Procedure 10 Extensor Tendon Repair in Zones 1 to 5
![]() See Video 7: Turnover Tendon Flap for PIP Extensor Tendon Injury
See Video 7: Turnover Tendon Flap for PIP Extensor Tendon Injury
Surgical Anatomy
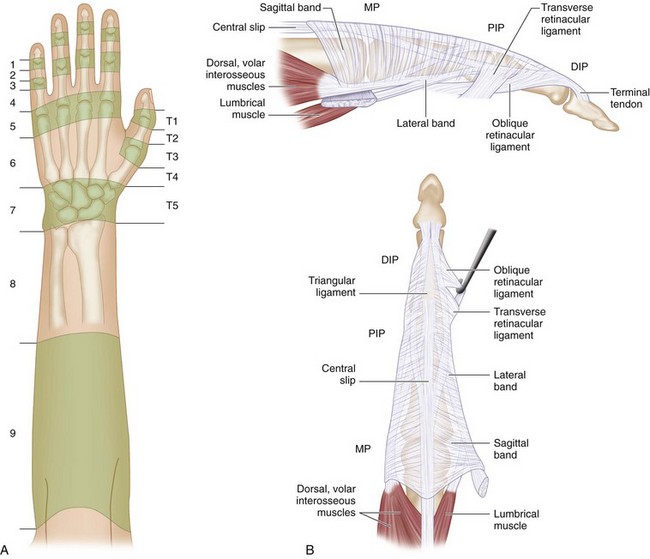
 Extensor tendon injuries are divided into nine zones for the fingers and seven zones for the thumb numbered from distal to proximal (Fig. 10-2A). An easy way to remember these zones is to bear in mind that the odd-numbered zones are located over the joints. Therefore zones 1, 3, 5, and 7 are located over the distal interphalangeal (DIP) joint, proximal interphalangeal (PIP) joint, metacarpophalangeal (MCP) joint, and wrist, respectively.
Extensor tendon injuries are divided into nine zones for the fingers and seven zones for the thumb numbered from distal to proximal (Fig. 10-2A). An easy way to remember these zones is to bear in mind that the odd-numbered zones are located over the joints. Therefore zones 1, 3, 5, and 7 are located over the distal interphalangeal (DIP) joint, proximal interphalangeal (PIP) joint, metacarpophalangeal (MCP) joint, and wrist, respectively.
 The extensor tendon is thick over the MCP joint but becomes broad and thin over the dorsum of the proximal phalanx, where it divides into three portions. The central portion becomes the central slip that inserts into the base of the middle phalanx, and the lateral portions join the lateral bands. The tendons of the lumbrical and interosseous muscles form the lateral bands. These lateral bands come together over the middle phalanx and form the most distal part of the extensor tendon that inserts into the base of the distal phalanx (Fig. 10-2B).
The extensor tendon is thick over the MCP joint but becomes broad and thin over the dorsum of the proximal phalanx, where it divides into three portions. The central portion becomes the central slip that inserts into the base of the middle phalanx, and the lateral portions join the lateral bands. The tendons of the lumbrical and interosseous muscles form the lateral bands. These lateral bands come together over the middle phalanx and form the most distal part of the extensor tendon that inserts into the base of the distal phalanx (Fig. 10-2B).
 At the MCP joint, the extensor tendon is held in position by the sagittal bands, which arise from the volar plate of the MCP joint and the intermetacarpal ligaments, to insert on the extensor hood. Injury to the sagittal bands may result in subluxation of the extensor tendon.
At the MCP joint, the extensor tendon is held in position by the sagittal bands, which arise from the volar plate of the MCP joint and the intermetacarpal ligaments, to insert on the extensor hood. Injury to the sagittal bands may result in subluxation of the extensor tendon.
 There is very little excursion of the extensor tendon over the fingers (11 to 17 mm at the MCP joint, 6 to 8 mm at the PIP joint, and 4 to 5 mm at the DIP joint). It is therefore important to do an accurate repair and avoid bunching up the tendon. It is usually possible to pass a core suture through the extensor tendon in the proximal half of zone 4 and in zone 5. However, only a simple suture is possible in zones 1, 2, and 3.
There is very little excursion of the extensor tendon over the fingers (11 to 17 mm at the MCP joint, 6 to 8 mm at the PIP joint, and 4 to 5 mm at the DIP joint). It is therefore important to do an accurate repair and avoid bunching up the tendon. It is usually possible to pass a core suture through the extensor tendon in the proximal half of zone 4 and in zone 5. However, only a simple suture is possible in zones 1, 2, and 3.
 Lacerations to the extensor pollicis longus (EPL) tendon cannot be tested by simply examining extension of the thumb interphalangeal (IP) joint. The IP joint may be extended by the extensor pollicis brevis (EPB) and the thenar intrinsic muscles via their insertions on the extensor expansion. The EPL is tested by placing the patient’s hand flat on a table and asking the patient to lift the thumb off the table (Fig. 10-3).
Lacerations to the extensor pollicis longus (EPL) tendon cannot be tested by simply examining extension of the thumb interphalangeal (IP) joint. The IP joint may be extended by the extensor pollicis brevis (EPB) and the thenar intrinsic muscles via their insertions on the extensor expansion. The EPL is tested by placing the patient’s hand flat on a table and asking the patient to lift the thumb off the table (Fig. 10-3).
Positioning
 Extensor tendon repairs can be done under a digital block (zones 1, 2, and 3) or a wrist block (zones 4 and 5). The use of a forearm tourniquet (placed distally over the nonmuscular portion of the forearm) will allow the patient to tolerate the tourniquet for a longer period (30 to 40 minutes) compared with the usual placement over the arm (20 to 30 minutes). The patient is positioned supine with the affected extremity on a hand table.
Extensor tendon repairs can be done under a digital block (zones 1, 2, and 3) or a wrist block (zones 4 and 5). The use of a forearm tourniquet (placed distally over the nonmuscular portion of the forearm) will allow the patient to tolerate the tourniquet for a longer period (30 to 40 minutes) compared with the usual placement over the arm (20 to 30 minutes). The patient is positioned supine with the affected extremity on a hand table.
Exposures
Zone 1 Injury
Clinical Examination
 Patients present with a flexed posture of the DIP joint (mallet finger) and inability to actively extend the DIP joint (Fig. 10-4).
Patients present with a flexed posture of the DIP joint (mallet finger) and inability to actively extend the DIP joint (Fig. 10-4).
 Patients with an untreated mallet finger, especially those with a preexisting hyperextensible PIP joint, can develop a compensatory swan-neck deformity because of extensor force being directed toward the central slip and leading to hyperextension at the PIP joint.
Patients with an untreated mallet finger, especially those with a preexisting hyperextensible PIP joint, can develop a compensatory swan-neck deformity because of extensor force being directed toward the central slip and leading to hyperextension at the PIP joint.
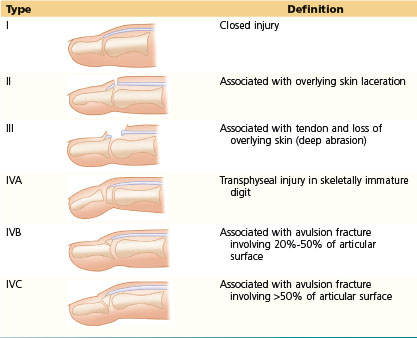
 Doyle has classified mallet finger into four types (Table 10-1).
Doyle has classified mallet finger into four types (Table 10-1).
Table 10-1 Classification of Mallet Finger
Procedure
Step 1
Step 2
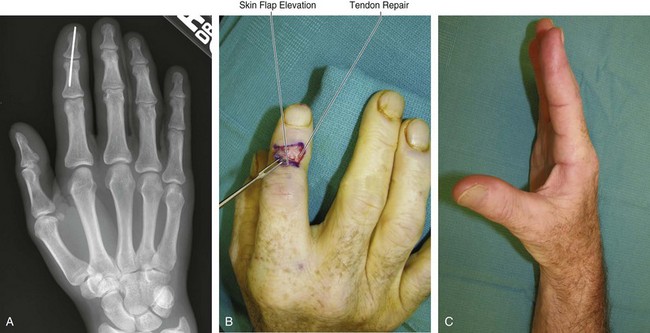
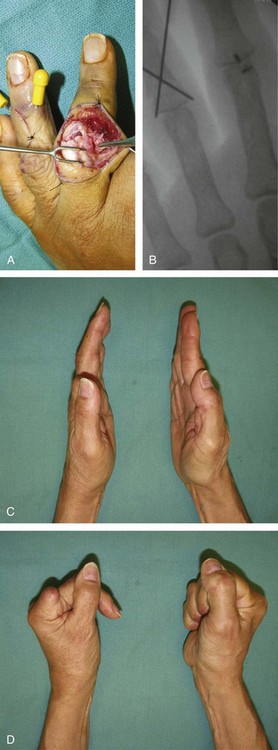
 The DIP joint is pinned in extension or slight hyperextension using a 0.045-inch K-wire (Fig. 10-5A).
The DIP joint is pinned in extension or slight hyperextension using a 0.045-inch K-wire (Fig. 10-5A).
Step 4
 The tourniquet is released and hemostasis secured. Skin is closed with 5-0 nylon interrupted sutures.
The tourniquet is released and hemostasis secured. Skin is closed with 5-0 nylon interrupted sutures.
 The K-wire may be cut short and buried under the skin.
The K-wire may be cut short and buried under the skin.
 A thermoplastic splint is also provided to immobilize the DIP joint and protect the tip of the K-wire. Additional immobilization of the PIP joint in extension may be required in patients who have an associated swan-neck deformity.
A thermoplastic splint is also provided to immobilize the DIP joint and protect the tip of the K-wire. Additional immobilization of the PIP joint in extension may be required in patients who have an associated swan-neck deformity.
Postoperative Care and Expected Outcomes
 The K-wire should be maintained for 6 weeks, after which time it is removed and the patient is started on gradual mobilization of the DIP joint. The splint is maintained for an additional 4 weeks.
The K-wire should be maintained for 6 weeks, after which time it is removed and the patient is started on gradual mobilization of the DIP joint. The splint is maintained for an additional 4 weeks.
 Patients should be advised to continue mobilizing the PIP joint during the period of DIP joint splintage.
Patients should be advised to continue mobilizing the PIP joint during the period of DIP joint splintage.
 Seventy percent to 80% of patients with zone 1 extensor tendon injuries have an excellent (no lag) to good (<10-degree lag) outcome (Fig. 10-5C).
Seventy percent to 80% of patients with zone 1 extensor tendon injuries have an excellent (no lag) to good (<10-degree lag) outcome (Fig. 10-5C).
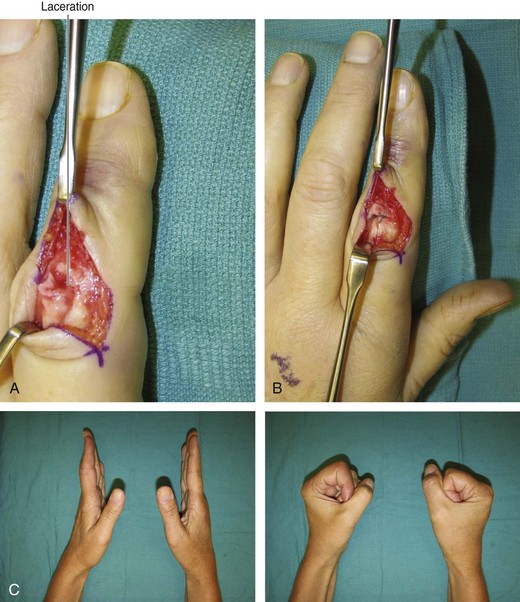
Zone 3 Injury
Clinical Examination
 Patients with an injury to the central slip (zone 3) but with intact lateral bands and triangular ligament will be able to extend the PIP joint through the lateral bands that are still dorsal to the axis of the PIP joint. However, if untreated, the triangular ligament is gradually attenuated over a period of 2 to 3 weeks, and the lateral bands sublux volar to the axis of the PIP joint. This results in the lateral bands becoming a flexor of the PIP joint. The patient will now be unable to extend the PIP joint and will present with a boutonnière deformity (flexion of the PIP joint and hyperextension of the DIP joint) (Fig. 10-7).
Patients with an injury to the central slip (zone 3) but with intact lateral bands and triangular ligament will be able to extend the PIP joint through the lateral bands that are still dorsal to the axis of the PIP joint. However, if untreated, the triangular ligament is gradually attenuated over a period of 2 to 3 weeks, and the lateral bands sublux volar to the axis of the PIP joint. This results in the lateral bands becoming a flexor of the PIP joint. The patient will now be unable to extend the PIP joint and will present with a boutonnière deformity (flexion of the PIP joint and hyperextension of the DIP joint) (Fig. 10-7).
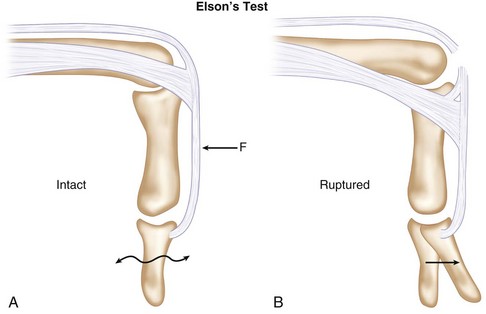
 The Elson test is useful in diagnosing a central slip injury early (before the development of a boutonnière deformity) and in differentiating a boutonnière deformity from edema of the PIP joint or a PIP joint flexion contracture. The examiner passively flexes the PIP joint to 90 degrees over a tabletop and asks the patient to attempt active extension of the PIP joint while the examiner resists PIP joint extension. Acute rupture of the central slip results in no extension power being felt at the PIP joint and significant extension power, or hyperextension, produced at the DIP joint (Fig. 10-8).
The Elson test is useful in diagnosing a central slip injury early (before the development of a boutonnière deformity) and in differentiating a boutonnière deformity from edema of the PIP joint or a PIP joint flexion contracture. The examiner passively flexes the PIP joint to 90 degrees over a tabletop and asks the patient to attempt active extension of the PIP joint while the examiner resists PIP joint extension. Acute rupture of the central slip results in no extension power being felt at the PIP joint and significant extension power, or hyperextension, produced at the DIP joint (Fig. 10-8).
Procedure
Step 3
Step 3 Pearls
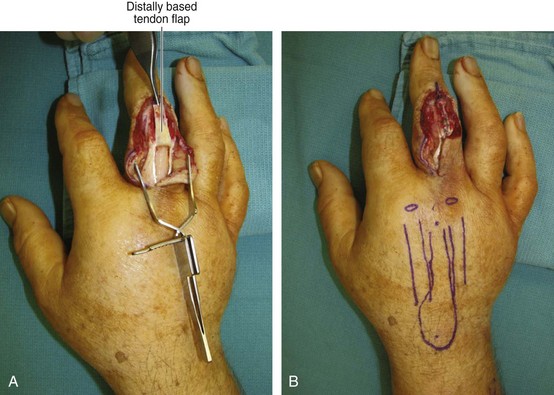
If there is a gap, a tendon turndown procedure may be used. Appropriate length of the tendon is raised as a distally based flap from the proximal tendon (Fig. 10-10). Another option would be to use a free tendon graft.
If there is not enough distal terminal tendon for suturing, a bone anchor can be used. The bone anchor must be inserted before the joint is pinned (Fig. 10-11).
Zone 4 Injury
Procedure
Step 2
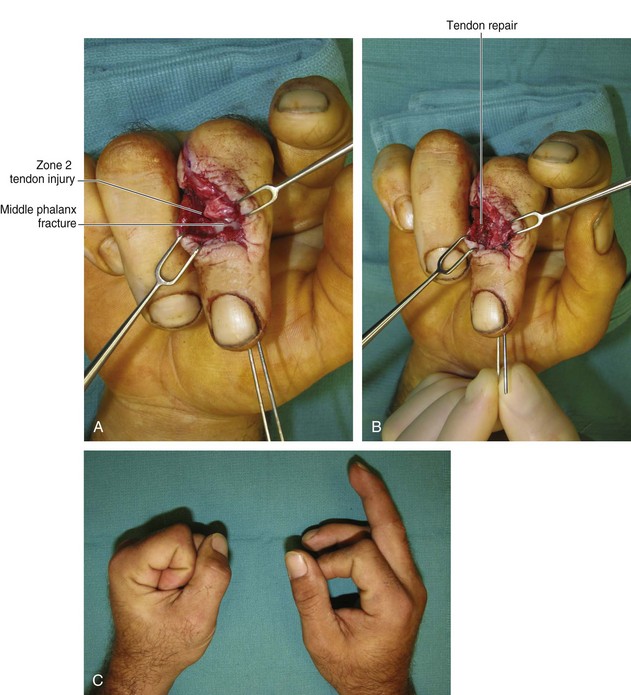
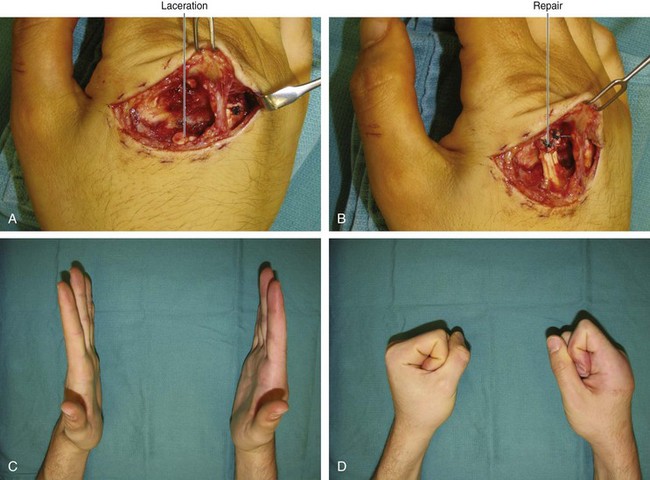
 If the tendon is thick (proximal half of zone 4), a modified Kessler repair with a 4-0 Ethibond core suture and a 6-0 Prolene epitendinous repair is carried out.
If the tendon is thick (proximal half of zone 4), a modified Kessler repair with a 4-0 Ethibond core suture and a 6-0 Prolene epitendinous repair is carried out.
 If the tendon is not thick (distal half of zone 4), a horizontal mattress repair with 4-0 Ethibond suture and a running 6-0 Prolene suture repair is carried out.
If the tendon is not thick (distal half of zone 4), a horizontal mattress repair with 4-0 Ethibond suture and a running 6-0 Prolene suture repair is carried out.
Zone 5 Injury
Clinical Examination
 A human bite injury should always be suspected in an open zone 5 tendon injury. These patients present with a small puncture wound over the knuckle that is associated with extensor tendon dysfunction, pain out of proportion to the presentation (owing to underlying joint infection), and a suspicious history.
A human bite injury should always be suspected in an open zone 5 tendon injury. These patients present with a small puncture wound over the knuckle that is associated with extensor tendon dysfunction, pain out of proportion to the presentation (owing to underlying joint infection), and a suspicious history.
 A closed rupture of the sagittal band should be suspected in patients who present with an inability to extend the finger after blunt trauma to the dorsum of the hand. This can be confirmed by passively placing the patient’s digit in extension and observing whether the patient can actively maintain the position. If the patient can maintain the position, it indicates a rupture of the sagittal band; if the patient cannot maintain the position, it indicates an extensor tendon rupture (or a nerve palsy).
A closed rupture of the sagittal band should be suspected in patients who present with an inability to extend the finger after blunt trauma to the dorsum of the hand. This can be confirmed by passively placing the patient’s digit in extension and observing whether the patient can actively maintain the position. If the patient can maintain the position, it indicates a rupture of the sagittal band; if the patient cannot maintain the position, it indicates an extensor tendon rupture (or a nerve palsy).
 The ability to extend the MCP joint does not necessarily mean that the extensor tendon is in continuity. The patient may still be able to extend the finger using the adjacent extensor tendon via the juncturae tendineae.
The ability to extend the MCP joint does not necessarily mean that the extensor tendon is in continuity. The patient may still be able to extend the finger using the adjacent extensor tendon via the juncturae tendineae.