Hollinshead’s functional anatomy of the limbs and back, ed 8, Philadelphia, 2002, WB Saunders, p 188.)
In addition to the basic anatomic knowledge of the upper limb from the shoulder to the hand, which is essential for acupuncture treatment, it is also important to know the sensory nerve distribution in the upper limb particularly when treating upper limb pain and numbness. A brief summary of the sensory nerve distribution on the upper limb is shown in Figure 10-28. Please note that in each patient there is a considerable overlap between the sensory territories of different nerves.
UPPER LIMB PAIN COMMONLY ENCOUNTERED IN ACUPUNCTURE CLINICS
Soft Tissue Pain and Injuries due to Overuse (Repetitive Motion Disorders)
The pathological conditions of irritated tendons may be different. The underlying pathologic entities can be tendinitis (inflammation of the tendon), peritendinitis (inflammation of the tendon and its sheath), or tendinosis (degeneration of the tendon). Our clinical experience shows that most of these tendon problems respond well to acupuncture needling if treated together with their corresponding muscles. Tight muscles always transfer the pulling force to the tendons and cause inflammation of the tendons. The stress on the tendons can only be relieved if the muscles are relaxed and flexible.
Rotator Cuff Tendinopathy
Four scapular muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) fuse their tendons with the fibrous capsule of the glenohumeral joint to form a musculotendinous cuff. The rotator cuff protects and stabilizes the shoulder joint by holding the head of the humerus in the glenoid cavity of the scapula (see the section on the glenohumeral joint). The supraspinatus helps abduct the arm and the other three rotator cuff muscles rotate the humerus.
Degenerative tendinosis of the musculotendinous rotator cuff is a common disease in senior people. Calcium deposits can be formed in the tendon of the supraspinatus and other rotator cuff muscles.
Subacromial Bursitis (Calcific Bursitis, Scapulohumeral Bursitis)
A bursa is a small fluid-filled sac or saclike cavity situated where friction would otherwise occur. Subacromial bursae lie between the acromion and supraspinatus tendon and extend between the deltoid and greater tubercle. Inflammation of the subacromial bursa can be the underlying cause of acute or chronic shoulder pain (see Figure 10-5). Patients with subacromial bursitis complain of pain and tenderness in the lateral shoulder, with pain that worsens during movement. In chronic cases, the bursa may become thickened and fibrotic, although this pathologic change may not be radiographically detectable. A calcium deposit can develop in the subdeltoid or subacromial bursa.
Bicipital Tendinitis
The tendon of the long head of the biceps ascends in the intertubercular (bicipital) groove of the humerus and enters the glenohumeral capsule. Within the capsule the tendon crosses the head of the humerus and attaches to the supraglenoid tubercle of the scapula (see Figure 10-8). The long course and angulation of this tendon make it susceptible to tears and degenerative changes. Pain or tenderness is anterior to the shoulder and radiates down the anterior arm.
Epicondylitis
Epicondylitis, if related to repetitive overuse of the arm, usually results from stressful, tight, or damaged muscles. Needling these muscles is even more important than needling the common tendon. Acupuncture usually provides very good results in most patients with epicondylitis, especially in those with acute onset from sport activities. Self-healable sports injuries such as those caused by repetitive overuse are usually soft tissue injuries with inflammation and swelling. Athletes usually maintain good self-healing potential, so acupuncture needling can achieve satisfactory results. If epicondylitis is caused by age-related necrotic change, less efficacy can be expected and more treatments are needed to reduce the inflammation and pain.
Localized Median Nerve Lesion: Carpal Tunnel Syndrome
The carpal tunnel is a narrow fibro-osseous passage through which 10 structures pass: the median nerve, the flexor pollicis longus tendon, four tendons of the flexor digitorum superficialis, and four tendons of the flexor digitorum profundus (Figure 10-29). All eight flexor tendons in the carpal tunnel share the same common synovial sheath (also called the ulnar bursa) formed by the synovial membrane. Sufficient synovial fluid is contained in the bursa to lubricate and hence facilitate the movement of the tendons beneath the retinaculum.
The efficacy of acupuncture in treating CTS depends on the severity of the condition, the nature of the case, and the general health of the patient. For example, better and faster results are achieved in patients who are suffering from the initial stages of CTS in one hand than in those who are affected in both hands. Acute and recently developed CTS is more responsive to acupuncture needling than chronic CTS in one or both hands. If the CTS is caused by carpal bone dislocation or rheumatoid thickening of the sheath as opposed to inflammation or infection, acupuncture efficacy will be uncertain. Acupuncture may help in reducing some pain, but the major symptoms can be reduced only after the carpal bone dislocation is corrected or the pressure from the rheumatoid thickening of the sheath can be released.
Joint and Bone Pain
Chronic Joint and Bone Pain
With age, cartilage changes and may lose its elasticity, making the joint more vulnerable to damage from injury or overuse. The breakdown of cartilage causes the synovial membrane of the joint to become inflamed. The inflamed tissue releases enzymes that further destroy cartilage. As a result, the bones become exposed from cartilage loss, thicken, and form bone spurs (osteophytes). Bone rubs against bone and produces pain. People with joint injuries due to automobile accidents, sports, and work-related activity have an increased risk of developing OA.
TREATMENT PROTOCOL
Symptomatic Acupoints
Figures 10-30 through 10-33 show some of the typical symptomatic acupoints used for upper limb pain and disorders. Careful palpation should be applied to find these local symptomatic acupoints. Figures 10-30 through 10-33 also show some of the needling methods. With a good understanding of anatomical structure and mechanical function, practitioners can explore more effective needling methods for each particular case.