CHAPTER 10. Euthanasia, assisted suicide and the nursing profession
L earning objectives
▪ Define and differentiate between the terms ‘euthanasia’, ‘assisted suicide’ and ‘mercy killing’.
▪ Explain why dictionary definitions of euthanasia can be misleading when considering the ethics of euthanasia and assisted suicide.
▪ Outline five conditions that must be satisfied in order for an act to count as an instance of euthanasia.
▪ Differentiate between six types of euthanasia commonly discussed in the bioethics literature.
▪ Discuss critically at least:
• six arguments commonly raised in support of euthanasia and assisted suicide
• seven arguments commonly raised against euthanasia and assisted suicide.
▪ Discuss critically the possible impact of climate change on the euthanasia debate.
▪ Discuss critically the nature and moral implications of ‘psychiatric euthanasia’.
▪ Examine critically the killing/letting die distinction.
▪ Discuss critically the issue of terminal sedation associated with the withholding of artificial hydration and nutrition at the end stage of life.
▪ Construct critical arguments for and against the proposition that the nursing profession should support the legalisation of euthanasia and assisted suicide.
I ntroduction
In 1990, in the United States (US), Janet Adkins, a 54-year-old newly diagnosed with early Alzheimer’s disease, died after pushing a red button on a suicide machine — or ‘mercitron’, as it has been called — designed by a retired pathologist, Dr Jack Kevorkian, whom she had approached for assistance to die (Gibbs 1993, 1990a). Adkins, who is reported to have ‘feared an excruciating future’, soon came to be viewed as a ‘symbol of all those patients who confront a horrible disease and vow to maintain some dignity in death’ (Gibbs 1990a: 70). Dr Kevorkian, meanwhile, found himself in the forefront of the pro-euthanasia debate and, as Time Magazine put it:
a standard-bearer for all those who fail to see a moral difference between unplugging a respirator and plugging in a poison machine.
(Gibbs 1990a: 70)
Despite being dubbed ‘Dr Death’, Dr Kevorkian continued his crusade for the legalisation of euthanasia/assisted suicide, or, as he called it, ‘medicide’ in the US (Gibbs 1993: 52; see also Brovins & Oehmke 1993; Kevorkian 1991). As part of this crusade, in December 1998 Dr Kevorkian was successful in getting authorities in the state of Michigan (US) to charge him with first-degree murder after he admitted, for the first time, having directly administered a fatal injection to one of his patients (Riley 1998a, 1998b, 1998c; see also Magnusson 2002: 28–32). In all other cases (130 in total), Dr Kevorkian admitted only to presiding over the suicides of his patient; that is, ‘instructed the patients and supervised them while they activated an injection from his so-called “suicide machine” ’ (Riley 1998c: ii; see also Riley 1999a, 1999b).
Dr Kevorkian’s case went to trial in March 1999, representing the fifth time he had been tried over the deaths of his patients. On 26 March 1999, the jury returned a verdict of second-degree murder and he was sentenced to serve 10–25 years in the Michigan State Prison (Magnusson 2002: 28–32). In passing her sentence, the judge presiding over the case stressed that the trial was not about ‘the political or moral correctness of euthanasia’, but about lawlessness and murder (AFD, DPA 1999). Referring to a national television broadcast several months earlier in which Dr Kevorkian dared legal authorities to arrest him for his actions, the judge responded:
You had the audacity to go on national television, show the world what you did and dare the legal system to stop you. Well, sir, consider yourself stopped.
(Judge Jessica Cooper, reported comments cited by AFP, DPA 1999)
In the Netherlands, during the same period, a very different scenario was at play. In contrast to the US, euthanasia and assisted suicide was, at the time of Janet Adkins’ medically assisted death, legally tolerated (although still a criminal offence). By the time Dr Jack Kevorkian had facilitated his first ‘assisted suicide’ in 1990, Dutch doctors had already participated in thousands of medically assisted deaths. In 1986, for example, the Royal Dutch Medical Association reported that there were between 5000 and 6000 cases of voluntary euthanasia each year in the Netherlands (British Medical Association 1986). In 1990, the overall incidence of euthanasia was estimated by formal sources to be between 4000 and 6000 deaths annually (de Wachter 1992: 24). In 2001 it was reported that approximately 2500 cases of euthanasia were notified to authorities in the previous year, with another 1000 cases going unreported ‘because of “grey” areas in the law’ (Mann 2001: 17). Some contend that the overall incidence of euthanasia is, in reality, unknown and, if informal sources are to be relied upon, could range from 2000 to 20000 cases a year (de Wachter 1992; Keown 1992; ten Have & Welie 1992).
Today, the Netherlands is one of only two countries (the other being Belgium) in which euthanasia is legal (euthanasia was legalised in the Netherlands in 2001, followed by Belgium in 2002) (de Beer et al 2004; Daverschot & van der Wal 2001; Dupuis 2003). This means that under certain clearly defined conditions that have undergone ‘subtle elaborations over the past three decades’, euthanasia and assisted suicide are no longer viewed by the courts as a punishable offence (Magnusson 2002: 64–5). In 1993, legislation was passed clarifying and affirming the strict conditions under which euthanasia and assisted suicide were permitted. The passage of this new law was reported at the time as giving the Netherlands the world’s most lenient policy on ‘mercy killing’ (Hirschler 1993: 7). Seven years later, the leniency of the Dutch ‘mercy killing’ laws was expanded even further when statutory support was given for the first time to the defence of ‘necessity’ (passed by the lower house of the Dutch parliament in November 2000, and the upper house in April 2001) (Magnusson 2002: 65). The defence of ‘necessity’ permits a doctor to avoid legal liability for assisted deaths on the grounds of professional duty; that is, ‘to reduce suffering and respect the autonomy of the patient’ and provided that he or she (the euthanasing doctor) can demonstrate that ‘due care’ was exercised in determining that the patient’s request ‘was voluntary and well-considered, that the patient’s suffering was unbearable, and that there is no prospect of improvement’ and no ‘reasonable’ alternative (Magnusson 2002: 65). Significantly, under the ‘due care’ requirements:
it is not necessary for the patient to be suffering physical pain: unbearable mental anguish is sufficient. Similarly, there is no requirement for the patient to be in a terminal phase of an illness, or indeed to be suffering from any (physical) condition at all. A physical disability, or a condition of ‘untreatable misery’ … will suffice.
(Magnusson 2002: 65)
The above legislative reforms have not only given the Netherlands the world’s most lenient policy on euthanasia and assisted suicide, but as some have noted has also given the world a ‘laboratory’ for ‘testing’ and ‘observing’ these practices — and one which has attracted many onlookers from both ends of the moral spectrum in regard to the moral permissibility of euthanasia. Certainly, the Netherlands is currently the only country in the world which is able to offer retrospective studies of substance concerning the practice of euthanasia and any emerging patterns or trends associated with it (see, e.g. Bindels et al 1996; Dupuis 2003; Onwuteaka-Philipsen et al 2003; van der Maas et al 1996; van der Wal et al 1996).
In 1996, Australia became the subject of international attention when it became the first country in the world to fully legalise active voluntary euthanasia. This followed the passage, in May 1995, of the Northern Territory’s controversial Rights of the Terminally Ill Act 1995, which came into effect on 1 July 1996. Almost 1 year later, however, the Act was overturned by the Australian Federal government — although not before five people had sought assistance to die under the Act. Of these people, four were successful in achieving legally assisted deaths; the only person not successful in achieving his wish was eligible for assistance to die under the Act but was ‘unable to find a specialist who was prepared to be one of the three doctors required under the Act’ to certify eligibility for an assisted death (Senate Legal and Constitutional Legislation Committee 1997: 11). To date, despite the success of the Australian Federal government in overturning the Northern Territory’s euthanasia legislation, proponents of euthanasia speculate that it will only be a matter of time before euthanasia and assisted suicide will be legal in not just one, but possibly all jurisdictions in Australia.
In 2002, in what has been described as an unprecedented and ‘landmark legal case’, a British High Court judge ruled that a competent 43-year-old woman with quadriplegia and unable to breathe unaided, had the ‘right to die’ and to have the ‘machine keeping her alive’ switched off ( Herald-Sun 2002: 7). This ruling stands just less than a decade after a House of Lords Select Committee report released in 1994 opposed legalising euthanasia in England (Magnusson 2002: 66). A year later in Australia, in what has also been described as a ‘landmark decision’, a similar ruling was made. In what has become known as the ‘tube woman case’, a Victorian Supreme Court judge ruled that a 68-year-old woman (known only as BMW) suffering from a rare and fatal brain disease, who had been kept alive for 3 years by artificial tube feeding, be allowed to die (Davies 2003: 5). The judge is reported to have said that her ruling would now make it possible for the woman’s advocate ‘to decide, on behalf of BMW, whether it is now time to allow her to die with dignity’ (Davies 2003: 5). It was noted, however, that once the tube feeds were stopped, it could take between 1 and 4 weeks for the woman to die. Margaret Tighe, President of Right to Life Australia, is reported to have criticised the court decision, arguing that it was ‘not an act of love to kill somebody by dehydration and starvation’ (Davies 2003: 5).
In 2005, after Hurricane Katrina had devastated the US city of New Orleans, a new and largely unanticipated dimension was added to the euthanasia debate, notably, climate change. In the aftermath of Hurricane Katrina, allegations were made that ‘mercy killings’ had occurred at the city’s Memorial Medical Centre, leading to autopsies being requested on 45 bodies taken from the hospital after the storm (Johnston 2005; Lugosi 2007). As the inquiries progressed, it was gradually revealed that four nonambulatory patients, aged between 61 and 90 years of age, had been ‘euthanised’ in an attempt to prevent their needless suffering in the face of having ‘no realistic chances of surviving in a stranded, incapacitated hospital’ (Curiel 2006: 2067). The four patients, who were allegedly given a combined lethal intramuscular dose of the drugs morphine and midazolam, were among 24 patients who died in the Life Care Unit situated on the 7th floor of the Memorial Medical Centre.
The environmental conditions at the time were extreme. According to one CNN report, the medical centre had been a storm refuge for up to 2000 people, where patients, staff and their families ‘rode out the storm inside’ (Griffin & Johnston 2005). However, as CNN goes on to report,
by Thursday, four days after Katrina hit, despair was setting in. The hospital was surrounded by floodwater. There was no power, no water and stifling heat. Food was running low. Nurses were forced to fan patients by hand. And outside the hospital windows, nurses … saw looters breaking into a credit union … The hours, and then days, passed with only the occasional boat or helicopter stopping by to pick up patients. On Thursday, according to people who were there, there was a shift in tone at the hospital …
(Griffin & Johnston 2005)
It is alleged that nurses started to discuss ‘who would be evacuated and, for the first time, who would not’, for example, patients who were ‘DNR’ (do not resuscitate) (Griffin & Johnston 2005). It was further reported that ‘at about the same time, some members of the hospital staff were discussing euthanising patients’ (Griffin & Johnston 2005). Although, none of the four patients in question were expected to die immediately from natural causes, were in pain, or had consented to the drugs they were given, they did have one thing in common: they were all the subject of a consented ‘Do Not Resuscitate’ (DNR) directive. As one commentator has noted, however, no one had warned the patients that ‘in case of a natural disaster, hospital administrators would interpret DNR to mean “Do Not Rescue” ’ (Lugosi 2007: 74).
In July 2006, a New Orleans physician (Dr Anna Pou) and two nurses (Lori Budo and Cheri Landry) were arrested and charged with second-degree murder in relation to the patients’ deaths, sparking public debate on whether the killings were ‘murder or mercy’ (Curiel 2006; Griffin & Johnston 2005; Johnston 2007; Lugosi 2007; Nossiter & Dewan 2006; Safer 2006, 2007; Skipp & Campo-Flores 2006). Commenting on the case, Curiel raised a number of important questions, including: What might lead a health care professional to consider euthanasia in such a situation? and Were the Memorial staff prepared to make life-and-death decision during a disaster, and, if not, what could have prepared them? — pointing out that tsunamis, earthquakes, fires and other calamities ‘are present and evolving threats that can rattle unprepared respondents to the core and expose complex ethical, legal and medical conundrums’ (Curiel 2006: 2067 & 2068).
While acknowledging the extreme conditions under which health care providers were operating at the time, Curiel nonetheless found it ‘unimaginable’ that effective team decision-making would have — and could have — led to a decision to euthanise patients (Curiel 2006). Referring to his own experience in the aftermath of Katrina, Curiel writes:
Katrina’s flood waters crippled emergency power generators, transforming hospitals into dark, fetid, dangerous shells. Extremely high indoor temperatures killed some people. We were under tremendous strain: in addition to the dire medical circumstances of many of our patients, we confronted uncertainty about our own evacuation, exacerbated by the tensions of threatened violence by snipers and frazzled soldiers and guards. I saw some competent professionals reduced to utter incoherence and uselessness as the crisis unfolded. I saw others perform heroic deeds that surprised me.
(Curiel 2006: 2067)
He concludes that if the allegations against the physician and two nurses in the Katrina case are ‘borne out’, then:
… such behaviour might be attributable to less effective group decision making, lack of a sense of control, or individual actions that were contrary to group decisions, in addition to environmental or medical conditions that were judged not to be survivable, requests of patients, or criminal intent.
(Curiel 2007: 2068)
Other commentators have been more circumspect. Lugosi (2007), for example, warns that the killings have served unacceptably to model ‘a new way to manage patients when natural disaster strikes — the non-consensual deceptive killing of patients that are too difficult to move because of logistics or lack of resources’ (p 76). Controversially, he has also suggested that racism and poverty may have influenced the decisions made that day, pointing out that another feature that all four patients had in common was that they were black and poor (p 78).
In June and July of 2007, the two nurses and then the physician were respectively all cleared of criminal charges after a New Orleans grand jury decided not to indict them ( American Medical News 2007; Jervis 2007). However, as CBS reports, ‘the case continues to resonate and raise questions about ethics, and compassion in what has been described as battlefield conditions’ (Safer 2007).
Euthanasia and assisted suicide continues to receive widespread attention both locally and globally, and remains the subject of much controversy. Central to the controversy is the fundamental question of whether a doctor should intentionally and actively assist a patient to die, and, if so, under what circumstances and by what means. These same questions can (and should), of course, also be asked of nurses — particularly given the fundamental role nurses play in caring for and promoting the dignity of patients who are incurably ill, suffering intolerably, dying (Asch 1996; Berghs et al 2005; Bilsen et al 2004; Crock 1998; Daverschot & van der Wal 2001; de Beer et al 2004; Gastmans et al 2006; van der Arend 1998), or, as has just been considered above, left hopelessly stranded by catastrophic emergency events linked to climate change.
In this chapter, attention is given to examining the nature and moral implications of the euthanasia/assisted suicide question for nurses. Attention is also given to clarifying what euthanasia is, how it differs from assisted suicide and ‘mercy killing’, and the kinds of moral arguments that can be raised both for and against the legitimation of euthanatic practices. It is hoped that by examining these and related issues, members of the nursing profession will move a step closer towards answering the following kinds of questions:
▪ How significant or important is the euthanasia/assisted suicide issue for the nursing profession?
▪ Should the nursing profession take a formal position either way on the euthanasia/assisted suicide question (e.g. should nursing organisations adopt formal position statements advocating a particular view on the moral permissibility or impermissibility of euthanatic practices, or is this a matter that should be left to individual nurses to decide conscientiously)?
▪ To what extent, if at all, should the broader nursing profession participate in public debate on the euthanasia/assisted suicide question (e.g. should nursing organisations actively lobby for the legalisation of euthanasia/assisted suicide)?
▪ In the event of euthanasia/assisted suicide being decriminalised, what (if any) should be the role of nurses in regard to assisting with or actually performing euthanasia and/or assisted suicide?
▪ How best can the nursing profession proceed to answer these and related questions (see also Johnstone 1996a)?
E uthanasia and its significance for nurses
Next to abortion, euthanasia is probably one of the most controversial bioethical issues to have captured the world’s attention. And, like the abortion issue, it is unlikely to be resolved to the satisfaction of all concerned.
Euthanasia and the so-called ‘right to die’ are not new issues for nurses. In Australia, one of the first articles addressing the subject was published as early as 1912 in the Australasian Nurses Journal. Reprinted from the British MedicalJournal, the article contains concerns and viewpoints which remain current — including the agonising question of whether euthanasia should be legalised. Citing an 1873 essay on the subject, the article contends that ‘a modified harikari should be made lawful in England’ (and, one presumes, her colonies, including Australia), and, quoting the essay’s author, that: ‘On the whole it cannot be doubted that the benefits resulting from a change in the law would be simply enormous’ (Lionel Tollemache, cited in the Australasian Nurses Journal 1912: 304).
While euthanasia may not be a new issue for nurses, it has nevertheless become a more complex, intense and significant one. Evidence of this can be found in the increased attention being given to the experiences of nurses in regard to euthanasia in both the professional and lay press over the past 20 years or so. In 1987, for example, the English nursing periodical Nursing Times carried a provocative report on the fate of four Dutch nurses who had been arrested in Amsterdam after it was alleged they had practised euthanasia on three hopelessly ill patients. The report concluded that, if the nurses were found guilty of killing the patients, they could face prison sentences of up to 20 years ( Nursing Times 1987: 8).
Almost a decade later, in another (although unrelated) case in 1995 in the Netherlands, a 38-year-old Dutch registered nurse was given a 2-month suspended prison sentence for performing active voluntary euthanasia on a patient suffering end-stage AIDS (Staal 1995: 7; van de Pasch 1995; van der Arend 1995; see also Daverschot & van der Wal 2001). What was particularly significant about this case was that the sentence was passed despite the fact that:
▪ the patient (who was a friend and colleague of the nurse) had specifically requested that the nurse perform the act of assisted death; and
▪ the procedure fully complied with legal regulations governing euthanatic practices in the Netherlands (for example, the patient had competently requested assistance to die, he was suffering from an end-stage illness, a second medical opinion had been obtained, and the procedure was fully attended to and supervised by a qualified medical practitioner [who, significantly, escaped sentence]).
(van de Pasch 1995: 108)
As I have discussed elsewhere (Johnstone 1996c: 21–2), this case helped to demonstrate the tenuous position of nurses in relation to euthanatic practices — even in countries where euthanasia and assisted suicide are ‘legally tolerated’. In this case, the court’s decision seemed to hinge on the view that euthanasia and assisted suicide were medical procedures of a nature that could not (and should not) be delegated to nurses. More specifically, the court clarified that the deed of ‘ultimate care’ (the procedure that is the act of euthanasia itself) could only be performed by a doctor and could not be delegated to anyone else (Daverschot & van der Wal 2001; Staal 1995: 7).
Nurses in the United Kingdom (UK) have also experienced significant problems in relation to the euthanasia issue. For example, in 1991, a UK registered nurse experienced threats of violence and obscene phone calls, was vilified by some sections of the media, and was made a scapegoat in the eyes of the public after reporting to the appropriate authorities that a terminally ill patient had died possibly as a result of being administered 10 mmol of potassium chloride by a consultant physician, Dr Nigel Cox (Hart & Snell 1992: 19). The incident was discovered after nurses noted the blatant documentation of the drug administration in the patient’s case history which ‘had been left in the nurses’ station for all to see’ (Hart & Snell 1992: 19). The registered nurse’s attempts to contact Dr Cox about the matter were unsuccessful. Not wishing to implicate other staff in the matter and recognising her professional duties as prescribed in the United Kingdom Central Council for Nursing, Midwifery and Health Visiting (1992) Code of Professional Conduct, the registered nurse decided that she ‘had no choice but to report the incident’. Accordingly she notified the director of nursing services and the unit general manager. One month later, Dr Cox was convicted of attempted murder at Winchester Crown Court, after the justice hearing the case rejected the argument that ‘Cox’s intention in injecting lethal quantities of a drug which lacked analgesic properties was to relieve pain, rather than to kill’ (Magnusson 2002: 26). He subsequently received a 1-year suspended prison sentence (Hart & Snell 1992: 19). He was not deregistered by the General Medical Council (UK), however, and continued to practise medicine. The registered nurse meanwhile carried a disproportionate burden of suffering for her actions.
Besides sometimes finding themselves unwitting witnesses to the illegal euthanatic practices of others, there is anecdotal evidence, some published research and a number of court cases suggesting that a small percentage of nurses (e.g. in the US, Hungary, Australia, England and the Netherlands) have also taken active steps to bring about the death of a patient themselves (Rozsos 2003; Magnusson 2002; Crock 1998; Kitchener 1998; Asch 1996; Walsh & Pirrie 1996; Staal 1995; Stevens & Hassan 1994; Kuhse & Singer 1992, 1993; Turton 1992). One commentator has even alleged controversially that British nurses are ‘often’ involved in performing euthanasia on patients:
British nurses are often involved in euthanasia; but that due to the illegality of euthanasia practices, it is difficult to assess the exact extent of the problem — particularly in a culture which prescribes that nurses should not ‘tell on colleagues’.
(Turton 1992: 92–3)
Euthanasia and assisted suicide is, however, a controversial issue for nurses in the UK (Johnstone 1996c). Significantly, the prestigious Royal College of Nursing (RCN), a leading professional nursing organisation in the UK, has historically and unequivocally rejected the role of nurses in participating in euthanasia. This position has been made explicit in an issues paper on living wills. In this paper, the RCN takes the following position (RCN 1994):
The RCN believes that this [euthanasia] is contrary to the public interest and to the medical and nursing ethical principles as well as to natural and civil rights.
It further asserts:
The RCN is opposed to the introduction of any legislation which would place on doctors or nurses a responsibility to respond to a demand for termination of life from any patient or from their relatives.
In 2003, the RCN’s opposition to euthanasia was reaffirmed by its General Secretary, Dr Beverly Malone, who reportedly stated in an RCN media release:
The RCN is against euthanasia and assisted suicide. Euthanasia is illegal and the RCN does not condone it. The RCN believes that the practice of euthanasia is contrary to the public interest, to nursing and medical ethical principles as well as patients’ civil rights. The RCN is opposed to the introduction of any legislation which would place the responsibility on nurses and other medical staff to respond to demand for termination of life from any patient suffering from intractable, incurable or terminal illness.
(StaffNurse.com 2003)
In 2004, after a survey of its members found that 70% did not support a ‘softening’ of its stance against the legalisation of euthanasia, the RCN again reiterated its opposition to the legalisation of euthanasia and assisted suicide (McDougall 2004; Hawkes 2005). In response to a House of Lords select committee on an assisted dying Bill, the then RCN Vice-President, Maura Buchanan (now president of the RCN), was reported to have said: ‘Our patients do not want nurses and doctors to be skilled in delivering lethal injections’ (quoted by BBC News 2005).
The euthanasia/assisted suicide question has also proved to be a significant professional issue for Australian nurses. For example, in January 1995, recognising the seriousness of the euthanasia issue for members of the nursing profession, the Royal College of Nursing, Australia (RCNA) took the unprecedented step of releasing for comment a discussion paper entitled ‘Euthanasia: an issue for nurses’ (Hamilton 1995). As I have discussed elsewhere (Johnstone 1996b), the RCNA received over 70 responses to this discussion paper from concerned and interested nursing organisations, groups and individuals from around Australia. The responses received represented nurses working in a variety of clinical areas and fields of nursing (including education) and reflected a great diversity of knowledge, opinion, values and beliefs about euthanasia and assisted suicide. In some cases, the responses also demonstrated an overwhelming need for information and guidance on how best to respond to the uncertainty, controversy, complexity and perplexity that has become so characteristic of the right to die movement generally. Perhaps most confronting of all, however, was the emerging difficult question of whether the nursing profession should formally and publicly support the legalisation of active voluntary euthanasia. Related to this was the equally confronting question of whether representative nursing organisations should adopt a formal position statement either supporting or rejecting the role of nurses in active voluntary euthanasia and assisted suicide. Not surprisingly, while the responses demonstrated the need to raise and address these troubling questions, they fell far short of offering a definitive answer to them. Recognising the complexity and perplexity of the issue, the RCNA subsequently commissioned, as part of its professional development series, a monograph entitled: The politics of euthanasia: a nursing response (Johnstone 1996a). The purpose of this monograph was not to provide nurses with definitive answers to the difficult questions posed by the euthanasia debate. Rather, it was to advance a discussion that would enable nurses ‘to formulate their own thinking and viewpoints on the subject and to be able to contribute to broader professional discussion on the whole issue of the right to die’ (Johnstone 1996b: 22). In July 1996, the RCNA also issued its first position statement on voluntary euthanasia and assisted suicide — subsequently revised and reaffirmed respectively in 1999 and 2006 (Royal College of Nursing, Australia 1996, 1999, 2006). This position statement primarily focuses on clarifying the illegal status of euthanasia/assisted suicide in Australia, acknowledging that there exists a diversity of moral viewpoints on the euthanasia issue, reminding nurses of their professional responsibility to be reliably informed about the ethical, legal, cultural and clinical implications of euthanasia and assisted suicide, and recognising and supporting the appropriateness of nurses taking a ‘conscientious’ position on the matter.
The RCNA’s initiatives (just outlined above) were to prove extremely timely, coinciding as they did with the enactment of the Northern Territory of Australia’s controversial Rights of the Terminally Ill Act 1995 which came into effect on 1 July 1996. As already stated in the opening paragraphs of this chapter, the passage of this legislation earned Australia the controversial distinction of being the first country in the world to legalise active voluntary euthanasia. Of significance to nurses (and to this discussion) is that the legislation anticipated and provided for nurse participation in active voluntary euthanasia and assisted suicide (either by way of preparing, or being delegated the task of actually administering, a substance to terminate life [see section 16(1); see also Trollope 1995: 21]). What, arguably, was troubling about the legislation’s provisions in regard to nurse participation was that they had been enacted even before the broader nursing profession itself had:
▪ clarified its position on the euthanasia/assisted suicide question (at the time, the issue had not been widely discussed in the Australian nursing literature, and policy statements on the subject were either non-existent, inadequate or only at draft stage)
▪ taken the necessary steps to ensure that its membership had been fully informed about and adequately prepared to deal with the complex range of political, social, cultural, moral, legal and clinical issues raised by public policy innovation and legal ratification of active voluntary euthanasia and assisted suicide (Johnstone 1996b).
Significantly, in May 1996, less than 2 months before the Rights of the Terminally Ill Act 1995 (NT) came into effect, the Nurses’ Board of the Northern Territory took the unprecedented step of formulating and ratifying a formal position statement on euthanasia (see Nurses’ Board of the Northern Territory Position Statement on the Nurse’s Role in Euthanasia, included in full as Appendix 5 in Johnstone 1996a). This position statement was keyed to the Rights of the Terminally Ill Act 1995 (NT) and sought to clarify the role and function of nurses in relation to the Act’s provisions. Specifically, the position statement supported:
▪ the role of nurses assisting in the voluntary euthanasia of competent patients; and
▪ the rights of nurses to conscientiously refuse to participate in the euthanasia of patients (Johnstone 1996c: 36).
The position statement also outlined the obligations of nurses in regard to the ethical and legal aspects of euthanasia, employment policies, professional competence and education (Johnstone 1996c: 36–7).
As stated earlier, the decriminalisation of euthanasia and assisted suicide in the Northern Territory of Australia was short-lived. Less than 1 year after its enactment, intense political pressure resulted in the Rights of the Terminally Ill Act 1995 (NT) being overturned by the Australian Federal government. Currently, euthanasia and assisted suicide is illegal in Australia, and anyone who wilfully assists a person to die would be viewed by the courts as having committed the criminal offence of homicide (Wallace 1991: 265, ss. 14–65; see also Forrester & Griffiths 2005; Magnusson 2002). As Dix et al warn (1996: 339, s. 1223):
It should be made very clear from the outset that the law does not allow mercy killing. Where a person takes steps to end, or hasten the end of another person’s life with the intention or the knowledge that this is likely to be the consequence of his or her actions, such a person may be liable for murder or, should death not eventuate, attempted murder. The sentence for murder is imprisonment for life, although in some jurisdictions (NSW, Vic, ACT) there is a discretion in the trial judge to order a sentence of less duration …
Despite the current legal prohibition against euthanasia and assisted suicide in Australia, Magnusson (2002: 272) asserts that it is a ‘virtual certainty’ that many medical practitioners are ‘heavily involved in assisted death’. Magnusson (2002: 24, 32) points out, however, that ‘doctors are rarely punished for their involvement in assisted death’ — even when making ‘front page news’ with admissions of having performed euthanasia. This is the situation not only in Australia, but also in the UK and the US. For example, in the US, between 1950 and 1991, only 11 doctors were prosecuted for euthanasia (Cox 1993: 234). Thus, while euthanasia as such is illegal, it nevertheless seems to be tolerated where it can be shown that the intention was ‘therapeutic’ (i.e. to alleviate suffering) rather than homicidal (i.e. to kill).
In Australia, proponents of euthanasia/assisted suicide speculate that it will only be a matter of time before euthanasia and assisted suicide will be legal in all jurisdictions in Australia. In light of the looming health and welfare implications of climate change (scientists are warning that ‘changes to the environment are rapidly becoming a threat to many of our life support systems’ [Anderson 2007: 10; Haines & Patz 2004; McMichael et al 2006]), and the perceived need of some to have an ‘exit strategy’ if and when stranded by climate change, impetus for the legalisation of euthanasia is likely to take on a whole new dimension. Given these predictions, there is ample room to speculate that it will only be a matter of time before Australian nurses will once again have to grapple with the complex and perplexing questions raised by the legalisation of euthanasia/assisted suicide, and, in particular, the possible and actual implications of this for nurses at a personal, professional, societal and political level (Johnstone 1996a).
P ublic opinion on the euthanasia/assisted suicide issue
In reaching a position on the euthanasia/assisted suicide issue, it might be tempting to appeal to and/or be persuaded by public opinion on the matter. Consider the following.
Over the past two decades, public opinion polling in Australia, Canada, Europe and the US suggests majority support (around 75%) for the legalisation of euthanasia and physician-assisted suicide (Marcoux et al 2007; Voluntary Euthanasia Society [VES] 2003; Somerville 1996; Kuhse 1991; Australian Dr Weekly 1990: 9; Kuhse & Singer 1988; Humphries 1983; Radic 1982; see also Gallup polling at http://www.gallup.com/). In Australia, for example, opinion polls conducted by Morgan and Newspoll respectively during 1995 and 1996 showed 75–78% public support for physician-assisted suicide. In 2007, a national Newspoll report (prepared for Dying with Dignity Victoria) found that around 80% of the 2423 respondents surveyed by telephone thought that doctors ‘should be allowed to provide a lethal dose to a patient experiencing unrelievable suffering and with no hope of recovery’ (Newspoll Market Research 2007: 6). In 2002, a UK public opinion poll indicated that 81% of those surveyed supported the legalisation of euthanasia for people suffering unbearably from a terminal illness (VES 2003). Similar support has also been indicated by public opinion polls conducted in France (88%), Belgium (72%), Germany (75%), Italy (75%), the Netherlands (85%), Spain (70%) and the US (75%) (VES 2003). Just what is to be made of this public opinion, however, is open to question.
As discussed earlier in Chapter 2 of this book, public opinion is not a reliable guide to moral conduct; all that it tells us is that a certain group of people hold a particular opinion, not that the opinion held is ‘morally right’ all things considered. In short, it tells us nothing about the moral acceptability or the moral authority of the opinion held. We must therefore look elsewhere (i.e. beyond public opinion) to guide our deliberations on whether euthanasia and assisted suicide are morally right or wrong. It is to looking ‘elsewhere’ that the remainder of this chapter will now turn. This exploration will begin firstly by clarifying what euthanasia is, and how, if at all, it differs from other end-of-life practices such as assisted suicide and ‘mercy killing’. This, in turn, will be followed by a critical examination of views popularly raised for and against the legitimation of euthanasia and assisted suicide.
D efinitions of euthanasia, assisted suicide and ‘mercy killing’
E uthanasia
The term euthanasia comes via New Latin from Greek eu (meaning ‘easy’, ‘happy’ or ‘good’) and thanatos (meaning ‘death’); it is translated literally as ‘good death’ or ‘happy death’. Contrary to popular opinion, the Greeks did not use the term euthanasia (or equivalents) to imply either ‘a means or method of causing or hastening death’ (Carrick 1985: 127). Rather, it was used in a broader and somewhat metaphorical sense ‘to describe the spiritual state of the dying person at the impending approach of death’ (p 127). Historical evidence also suggests that euthanasia, as we understand it today, was in fact prohibited in ancient medical circles (p 81). Plato, for one, even went so far as to suggest that physicians who attempt to poison another ‘must be punished by death’, whereas the lay person who attempted such a thing should only be fined — indicating that physicians were regarded as having the greater burden of responsibility to refrain from causing death (p 83). Carrick comments that ‘if someone’s life was terminated without his (sic) consent, normally this was prima facie a case of homicide’ (p 128).
Contemporary English definitions of euthanasia vary. The Oxford English Dictionary, for example, defines it as ‘the action of inducing a quiet and easy death’, and the Collins Australian Dictionary (2005) as ‘the act of killing someone painlessly, especially to relieve suffering from an incurable illness’. Webster’s Dictionary, similarly, defines euthanasia as ‘an act or practice of painlessly putting to death people suffering from incurable conditions or disease’.
Whether euthanasia is any of these things, however, is a matter of some controversy. For example, we can imagine a case of ‘inducing a quiet and easy death’ which is a case not of euthanasia but of cold-blooded murder. I could, for example, slip a calming and sleep-inducing sedative into my fit grandmother’s nightcap, and the moment she starts blissfully sleeping in her armchair administer to her a lethal dose of intravenous morphine. My sole intention might be nothing more than to secure her premature death so that I may receive the large inheritance I know she has left me in her will. There is something about this example which, to borrow from Beauchamp and Davidson (1979: 295) ‘omits all the subtle aspects of our notion of euthanasia’. Likewise, we can imagine cases involving patients with incurable diseases or conditions who would nevertheless not be candidates for euthanasia. Diabetes, for example, is an incurable disease, and colour blindness an incurable condition. Yet, we would not, I think, regard either of these incurable states as grounds for euthanasia.
The notion of ‘painlessly’ inducing death is also unhelpful. We can, for example, imagine a painless means of causing death (e.g. injecting a lethal substance through the side arm of an intravenous line, or removing someone from a life-support system or withholding food and fluids) but where the death itself is nevertheless painful and/or distressing (e.g. where a patient is acutely aware of the sensations of suffocation after being taken off a respirator or after being given a large dose of narcotics, or is aware of both hunger and thirst sensations when food and fluids have been withheld). Just because the means of death was ‘pain-free’, it does not always follow that the death itself was a ‘good death’.
All three dictionary definitions are also inadequate in that they say nothing about the kinds of reasons which should be considered for killing another person, leaving it wide open for motivations of self-interest to be admitted (Beauchamp & Davidson 1979: 295). The questions remain: How should euthanasia be defined? How can we be sure that a given act is an act of euthanasia rather than some other kind of act, such as murder or unassisted suicide?
In a classic article on defining euthanasia, Beauchamp and Davidson (1979) argue that for an act to be an instance of euthanasia, it must satisfy at least five conditions.
1. Intentionality. Death must be intended and not be merely accidental, and further must be intended by at least one other human being.
2. Suffering and evidence of suffering. Here suffering may be in the form of conscious pain, mental anguish, and/or serious self-burdensomeness (as may occur in cases of high quadriplegia, or tetraplegia, or the like). This interpretation of suffering fully upholds the view that ending a person’s pain is not always tantamount to ending that person’s suffering (see also Cassell 1982, 1991; Kuhse 1982; Hill 1992; Starck & McGovern 1992). In assessing a person’s level of suffering, every effort must be made to gain ‘sufficient current evidence’ (Beauchamp & Davidson 1979: 301); in this instance, it is simply not enough to rely on mere guesswork or on supposition based on ignorance.
3. Reasons for death and the means of death. Beauchamp and Davidson contend that death-causing acts must be motivated by beneficence or other humanitarian considerations (such as the demand to end suffering). Killing acts which are not motivated by these things are not acts of euthanasia, but murder. Further to this, any means of death chosen must also be of a nature that does not cause more suffering than is already being experienced (Beauchamp & Davidson 1979: 302).
4. Painlessness. This condition is related to the previous one and demands, quite simply, that any death act performed must be as painless and as merciful as possible. Beauchamp and Davidson (1979: 303) explain that if the means of bringing about death causes more suffering than if that particular means was not used, then the individual will be effectively deprived of a ‘good death’.
5. Non-fetal humanity. Beauchamp and Davidson (1979: 303) contend that if this simple qualification is not included then we would not be able to distinguish acts of abortion from acts of euthanasia.
Beauchamp and Davidson (1979) maintain that the five conditions they have formulated supply a ‘non-prescriptive definition’ of euthanasia, and thus one which avoids dictating a particular moral conclusion. Whether they have succeeded, however, is another matter. The definition still seems ethically loaded, and therefore carries prescriptive meanings. Nevertheless, the five conditions given supply an important step towards the formulation of an operational definition of euthanasia, and one which can be meaningfully applied in the euthanasia debate.
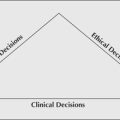
Active euthanasia, meanwhile, typically involves a deliberate act (or commission) which results in the patient’s death. The deliberate act of administering a lethal injection or a lethal dose of pills is an example of active euthanasia. This type of euthanasia is sometimes referred to as positive euthanasia. Passive euthanasia, on the other hand, involves a deliberate omission or the withholding of certain life-supporting cares and treatments. Withholding antibiotics, nutrition and fluids, mechanical life supports, or other life-supporting measures from terminally or chronically ill patients are examples of passive euthanasia. This type of euthanasia is sometimes referred to as negative euthanasia (Glaser 1975).
The six types of euthanasia just outlined can be expressed diagrammatically, as shown in Figure 10.1.
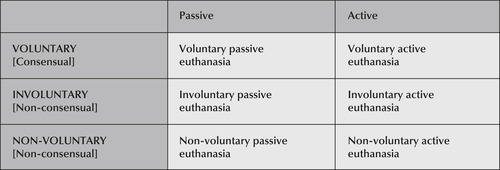 |
| Figure 10.1 |
A ssisted suicide
The term ‘euthanasia’ (and, more specifically, voluntary active euthanasia) is sometimes used interchangeably with the term ‘assisted suicide’. As I have explained elsewhere (Johnstone 1996c), this interchanging usage is not, however, strictly correct. While it is acknowledged that there may be no morally significant difference between voluntary active euthanasia and assisted suicide (see Brock 1993: 204; Parker 1994: 34–42), there is nevertheless a qualitative (experiential) difference between them. With assisted suicide, a qualified medical practitioner supplies the patient/client with the means (e.g. a prescription for a lethal dose of drugs) for taking his or her own life but, unlike in the case of voluntary active euthanasia, it is the patient/client (not the doctor) ‘who acts last’ (Brock 1993: 204; Campbell 1992: 276). To put this another way, in the case of active euthanasia it is the qualified medical practitioner who kills the patient/client; whereas in the case of assisted suicide, the patient/client kills him or herself. Interestingly, while there may indeed be no morally significant difference between voluntary active euthanasia and assisted suicide (in both instances the ultimate choice rests with the patient/client, both involve assistance from a qualified medical practitioner [or his or her proxy, e.g. a nurse] and both result in the foreseeable and intended death of the patient/client suffering from an irreversible medical condition), the law, public policy and public opinion have all distinguished between them (Brock 1993; Glick 1992; Forrester & Griffiths 2005). A notable US example here can be found in the 1994 Oregon Death with Dignity Act (known as ‘Measure 16’) which legalised physician-assisted suicide (in the form of prescribing a lethal dose of medication), but not active voluntary euthanasia (Magnusson 2002: 64; Kuhse 1995). It has also been argued controversially that physician-assisted suicide is more defensible and hence preferable to active euthanasia since with the former ‘the willingness [by the patient] to commit suicide gives compelling evidence of the patient’s desire to die’ (Dixon 1998: 29).
‘M ercy killing’
A third terminology which has found usage in discussions on euthanasia is that of ‘mercy killing’. Although this term is also sometimes used interchangeably with the term ‘euthanasia’ it can nevertheless be distinguished from euthanasia on a contextual basis. Specifically, as Glick explains (1992: 81–2):
Mercy killing is not the same as voluntary active euthanasia since many killings are committed without patient request or consent — typically an elderly husband shoots his terminally ill and unconscious or Alzheimer’s disease-stricken wife. But the cases almost always exhibit wrenching long-term personal suffering and sacrifice and financial ruin … They evoke sympathy for both killer and victim and perpetuate interest in the legalisation [sic] of voluntary active euthanasia, which some believe might eliminate the compelling need that desperate people feel for killing their hopelessly ill spouses.
A classic example of a ‘mercy killing’ scenario can be found in the highly publicised Australian case of Raymond Riordan, a 71-year-old man, who admitted trying to kill his 71-year-old wife who was suffering from advanced Alzheimer’s disease (Haslem 1998: 3). Although pleading guilty and convicted of attempted murder (which could have carried a jail sentence of up to 25 years), Riordan was freed after being placed on a 3-year good behaviour bond. Justice Cummins of the Victorian Supreme Court is reported to have said that while Riordan had acted illegally, he had ‘sought to relieve (his) wife of her terrible suffering and indignity’ (Haslem 1998: 3). Describing Riordan as a ‘person of compassion and selflessness, totally devoted to his wife’, Justice Cummins stated that Mrs Riordan’s ‘deteriorating health had had a “catastrophic” effect on her husband, who sought treatment for depression’ (Haslem 1998: 3). Mr Riordan’s son, meanwhile, is reported to have told the court that he had ‘never seen two people more devoted to each other than his parents’. He is reported to have described how (Haslem 1998: 3):
Every morning they would rise at six o’clock and have brekkie [breakfast] and go for walks … They would probably cover 30km [sic] and there probably was not more than 100m [sic] they weren’t hand-in-hand.
Outside the court, Mr Riordan’s son was further reported as stating (Haslem 1998: 3):
It’s dad’s wish that not one other person … has to go through what he’s been through. He would like to see the law-makers of this country … do something about laws covering euthanasia.
V iews for and against euthanasia/assisted suicide
Like other controversial bioethical issues, euthanasia and assisted suicide have proponents and opponents. Attitudes towards them range from liberal and moderate acceptance to absolutist conservative prohibition. It is to examining some of the various viewpoints for and against euthanasia and assisted suicide that this discussion will now turn.
V iews in support of euthanasia
Those who support euthanasia typically take the view that it is morally wrong to allow people to suffer unnecessarily. As one author writes:
the most horrible thing in the world for us, living and sentient beings, is inexorable suffering pain, without any possible compensation when it has reached this degree of intensity; and one must be barbarous, or stupid, or both at once, not to use the sure and easy means now at our disposal to bring it to an end.
(Reiser 1975: 28)
Popular views advanced in support of euthanasia (and, in particular, in support of legalising it) fall roughly under four main augmentative categories:
1. arguments from individual autonomy and the right to choose;
2. arguments from the loss of dignity and the right to the maintenance of dignity;
3. arguments from the reduction of suffering;
4. arguments from justice and the demand to be treated fairly.
(adapted from Beauchamp & Perlin 1978: 217)
A fifth and controversial category of argument raised in support of euthanasia is that, in some instances, patients have a ‘duty to die’ (Hardwig 2007; Beloff 1992: 52–6) and furthermore that it might even be a violation of a person’s ‘freedom of conscience’ not to respect this duty (Lewis 2001: 60–2). A sixth argument emerging in support of euthanasia derives from all of the above, but with the significant difference that the decision-point for euthanasia is not a patient’s hopeless medical condition imposed by injury or illness, but rather a person’s hopeless life condition imposed by climate change.
Arguments from individual autonomy and the right to choose
We generally accept that people have a right to choose. And, as we have already seen in Chapter 3, the moral principle of autonomy demands that we respect other people’s choices, even if we consider them to be mistaken or foolish. The only grounds upon which a person’s autonomous choices can be justly interfered with is if they stand to impinge seriously on the significant moral interests of others. Proponents of voluntary euthanasia argue that the right to choose includes the right to choose death (abbreviated as ‘the right to die’). Given the right to die, this means that others (including the state) should not interfere with a person’s decision to die, and in some instances may even entail a positive duty to assist a person to die — as in cases where a person desires death but is physically unable to end his or her own life. Voluntary euthanasia is thought to be justified here on grounds of autonomy and the demand to respect a person’s autonomous wishes.
An important example of this can be found in the comments of Baume (1996: 17) who writes that voluntary euthanasia is justified because ‘it is a self-regarding victimless action from an individual decision in a matter which affects individuals alone’.
Arguments from the loss of dignity and the right to the maintenance of dignity
Related to the demand to respect a person’s autonomous choices is the further demand to respect and maintain a person’s dignity. Advances in medical technology have increased medicine’s capacity to prolong a person’s life. Its methods, however, are not always humane, and can seriously erode a person’s self-concept, character, sense of self-worth and self-esteem, and the like. As Beauchamp and Perlin (1978) point out, some patients ‘are not only subjected to intense and abiding pain, they are often aware of their own deterioration, as well as of the burden they have become to others’ (p 217). They conclude that under these conditions ‘it seems uncivilised and uncompassionate’ not to allow patients to choose their own death. Euthanasia in some pain states as well as in some chronic disease states may well be the most dignified option.
Arguments from the reduction of suffering
Suffering may be defined as a state of severe distress that people experience when some crucial aspect of themselves, their being or their existence is threatened (Kahn & Steeves 1986; Cassell 1991). It is important to clarify that while pain is a major cause of suffering, suffering itself is ‘not confined to physical symptoms’ (e.g. people can be in pain, yet not be ‘suffering’) (Cassell (1991). Suffering may, for example, derive from other aspects of ‘personhood’ — including the cognitive, emotional, spiritual, social and cultural aspects of a person’s identity — not just their physical aspect. Moreover, when any one or a combination of these aspects is threatened, a person may simultaneously give a cognitive, emotional, spiritual, social and other (cultural) meanings to that threat and respond accordingly (Fry & Johnstone 2008).
Suffering is generally regarded as morally unacceptable and, as discussed in Chapter 3 of this work, morality demands that, where possible, people (including the very young as well as others across the life span) should be spared or prevented from suffering unnecessarily. In cases where patients’ suffering is intense, protracted, unendurable and intractable, it seems cruel to deny them the choice of death as a means of release from their suffering. Euthanasia in these kinds of cases is said to be justified on grounds of ‘prevention of cruelty’ or ‘mercy’ (Beauchamp & Perlin 1978: 217). It is also thought to be justified on the grounds that people have the indisputable right to judge their suffering as unbearable, and the concomitant right to request euthanasia to end their unbearable suffering (see, e.g. Admiraal 1991: 11). This, in turn, is grounded in the fact that, despite the achievements of modern medicine, doctors still cannot relieve all suffering (Magnusson 2002; Pool 2000; Admiraal 1991; Cassell 1991).
Arguments from justice and the demand to be treated fairly
It is argued that everybody is entitled to be treated fairly and to share equally the benefits and burdens of life. To deny patients the option of being spared intolerable and intractable suffering is to treat them unfairly, and to make them carry a burden which others do not have to carry. Furthermore, to deny patients the right to die (i.e. in a manner and time of their choosing) is to impose unfairly on them the values of others. Only patients, or those intimately involved with them (e.g. family and friends), can judge what is in their own best interests. For others to deny patients the right to choose death is therefore to violate unfairly these patients’ autonomy, dignity and entitlement to be spared the harms that will flow from suffering intolerable and intractable pain. Where euthanasia is the only thing that can end patients’ intolerable and intractable pain and/or suffering, it stands as a morally just alternative.
Arguments from altruism and the ‘duty to die’
It is argued that in certain circumstances (such as in the case of old age, chronic illness or when medical treatment is futile) it may be a person’s duty to volunteer for euthanasia (Hardwig 2007; Kilner 1990; Beloff 1992; Schwartz 1993) and that it might also be a violation of a person’s right to freedom of conscience to interfere with the exercise of this duty (Lewis 2001: 60–2). Beloff (1992: 53), for example, apparently finds it quite plausible that:
the mere thought of becoming a burden to others, not to mention a drain upon society, would suffice to make [some] choose voluntary euthanasia as the only honourable course of action still open to them.
In situations where a person’s primary caregivers are burdened to the point where they cannot live their lives fully and are themselves beginning to suffer as a result of their burden of care, euthanasia, argues Beloff, is not only permissible, but required. Beloff (1992: 54) explains that this is because:
If there is a duty to die it is one that arises from our basic human predicament, the fact that we are dependent on others, and it is a duty we owe to those we cherish.
Hardwig (2007) holds a similar position, contending that sometimes ending one’s own life is ‘simply the only loving thing to do’. He writes (pp 94–5):
I may well one day have a duty to die, a duty most likely to arise out of my connections with my family and loved ones. Sometimes preserving my life can only devastate the lives of those who care for me. I do not believe I am idiosyncratic, morbid or morally perverse in believing this. I am trying to take steps to prepare myself mentally and spiritually to make sure that I will be able to take my life if I should one day have such a duty … Tragically, sometimes the best thing you can do for your loved ones is to remove yourself from their lives. And the only way you can do that may be to remove yourself from existence.
In regard to the assumed right to freedom of conscience, it might be argued that ‘the decision whether or not to commit [assisted] suicide is essentially a matter of conscience’ — the terms of which can be formulated on either religious or secular terms — which must be respected (Lewis 2001: 61).
Arguments from climate change
It is argued that climate change is poised to have a significant, far-reaching and possibly devastating impact on human health and psychological wellbeing, and that in instances where the impact is likely to be extreme people might want to — and indeed have the right to — ‘opt out’. The usual arguments from individual autonomy, dignity, the reduction of suffering, justice, and even a duty to die (as considered in the bioethics literature, too numerous to mention here), all support such a stance.
The prospect of people seeking euthanasia as an ‘exit strategy’ to escape a world severely disrupted by desperate food and water shortages, a crumbling infrastructure, and a soul-destroying loss of amenities has been given graphic expression in the 1973 classic (now cult) science fiction movie Soylent Green (directed by Richard Fleischer) (Wikipedia 2007a). Loosely based on Harry Harrison’s 1966 science fiction novel Make Room! Make Room! (available as a Penguin paperback re-issue), the film is set in the year 2022, and depicts a ‘Malthusian catastrophe that occurs because humanity has failed to pursue sustainable development and has not halted uncontrolled population growth’ (Wikipedia 2007b). At a key point in the film, the character Sol Roth (played by Edward G Robinson) opts for euthanasia after he becomes dispirited by a lack of books (because of a lack of paper, ‘real books’ were out of print) and the hideous lack of electricity, water, food and other amenities once taken for granted in everyday life. (Sol, a former college professor of literature, dies in a room adorned by motion pictures of the beautiful Earth as it once was, and which are shown only to those being euthanised [Wikipedia 2007a, 2007b].)
Soylent Green, although science fiction, contains some salutary lessons. When extreme weather events (including periods of high temperatures, droughts, torrential rains, and flooding) affect local populations, they are generally able to adapt ‘to the local prevailing climate via physiological, behavioural, and cultural and technological responses’ (McMichael et al 2006: 860). Scientists are warning, however, that extreme weather events (as well as other natural disasters such as earthquakes, tsunamis and fires) often ‘stress populations beyond those adaptation limits’, resulting in serious health risks and related poor health outcomes (McMichael et al 2006: 860; see also Haines & Patz 2004). Notable among the adverse health consequences that people can experience (and are already experiencing) are thermal stress (which may also precipitate or exacerbate heart attack, stroke and chronic respiratory disease), food poisoning, vector-borne infections and other infectious diseases, increased allergies, malnutrition, injuries, mental health disorders, and deaths (McMichael et al 2006; Haines & Patz 2004). Scientists further warn that, due to the social, demographic, economic and political disruptions it causes, climate change has other indirect or ‘knock on’ health effects as well. That is, because of the significant risks that climate change poses to infrastructure, amenities, regional food yields, water supplies, and so on, it can further disrupt individual and population health (McMichael et al 2006: 865, 866).
In a feature on global warming, National Geographic has highlighted that ‘things that normally happen in geologic time are happening during the span of a human life time’ (Appenzeller & Dimick 2004: 8–9). Given this, and the scientific warnings outlined above, it is understandable that people might reach a point where they would prefer to choose a peaceable death than to go on living a life hopelessly stranded by the impact of irreversible climate change.
C ounter-arguments to views supporting euthanasia
Not surprisingly, those who are against euthanasia are not moved by these kinds of arguments. The anti-euthanasia response typically entails three main approaches: (1) to assert a number of counter-claims and counter-arguments against the views put forward in support of euthanasia; (2) to assert a number of distinctive arguments against euthanasia; and (3) to reject altogether the notion of passive euthanasia (killing by omission) on the grounds that there is a morally significant difference between directly killing a person and merely letting a person die ‘naturally’ (referred to in the bioethics literature as the ‘killing/letting die distinction’).
Autonomy and the right to choose death
While the moral principle of autonomy is well established in Western moral thinking, it nevertheless has limits. Whether ‘autonomy’ was ever meant to stretch so far as to impose a moral duty on a doctor or a nurse to comply with a patient’s request for euthanasia — to intentionally and actively assist that patient to die — is an open question. If complying with a patient’s request for euthanasia has the foreseeable consequence of harming or affecting prejudicially the significant moral interests of others (e.g. the doctor[s] or nurse[s] receiving the request, or the patient’s family and friends), there is considerable scope for arguing that the doctor(s) and nurse(s) in question have no duty to perform euthanasia, no matter how autonomous the patient’s request for it. Further, given the complex nature of the morality of euthanasia, it is rather simplistic to hold that euthanasia can be justified on the grounds of patient autonomy alone without consideration being given to other important moral considerations which might also have a significant bearing on a patient’s choosing euthanasia/assisted suicide, and on a doctor’s, a nurse’s, a family member’s or a friend’s providing it.
Appeals to autonomy to justify euthanasia and assisted suicide are, however, problematic on another account. Paradoxically, acts of euthanasia/assisted suicide carried out in response to a patient’s autonomous request, destroy the very basis of their justification. According to Safranek (1998), while autonomy is necessary for the existence of a moral act, it is not sufficient to justify an act. As he explains (p 34):
The justification of the act will hinge on the end to which autonomy is employed: if for a noble end, then it is upheld; if depraved, then it is proscribed. It is not autonomy per se that vindicates an autonomy claim but the good that autonomy is instrumental in achieving. Therefore an individual cannot invoke autonomy to justify an ethical or legal claim to acts such as assisted suicide; rather he [or she] must vindicate the underlying value that the autonomous act endeavours to attain.
Since autonomous requests for euthanasia and assisted suicide are socially threatening (they threaten human survival), it is appropriate that the autonomy of individuals requesting such threatening acts (euthanasia/assisted suicide) be circumscribed — at least until such time it is clarified and agreed just what kinds of ‘good’ autonomy should be invoked to achieve (Safranek 1998: 34).
(It is important to note here that autonomy discourse is extremely powerful, making challenges to it difficult. So successful has been the promotion of autonomy, and the assumed sovereign rights of individuals to exercise self-determining choices, that the imperatives of these things — especially in the case of euthanasia/assisted suicide — have come to seem ‘so self-evident to all “right thinking people” that to question them seems almost perverse’ [Moody 1992: 50]. Those who do question them risk being publicly ridiculed and dismissed by opponents as ill-informed and ‘illogical’, or worse as being ‘insulting’ to vulnerable and oppressed groups [see, e.g. the reported comments in the Senate Legal and Constitutional Legislation Committee 1997: 71, 176].)
Dignity and the right to die with dignity
Dignity and dying with dignity does not necessarily entail choosing death over the artificial prolongation of life. The demand to respect and maintain a person’s dignity might equally entail respect for a person’s autonomous wish that ‘everything possible be done’ to prolong or sustain her or his life — and to sustain a sense of hope that is fundamental to living that life meaningfully, even though (and when) dying. Here, it is important to understand that the ethical controversies surrounding the care of dying patients are not just about management at a technological, medical or institutional level. As Campbell (1992: 255) points out, they should also be seen ‘as a sign of a deeper crisis of meaning in our culture’, and as an indication of how impoverished our society has become in ‘assessing the significance of suffering, dying and death as part of a whole human life’. Given this, as Campbell goes on to explain (p 255):
The emergence of the individual asserting inviolable rights to self-determination becomes intelligible in this void as a way to create meaning through a freely-chosen style of life and an authentic manner of death.
One way to respond to this crisis of meaning is to ‘provide compassionate presence to the sufferer’, not to ‘end the suffering by killing the sufferer’ (Campbell 1992: 269, 276). Another is to deny altogether the philosophical bases for a ‘right to die’ (see, e.g. Kass 1993).
Suffering and the demand to end it
Suffering is not just a medical problem; it is also an existential problem involving profound questions concerning the meaning and purpose of human life and destiny (Neimeyer 2001; Spelman 1997; Attig 1996; Campbell 1992; Starck & McGovern 1992; Amato 1990; Klemke 1981). To ‘end suffering by killing the sufferer’ is, to borrow from Campbell (1992: 276), to misunderstand ‘both suffering and ourselves in a way that threatens [infinitely] our moral integrity’.
Justice and the demand to be treated fairly
To deny patients the right to choose treatment — including the artificial prolongation of ‘hopeless life’ — is as unjust as to deny patients the right to choose death. Denying patients’ requests for ‘everything possible to be done’, where this conforms with their notions of dignity, meaning, value and quality of life, is to impose unfairly on them the values of others. As in the case for euthanasia, only patients (or those close to them) can judge what is in their best interests, and they must be permitted to make these judgments.
Altruism and the ‘duty to die’
In some circumstances, people may have a conscientious ‘duty to live’ in order to spare the pain of their grieving loved ones, who desire their ill loved one to live ‘as long as possible’. Being dependent on others is not necessarily being a burden on them (see, e.g. Kanitsaki 1994, 1993). Even if dependency does become burdensome — either for the dependent person or her or his carers — it is not clear how, if at all, this gives rise to a so-called ‘duty to die’. At best, it may only substantiate ‘our basic human predicament’ that:
the very experience of illness, and more fundamentally the process of aging that inevitably culminates in death, not only reveals our shared vulnerability and dependency, but also that we are all subject to some kind of ultimate powers beyond our control. Through our knowledge and technology we may aspire to a mastery of nature and the immortality of the gods, but we continually receive reminders of our dependency and finitude. From this it follows that any control we assert over our dying is already limited, and that dependency and dignity are not mutually exclusive.
(Campbell 1992: 270)
At worst, to embrace a ‘duty to die’ may be to embrace an all-pervasive sense of pessimism and hopelessness which would blind people to understanding that ‘the lives of even the terminally ill are precious and matter, right up to the last second of breath’ (Mirin, reported by Gibbs 1993: 53). And it may risk blinding people to the fundamental insight which has been articulated so well by the late French philosopher and feminist, Simone de Beauvoir (1987: 92), that, while all people must die, death is still an accident, and that, even if people know this, and consent to it, death remains ‘an unjustifiable violation’ (de Beauvoir 1987: 92). By this view, therefore, to embrace a duty to die emerges as an embracement of the unjustifiable violation of human life and all that it stands for. It also risks the perversion of morality — and of its ultimate aim, notably, how best to live the ‘good life’. Finally, if currency is given to the notion of people having a ‘duty to die’, this might have the undesirable effect of adding ‘to the distress and guilt [conscience] of those who wondered whether they were too great a burden on others’ (Muirden 1993: 14).
Climate change and the desire to have an ‘exit strategy’
There is no denying that climate change is serious and its adverse health effects potentially devastating. However, human culture is extremely adaptable and, as scientists are also advising, ‘many communities will be able to buffer themselves (at least temporarily) against some of the effects of climate change’ (McMichael et al 2006: 866). To ‘opt out’ of climate change by opting out of life, is to opt out of one’s civic responsibility to mitigate climate change and to adopt a proactive response to environmental justice that would be of benefit to all (Gostin 2007).
S pecific arguments against euthanasia
Specific arguments commonly raised against euthanasia (and the need to legalise it) include:
1. arguments from the sanctity-of-life doctrine
2. arguments from clinical uncertainty, misdiagnosis and possible recovery
3. arguments from the risk of abuse
5. arguments from discrimination
6. arguments from irrational or mistaken or imprudent choice
7. the ‘slippery slope’ argument.
Arguments from the sanctity-of-life doctrine
A popular argument raised against euthanasia draws heavily on the sanctity-of-life doctrine and contends that, since life is sacred and inviolable, nothing (not even intolerable and intractable suffering) can justify taking it. Sanctity-of-life arguments against euthanasia run something like this:
1. human life is sacred, and taking it is wrong
2. euthanasia is an instance of taking human life; therefore
3. euthanasia is wrong.
Whether human life is sacred, and whether taking it is always wrong is, however, a matter of philosophical controversy (Singer 1993; Kuhse 1987).
Arguments from clinical uncertainty, misdiagnosis and possible recovery
An argument often used against euthanasia is that which speaks to the risk of clinical uncertainty (ambiguity), misdiagnosis and the possibility of recovery. Doctors diagnosing life-threatening medical conditions are not infallible and can (and do) make mistakes (Craig 1994; Wilkes 1994). Furthermore, patients can sometimes recover spontaneously and unexpectedly from devastating and/or terminal illnesses — for reasons not always understood or accepted by medical scientists (for an insightful exploration of people’s capacity to heal and to recover unexpectedly from life-threatening conditions, see Gawler 2001; Dossey 1993, 1991; Chopra 1989). A poignant example of this can be found in the case of the noted best-selling author of The Women’s Room, Marilyn French. In 1992, French was diagnosed belatedly with metastasised oesophageal cancer. Her treating doctor at the time was extremely pessimistic about her prognosis, advising French that she had ‘terminal cancer, that there was no hope for cure or remission, and that [she] was not to think of that’ (French 1998: 34). Of this moment, French writes (p 34):
What was he saying? Hope, but not too much? Hope, but don’t expect a cure? What was I to hope for, then? He emphasised that mental attitude was crucial to anything they did. I spoke up, assuring him that I had strong powers of concentration and that I wanted to hope … But he wasn’t listening; he was talking over me. There was no hope for a cure, he said …
French, however, rejected the pessimism of her physician and simply ‘decided’ to survive. Accordingly she ‘twisted’ what medical information she had on oesophageal cancer to her purpose. For example, she seized on an article that stated ‘one in five people treated with extreme measures survive non-metastasised esophageal cancer for five years’ and decided those figures applied to her (despite her metastases). In French’s words, ‘I decided I had one chance out of five. I simply made it up’ (French 1998: 35). By the end of that day, she had obliterated the word ‘terminal’ from her memory; and within a couple of days, she had increased her odds of survival to be one in four and had ‘repressed any sense that [she] was deluding herself’ (pp 35–6). After going through what French describes as a ‘season in hell’ involving years of pain, dread and severe illness, she reached ‘a plateau of serenity’ (p 237). At the time of writing an autobiographical account of her experience of survival (published in 1998), French stated that, although suffering from a number of symptoms related to the damage caused to her bodily systems by the intense radiotherapy and chemotherapy treatment she received, she was feeling ‘relatively well’ and secure in the knowledge that the aches and pains she felt were not an indication of cancer (which had been cured).
There is also the possibility that new cures might be found for certain life-threatening conditions. For example, stem cell research (Keirstead 2001; Keirstead et al 2005; Lim & Tow 2007) and nanotechnology regenerative medicine research (Stupp 2005) are heralding a new era of medicine, together with renewed hope for the remedial treatment (including permanent cures) of such conditions as spinal cord injuries, diabetes, Parkinson’s disease and Alzheimer’s disease. (For a futuristic view of curative possibilities in medicine, see also ‘The Body’ [part 1] of the Discovery Channel’s three-part science documentary 2057, details at http://dsc.discovery.com/convergence/2057/about/about.html.) If a cure for serious spinal injuries or Alzheimer’s disease were found, people living with these conditions might, for example, not request assistance to die as they are now doing.
Finally, an important example of how a misdiagnosis can misinform the choice of euthanasia as a ‘treatment option’ can be found in the much-publicised Australian case of Nancy Crick. Mrs Crick, a 69-year-old grandmother, died in a blaze of media publicity after having ‘one last smoke, a sip of Baileys Irish Cream liqueur and a drug overdose’ (Davies 2002; Griffith 2002: 4; Hudson 2002: 1). Her death (witnessed by 21 relatives who were at her bedside) followed a campaign by pro-euthanasia supporters ‘to allow Mrs Crick, who had suffered bowel cancer, the right to die at a time of her own choosing’ (Franklin et al 2002: 1; see also Hudson 2002). The case took an unexpected turn when a forensic pathology report following autopsy revealed no evidence of bowel cancer (Franklin et al 2002). Dr Nitschke, a euthanasia campaigner who supported Mrs Crick in her quest for assistance to die, was reported as ‘not being surprised’ by the report stating ‘The only definite way cancer could have been established was through surgery and she flatly refused to have it’ (Franklin et al 2002: 2). He later admitted being present when Mrs Crick’s doctors had informed her 2 months before her assisted suicide that she probably did not have cancer (Jackson 2002). Nitschke is reported to have further admitted that ‘Now I think we should have perhaps stressed it [the uncertain diagnosis] more … it was a mistake in emphasis’ [emphasis added] (Jackson 2002: 2). Mrs Crick’s son, meanwhile, was reported to have said that he would be ‘massively shocked if the tests showed there was no cancer’ (Franklin et al 2002: 2). Other commentators were quick to point out that whether Mrs Crick had cancer was irrelevant, since there were no arguments as to why she should not have had the assistance she wanted, that is ‘to end her life with others present’ (Syme 2002; Komersaroff 2002).
What is of concern about the euthanasia option (and what the above cases highlight) is that once euthanasia is performed it cannot be reversed. Once done, it is done. The risk of error is unacceptable, and overrides any other considerations which might favour euthanasia in a particular case.
Arguments from the risk of abuse
The possibility of euthanasia being abused is an argument frequently raised against euthanasia. For example, Dr Nell Muirden, of the Peter MacCallum Cancer Institute in Melbourne, has emphasised the danger of euthanasia being abused by unscrupulous relatives (Muirden 1993; Athersmith 1986). Others, however, are more concerned about legislation giving one group (notably doctors) the power to terminate life. Such power could be particularly problematic in contexts heavily influenced by coercive (negative) social and political processes. In the US, for example, Margaret Pabst Battin, one of the foremost experts on end-of-life issues, warns (1991: 399):
This [the US] is a country where 1) sustained contact with a personal physician is decreasing, 2) the risk of malpractice action is increasing, 3) much medical care is not insured, 4) many medical decisions are financial as well, 5) racism is on the rise, and 6) the public is naïve about direct contact with Nazism or similar totalitarian movements. Thus, the United States is in many respects an untrustworthy candidate for practicing active euthanasia.
For the anti-euthanasiasts, the risk of abuse is unacceptable and underscores the need to reject the moral permissibility (as well as the legalisation) of euthanasia.
Arguments from non-necessity
Some contend that it is simply ‘not necessary’ to legislate or to support euthanasia. The reason commonly offered (particularly by those working in palliative care) is that the medical, nursing and allied health professions have been very successful over the years in allowing patients to ‘die with dignity’ (Chiarella 2006; Mendelson 1997; Ashby & Stoffell 1991). Since patients are ‘dying well’ or are having ‘good deaths’ anyway, why take the matter any further?
Arguments from discrimination
It is sometimes suggested that euthanasia entails blatant discrimination, notably by treating some lives as less worthy than others. Margaret Tighe, President of Right to Life Australia, for example, repeatedly argues that euthanasia is detrimental to terminally ill, sick and incompetent people. She has long maintained that euthanasia ‘reinforces the concept that there are some lives not worthy to be lived’ (Harari 1987; Maslen 1986). Others worry that were euthanasia and its counterpart assisted suicide to be legitimated, ‘people with disabilities will be subtly coerced to accept death prematurely’ (Mayo & Gunderson 2002: 14; see also Snyder & Mitchell 2006).
By this view, just as any other act of discrimination is morally offensive, so too is euthanasia.
Arguments from irrational, mistaken or imprudent choice
It is sometimes argued that any person requesting euthanasia is not really exercising a rational or prudent choice, and that, for this reason, among others, an individual’s request for euthanasia should not be taken seriously. One of the staunchest supporters of this view is the Vatican. In its 1980 Declaration on euthanasia, it states (1980: 7):
The pleas of gravely ill people who sometimes ask for death are not to be understood as implying a true desire for euthanasia; in fact it is almost always a case of an anguished plea for help and love.
There is also the risk that a person’s lawful representative might ‘get it wrong’. Just as someone who is in unbearable and untreatable misery might make irrational or imprudent choices, so too might their advocates — who, even though well intended, might nevertheless be misguided in their beliefs and actions. For example, Professor Peter Singer, one of the world’s most controversial philosophers and foremost advocates of euthanasia, has long argued that it is morally justifiable and even morally desirable (on utilitarian grounds) to kill severely disabled newborns and other ‘non-persons’ (e.g. children, adults and older people who, because of being brain-injured or suffering from a severe organic brain disease, such as end-stage Alzheimer’s, are incapable of making rational and autonomous life choices) (Singer 1993; Kuhse & Singer 1985). In 1999, however, it was reported that Professor Singer’s beliefs about euthanasia and the grounds upon which euthanasia might be justified and/or morally required in certain cases, were seriously challenged by a personal tragedy, notably, that of his mother becoming a ‘non-person’ (by his own definition) on account of developing advanced Alzheimer’s disease (Churcher 1999). When asked whether his personal situation would cause him to abandon his beliefs, he is reported to have replied (Churcher 1999: 19):
I think this has made me see how the issues of someone with these kinds of problems are really very difficult. Perhaps it is more difficult than I thought before, because it is different when it’s your mother.
The question of whether a death request is necessarily the product of irrational or imprudent or mistaken choice, however, is likely to remain a matter of controversy.
‘Slippery slope’ argument
Also popular in the anti-euthanasia debate, as it is in the anti-abortion debate, is the ‘slippery slope’ contention (Lewis 2007; Materstvedt 2003). It will be recalled that the slippery slope argument holds that we risk a decline in our moral standards once we permit the taking of human life. For example, if we permit abortion today, we will permit infanticide the next day, and euthanasia the next. In the case of euthanasia, a slippery slope argument might run as follows: once we allow euthanasia for consenting persons, we will permit euthanasia for unconsenting and non-consenting persons, such as infants, the intellectually impaired and the severely brain-injured. Once we compromise the standards for protecting human life, we compromise all other standards pertaining to human life and wellbeing. Euthanasia, then, should never be justified.
An instructive example of the risk of ‘slippery slope’ action in the context of euthanasia being practised can be found in the 1991 Dutch case involving a psychiatrist who medically assisted the suicide of a female patient who was suffering emotionally but who was otherwise physically healthy; that is, she had no somatic illness (Klotzko 1995; Ogilvie & Potts 1994). Although deemed by her psychiatrist not to be suffering from a psychiatric illness, the patient was nevertheless regarded as being clinically depressed. The social history of this woman is as follows and worth quoting at length:
She was a 50-year-old social worker. She was also a painter in her spare time. She was divorced. She had been physically abused by her former husband for many years. She had two sons. One son, Peter, died by suicide in 1986, at the age of 20. She then underwent psychiatric treatment for a marriage crisis following his suicide. At the time, she strongly wished to commit suicide, but decided that her second son, Robbie, age 15, needed her as a mother.
Her son, Robbie, died of cancer in 1991, at the age of 20. Before his death, she decided that she did not want to continue living after he died. She attempted suicide, but did not succeed. On July 13, 1991, she wrote to a social worker at the academic hospital where her second son died of cancer; she asked for a contact and for pills, so that she could kill herself. She had bought a cemetery plot for her sons, her former husband, and herself; her only wish was to die and lie between the two graves of her sons.
(Klotzko 1995: 240–1)
Subsequently, the patient wrote to Dr Boudewijn Chabot, a psychiatrist, requesting assistance to die. On 28 September 1991, Dr Boudewijn Chabot, after assessing the patient, provided her with a lethal dose of medication and remained with her while she swallowed the medication and died (Klotzko 1995: 239). He subsequently reported the death to the relevant authorities following which he was prosecuted by the Supreme Court of the Netherlands. On 21 June 1994, in what has been described as a ‘historic ruling’, the Supreme Court of the Netherlands found Dr Chabot guilty, but declined to punish him. Significantly, in reaching its verdict, the court rejected the contention that ‘help in assistance with suicide to a patient where there is no physical suffering and who is not dying can never be justified’ (Ogilvie & Potts 1994: 492). To the contrary. As Ogilvie and Potts report (p 492), the court:
explicitly accepted that euthanasia and assisted suicide might be justified for a patient with severe psychic suffering due to a depressive illness and in the absence of a physical disorder or terminal condition.
Significantly, the court found that Chabot’s guilt lay not in his providing a medically assisted death to his patient, but in his failure to obtain a second psychiatric opinion on the woman, and his failure to secure independent expert evidence that an ‘emergency situation existed’ — regarded as providing ‘the normal mitigating defence in such cases’ (Ogilvie & Potts 1994: 492).
Responses to the Chabot case have been mixed. Some have cited the case to underpin their sympathy for the view that (Ogilvie & Potts 1994: 493):
in severe and persistent depressive illness, when all appropriate physical treatments, including polypharmacy, electroconvulsive therapy, and psychosurgery, have apparently been exhausted, voluntary euthanasia may sometimes seem to be as justifiable an option as it does in intractable physical illness.
Others, however, take the Chabot case as underscoring the fears of those advancing the slippery slope argument. As Ogilvie and Potts (1994: 493) point out, the Chabot case of ‘psychiatric euthanasia’ has demonstrated that the ‘slippery slope’ exists. They conclude:
However well any legislation is hedged about with guidelines and protections against abuse, the slippery slope predicts an inevitable extension of those practices to other, more vulnerable, groups, such as those who are demented, mentally ill, chronically disabled, frail, dependent, and elderly — and perhaps even simply unhappy.
A further example of the slippery slope leading to an ‘inevitable extension’ of euthanatic practices can be found in the Dutch legislative reforms, referred to in the opening paragraphs of this chapter. The new legislation ‘now permits persons aged between 16 years or older to make an advance directive requesting euthanasia if they later become incompetent’ (Magnusson 2002: 65). Children aged 16 to 17 years are also authorised to request assistance to die, provided their parents are ‘ involved in the decision process’ [emphasis added]; in the case of children 12 to 15 years, however, parental approval is required before a request for euthanasia can be honoured (Magnusson 2002: 66).
A more recent example of ‘a slide down the slippery slope’, however, can be found in a 2006 decision by the Swiss Federal Supreme Court involving the case of an unnamed 53-year-old man with manic depression who had attempted suicide on two occasions. Assisted suicide has been legal in Switzerland since 1918 and, on account of being the only jurisdiction that does not require the involvement of a physician in the process, Switzerland is regarded as having the most liberal assisted-suicide laws in the world (Appel 2007). Up until the 2006 case, however, there had been a stringent taboo against assisted suicide in psychiatric patients or those with mental illness.
The case came before the court after physicians refused to prescribe the man a lethal dose of drugs to enable him to take his own life. In response to this situation, the man claimed that his right to self-determination under Article 8 of the European Convention had been violated and, with the assistance of Dignitas (a Zurich-based advocacy group), filed a suit in the Swiss Federal Supreme Court to have his right upheld (Appel 2007). His action was successful, with the Swiss High Court responding ‘with a sweeping opinion upholding the right of those suffering from “incurable, permanent, severe psychological disorders” to terminate their own lives’ (p 21). The court reasoned that, in contradistinction to people who have a treatable psychological disturbance and who are ‘temporarily impaired’, individuals with ‘severe, long-term mental illness who have made “rational”, and “well-considered” decisions to end their lives to avoid further suffering’ and who ‘repeatedly express a wish to end their lives under such circumstances’, should be permitted to do so (p 21). The ruling in this case is deemed to have significantly undermined the longstanding taboo against extending assisted suicide rights to ‘psychiatric patients and others with mental illness’, and many worry that this decision will seriously undermine the moral imperatives of contemporary psychiatry to prevent suicide, not to enable it (p 21).
The arguments for and against euthanasia considered here are not the only arguments raised in bioethics literature, but they are nevertheless common, and nurses need to become familiar with them. It should be pointed out that none of these arguments is uncontroversial, and that much more remains to be said about them than there is space here to do. Nevertheless, the discussion so far provides a starting point from which nurses can begin to address questions relating to the moral permissibility of euthanasia and assisted suicide.
T he killing/letting die distinction
Another response to the euthanasia debate is to argue that there is a morally significant difference between ‘killing’ and merely ‘letting die’. Opponents of euthanasia claim that so-called passive euthanasia is merely ‘letting die’; it is not euthanasia at all, and is therefore morally permissible. Let us explore this view further.
It is sometimes suggested that where medical treatment is relatively ‘expensive, unusual, difficult, painful or dangerous’ (sometimes referred to as ‘extraordinary’ treatment), no moral obligation exists to use it in order to prolong a person’s life (Beauchamp 1997; Gert et al 1997; Singer 1993; Vatican 1980: 10–11; Glover 1977: 195–6). Furthermore, where a given life-prolonging treatment is unduly ‘burdensome’ to the patient, or even costly, it may, in conscience, be withdrawn (Vatican 1980: 10–11; see also Repenshek & Slosar 2004; Shannon & Walter 2004). Even though the withdrawal of life-restoring or life-prolonging therapy may causally result in a patient’s death, this need not be regarded as an intentional termination of a life, and therefore an act of passive euthanasia, but rather as merely ‘letting nature take its course’. To put this another way, it is merely ‘letting die’, not direct and intentional killing. Withholding or withdrawing burdensome life-saving or life-prolonging treatment is therefore not, strictly speaking, euthanasia.
Bonnie Steinbock (1983) has argued classically that withdrawing or withholding burdensome life-prolonging treatment should not be viewed as the intentional termination of life, but as ‘the avoidance of painful and pointless treatment’ (p 293) — a position also upheld in law (Forrester & Griffiths 2005). Where decisions are made to withdraw treatments, these are really decisions about ‘the most appropriate treatment for a given patient’, not about killing that patient. She further contends that if a case of ceasing treatment is to hold as a case of euthanasia, it must first be shown that a particular treatment has been withdrawn with the intention of causing death. Where this cannot be shown, a claim of killing simply does not hold.
There are cases in which a doctor is simply ‘not at liberty’, argues Steinbock (1983), to continue treatment — such as where a competent patient has explicitly refused a recommended life-saving therapy. In such cases it seems odd to hold the doctor culpable for failing to provide treatment or for causing the patient’s death. Similarly, in cases involving hopelessly ill patients, where ‘nothing more can be done’, it seems implausible to hold that the discontinuation of a given treatment directly caused a patient’s ultimate death (Steinbock 1983: 294). Here it is disease that has provided the causal link to a patient’s death, not some act or omission on the part of a doctor or a nurse (see also Forrester & Griffiths 2005).
The ultimate conclusion of Steinbock’s argument is that the discontinuation of life-prolonging treatment cannot be considered the intentional killing of another — that is, an act of euthanasia. At best, it is merely ‘allowing nature to take its course’ or allowing the ‘natural flow of events to continue’.
The case for ‘letting die’ fails to consider, however, that deliberately not acting in life-threatening situations is itself a kind of act (see also Weinryb 1980). In this respect, a conscious decision to withdraw or withhold life-saving therapy still amounts to a ‘deliberate inducement of death’ (Trammell 1978). As Fletcher points out (1973: 675):
It is naive and superficial to suppose that because we don’t ‘do anything positively’ to hasten a patient’s death we have thereby avoided complicity in his [sic] death. Not doing anything is doing something; it is a decision to act every bit as much as deciding for any other deed.
By this view, it can be seen that withdrawing or withholding life-saving treatment still involves deliberate choice, just as positively administering treatment does, and as such still has ‘a place among events’ (Green 1980: 204). In this respect discontinuing or withholding burdensome life-saving treatment may hold as at least one way of intentional killing.
The view that withholding or withdrawing life-saving treatment is tantamount to intentional killing becomes even more compelling when considering the very nature of medical/health care contexts, which generally have the facilities to restore and/or prolong life. As Gruzalski (1981) points out, failing to treat in a medical setting is one way of killing precisely because in such settings there are the means to prolong life; where these means are not used, then a failure to treat can be differentiated from disease as a causal factor in a patient’s death. A good example of this is the highly publicised US case of Clarence Herbert (cited in Fry & Veatch 2006: 218–19). Mr Herbert, a 55-year-old security guard, suffered a respiratory arrest following an uneventful closure of an ileostomy. He was subsequently intubated and transferred to intensive care for treatment. There was, however, some controversy about whether Mr Herbert should be maintained on a ventilator. Nevertheless, the decision was made to discontinue his respiratory support. Although unconscious, Mr Herbert continued to breathe spontaneously and his vital signs stabilised. Despite this stabilisation, a second decision was made to withdraw all intravenous and nasogastric fluids, and to transfer Mr Herbert from the intensive care unit to a room in the hospital’s surgical unit. Six days after his respiratory arrest, Mr Herbert died. An autopsy listed ‘anoxia and dehydration as two of the causes of death’ (Fry & Veatch 2006: 219). Here then is one case in which a failure to treat (namely the withdrawal of respiratory support and hydration) contributed causally to a patient’s death; in this case a failure to treat was clearly distinguishable from mere disease.
The killing/letting die distinction is vulnerable to criticism on other grounds as well. Tooley (1980), for example, argues that there is no morally significant difference between intentionally killing and intentionally letting die, and that it is therefore just as wrong to ‘intentionally refrain from interfering with a causal process as it is to initiate it’ (p 58). One of the consequences of this view is that, if there is no significant distinction between intentionally killing and intentionally letting die, it is probably the case that there is also no real distinction between active and passive euthanasia, since, like killing and letting die, these share the same intention — that of bringing about or hastening a patient’s death. This, suggests Tooley, forces us to conclude that either euthanasia is somehow justified and therefore not morally wrong, or that we are morally confused or insincere in our thinking about it being wrong.
Arguing along similar lines, James Rachels (1975) contends that not only is there no distinction between killing and letting die, but that letting die ‘has no defence’ (p 496), particularly where the period of letting die entails a period of prolonged and intolerable suffering (see also Beauchamp 1997; Singer 1993). Cases involving the withdrawal or withholding of nutrition and hydration from severely disabled newborns and severe stroke patients who are not at the end stage of life are examples of this. Rachels further argues (p 495) that where letting die is allowed for so-called ‘humane reasons’, it amounts to much the same thing as killing; that is, the cessation of treatment amounts to intentionally terminating another’s life.
Consider, for example, the practice of withholding nourishing fluids from severely disabled newborns. As a result of this practice, the severely disabled newborn almost always dies (mostly as a result of dehydration and starvation). The decision to withhold fluids from a severely disabled infant is usually considered a ‘humane’ course of action, since if the infant were to live it could only look forward to a ‘burdensome’ life. In these kinds of cases, withholding fluids from a severely disabled newborn amounts to exactly the same thing as administering lethal injections to it, since both acts have the same intention (and outcome) — that is, of hastening the newborn’s death and thereby preventing it from living or having to live a ‘burdensome’ life.
If we accept these views, against the proponents of the killing/letting die distinction, we are also committed to accepting that there is no morally significant difference between withholding nourishment and fluids and administering a lethal injection. This is particularly so in cases where both have as their intention the hastening of a patient’s death, the ending of a patient’s suffering, and where both ultimately stand as a causal link to the patient’s death when it actually occurs. If we accept this, we are further committed to accepting that in the ultimate analysis there is no intrinsic difference between active and passive euthanasia.
I ntentional killing versus alleviating pain
At this point some comment needs to be made on the issue of narcotic administration to chronically and terminally ill patients. Is this, in some cases, tantamount to killing patients? I have spoken to many nurses over the years who feel that their actions in administering prescribed narcotic analgesia to some patients have been tantamount to ‘murder’. Accordingly, they have gone on to develop what some have termed ‘opioid phobia’, underscoring the need ‘to educate healthcare professionals about the need for adequate pain relief and to de-bunk some of the myths around pain management’ — especially in palliative care (Chiarella 2006: 34). The question that arises here is: Is the administration of narcotics in some cases the same as intentional killing? If so, is this always morally wrong?
It must be remembered, first, that many cases of medically prescribed narcotic administration are not cases of intentional killing, and in fact may prolong life. Second, it is also likely that some cases fall somewhere between prolonging life and intentional killing. Third, it is probably true that some cases of medically prescribed narcotic administration are cases of intentional killing (see earlier discussion in this chapter on nurse involvement in euthanasia). Let us refer to these three kinds of cases respectively as analgesia without death; analgesia with unintended death; and analgesia with intended death.
Analgesia without death
There are some pain states which can only be relieved by the administration of narcotic agents. An effective narcotic regime — even when entailing enormous doses — can, however, control pain without necessarily ‘doping’ or debilitating the patient. Indeed, many patients receiving large doses of narcotics remain alert, pain-free and as active as their disease will allow. Muirden (1993), for example, cites the case of a 55-year-old man who had cancer and who, at one stage of his illness, was receiving up to 3600 mgms of morphine by injection (the usual dose is about 10 mgms every four hours, a total of just 60 mgms a day). She writes: ‘He did not die of an overdose, and did not remain in a drowsy or drugged state’ (Muirden 1993: 18). In such cases the administration of narcotics is clearly nowhere near tantamount to intentional killing. In fact, it may be quite the reverse. As pain specialists have long pointed out, the correct prescription of narcotic agents (e.g. morphine) as well as the use of sedatives is more likely to prolong patients’ lives than shorten them, because patients are ‘able to rest, sleep, eat more and take a renewed interest in life’ (Twycross & Lack 1984: 183; see also Sykes & Thorns 2003; Mendelson 1997; Muirden 1993). In regard to this matter — particularly in the context of palliative care — Ashby and Stoffell (1991: 1323) conclude that there is ‘no evidence that the skilled and appropriate delivery of palliative measures (in particular the use of opioid analgesics and anxiolytic drugs) shorten life’ and that by operating within a ‘therapeutic ratio’ treating physicians are able to balance ‘symptom relief against a risk of death’ (see also Klepstad et al 2005; Sykes & Thorns 2003; Wells et al 2004).
Analgesia with unintended death
There are other pain states which can only be relieved by the administration of narcotic analgesia. However, unlike the previous type of case, these pain states require the administration of narcotics at a level which may compromise patients’ alertness and physical ability (including the ability to eat and drink), and may even render them semi-comatose. In these types of cases, death may be hastened, even if not directly intended. Although the precise incidence of this type of case occurring is not known (McStay 2003), they do occur frequently enough to be of concern to some nurse clinicians — particularly when associated with the withdrawal or withholding of life-sustaining nutrition and hydration (to be discussed later in the chapter under the subheading ‘Medical directives to withhold or withdraw nutrition and hydration’).
Analgesia with intended death
In another type of case, ill or debilitated patients do not have an organic pain state, or have only trivial pain states, but are nevertheless prescribed potentially lethal narcotic regimes. Pat Turton (1992, 1987), for example, cites the case of an elderly stroke patient who was prescribed what one nurse considered an ‘unnecessary and dangerous’ dose of morphine. The nurse’s views were shared by the hospital pharmacy. When the nurse questioned the drug order, however, she was asked by the prescribing doctor ‘Is this your first ward?’, the implication being that the nurse was naive. Turton comments that the drug was given by another nurse and the woman died within hours. Similar cases occur every day in residential care homes and in some general hospital wards. In other cases, analgesia is given to seriously ill patients who have neuropathogenic pain states which conventional medicine is unable to alleviate. The drug regime given is clearly intended to hasten death, although this intention may be ‘disguised’ in some way — for example, by stating a rationale to ‘alleviate pain’, even though it is known that the pain cannot be alleviated. It is difficult to avoid the impression that in all these cases the administration of a given narcotic regime is tantamount to intentional killing or the intentional shortening of life.
Given these three situations, the question remains: Is the administration of potentially lethal doses of narcotics always morally wrong?
The case of analgesia without death is morally uncontroversial. Here narcotic regimes enhance not only patients’ wellbeing but also patients’ lives. Since no moral standards are compromised, the administration of enormous doses of narcotics in this instance is morally permissible.
The case of analgesia with unintended death, however, is not so morally clear-cut. Although a patient may well be spared intolerable suffering by the administration of large and potentially lethal doses of narcotics, this cannot be achieved without compromising the patient’s sanctity of life. For some nurses, the conflict between the demand to alleviate a patient’s pain and the demand to respect and preserve a patient’s life is the most troublesome of all. When caught in such a conflict, these nurses generally find the preservation-of-life principle too compelling to override and, rightly or wrongly, opt for withholding the analgesia.
Like analgesia with unintended death, analgesia with intended death is morally controversial. It also needs to be remembered that administering analgesics for the intended purpose of bringing about death is illegal and would be viewed by the courts as tantamount to homicide. This is an issue which requires open and honest intellectual debate, as indeed the entire debate on euthanasia and assisted suicide makes plain (Chiarella 2006; Crock 1998; Magnusson 2002).
The doctrine of double effect
Catholic theologians have long recognised the dilemma posed by intolerable pain and the use of potentially lethal doses of narcotics as a means of suppressing pain. Interestingly, although the Vatican prohibits euthanasia, it nevertheless permits the use of narcotics as a means of alleviating pain — and, furthermore, permits dosages which might suppress a patient’s level of consciousness and even shorten a patient’s life (Vatican 1980: 9; Repenshek & Slosar 2004). There are, however, clearly defined conditions which must be met. First, there must be no other means of alleviating the patient’s pain; in other words, potentially lethal doses of narcotics must never be prescribed except as a last resort. Second, the intention of using narcotics must be to only alleviate pain, not to cause death.
The first condition, that of last resort, is consistent with the general principles governing effective and safe pain management and, as it stands, is relatively uncontroversial. The second condition, however, that of intentionality, takes its force from the controversial ‘doctrine of double effect’, and thus is vulnerable to the same criticisms as is the doctrine itself.
The doctrine of double effect was developed by Catholic theologians. It states, roughly, that it is always wrong to do a bad act for the sake of good consequences, but that it is sometimes permissible to do a good act even knowing it might have some bad consequences. To illustrate this doctrine, consider the case of a patient suffering intolerable and intractable pain. In this case, ending the patient’s life would also result in ending the patient’s intolerable and intractable pain. While ending the patient’s pain would be a ‘good thing’, ending the patient’s life would not. Indeed, given the sanctity-of-life doctrine, deliberately ending an innocent patient’s life would be a morally evil thing to do. Thus, we could say here, it would always be wrong to end an innocent patient’s life (a bad act) in order to alleviate that patient’s pain (a good consequence).
Given the ‘good’ of alleviating pain, however, we are morally permitted to give the patient analgesia — even though this might have the foreseeable and unfortunate consequence of shortening the patient’s life. This is permitted since, even though the act of narcotic administration is associated with the foreseen possibility of hastening death, ending the patient’s life is not the conscious intention behind the act. In short, the decision and action of giving the narcotics was not done with ‘murder in your heart’. To express the doctrine of double effect another way, we could say: it is always wrong to end patients’ lives for the sake of alleviating their pain, but it is sometimes permissible to give potentially lethal doses of narcotics to alleviate pain, even though this might result in the patient’s death — as long as the patient’s death is not the intended outcome.
Significantly, although primarily originating from Roman Catholic religious tradition, the doctrine of double effect has influenced secular legal reasoning in regard to end-of-life decision-making (McStay 2003: 53–6; Mendelson 1997: 112). One US legal commentator has even suggested that:
the double effect principle represents sound public policy to the extent that it allows physicians to provide adequate palliative care without engaging in clearly illegal conduct.
(McStay 2003: 54).
The doctrine of double effect has been the subject of much philosophical criticism, however, most notably on account of its over-reliance on what is called the foreseeability/intentionality distinction. This distinction holds roughly that foreseeing that a bad consequence will occur as a result of a given act is not the same thing as intending that bad consequence. For example, foreseeing that a patient will die as a result of being given large doses of narcotics is not the same thing as intending to end that patient’s life; therefore the person who administers the narcotic is not morally culpable.
Critics reject this, however, and argue that the distinction drawn here is misleading. They contend that foreseeing a bad consequence of an action is exactly the same as intending it, since the agent knows that a bad consequence is pending but deliberately refrains from preventing it. To some extent, this position is also upheld in legal law. As Kuhse (1984) points out, the law presumes: ‘everyone must be taken to intend that which is the natural consequence of his [sic] actions’ (p 26).
Given these criticisms, then, it seems that we cannot rely on the distinction between merely alleviating a patient’s pain and intentionally ending a patient’s life. Although it might perhaps be psychologically more tolerable to admit this distinction, it is not morally tolerable to do so. Where does this leave us?
The position is clear — nurses must all pursue a path of rigorous moral analysis of their actions. Acts involving narcotic prescription and administration must satisfy the ultimate standards not only of medicine, nursing and law, but also of ethics.
First and foremost, narcotic administration must accord with patients’ considered preferences. This means that every effort must be made to establish what patients’ preferences are, and to what extent patients are prepared to tolerate or not tolerate pain. Nurses must be open to the possibility, for example, of some patients preferring to suffer a certain degree of pain rather than compromise their mental alertness and physical ability. While a nurse might not agree with this kind of decision, it is nevertheless the patient’s prerogative to make it.
Second, pain management must be guided by moral as well as clinical and legal considerations (for a helpful outline of the agreed principles/standards of lawful narcotic administration see Mendelson 1997: 112).
Lastly, those involved in the administration of narcotics must be free conscientiously to refuse to administer drug regimes which they judge to be morally controversial or unacceptable.
I mplications for nurses of narcotic administration
Narcotic administration (particularly in the case of terminal sedation) will always remain a controversial issue for some nurses, as it does for other clinicians (McStay 2003). Nevertheless it is not insurmountable. In the case of legally prescribed narcotic pain management regimes, a sound knowledge of the principles and policies of pain management, proper pain assessment, and correct drug administration will help to reduce the likelihood of moral dilemmas occurring (see Chiarella 2006). In other cases, a clear articulation of relevant moral standards and values will help to reduce or at least adjudicate many of the moral problems associated with effective pain management and drug administration. Either way, the position nurses are morally obliged to take is clear: the patients are always the nurses’ primary concern. If nurses have good reason to believe that a patient’s safety, dignity, autonomy and wellbeing will be compromised by a given drug order or regime, then they must question it. This is not only a moral requirement, but also a legal requirement. It is far better to question a narcotic order and be wrong than not to question a narcotic order and be wrong — with the former, what is at stake may be only a little self-pride; with the latter, at stake may be a patient’s life.
‘N ursing care only’ directives
A common, although not widely acknowledged, euthanatic practice — and one that has significant implications for nurses — is that of doctors prescribing ‘nursing care only’ for patients deemed ‘medically hopeless’. In many instances (although, of course, not all), this medical prescription has become a euphemism for non-voluntary and involuntary passive euthanasia since what is in fact being ordered is not nursing care, but rather the withdrawal of both competent nursing care and life-sustaining (medical and nursing) care. To illustrate this point, consider the widely discussed Dr Leonard Arthur case (Kuhse 1984), and the Danville case (Robertson 1981). Although these two cases are now somewhat dated, the issues they raise remain current in contemporary nursing care contexts — particularly in regard to the common practice of prescribing terminal sedation in association with the withdrawal or withholding of nutrition and hydration (for a comprehensive account of the ‘terminal sedation’ issue, see McStay 2003).
The Dr Leonard Arthur case
On 1 July 1980, in a small English city, a Down’s syndrome infant named John Pearson died in the arms of a nurse. The case would have escaped public attention had it not been for a member of staff reporting the circumstances of the case to Life, an anti-abortion organisation. On the basis of the information obtained by Life, John Pearson’s attending physician, Dr Leonard Arthur, was charged with murder. The charge was based on the prosecution’s claims that:
1. Dr Arthur had ordered the administration of the drug DFl18 with the intention of bringing about the baby’s death;
2. the fact that Dr Arthur had ordered ‘nursing care only’ showed that he had intended the infant to die.
(Kuhse 1984: 22)
Dr Arthur’s ‘nursing care only’ order in this instance directed the feeding of water only to the infant, and the administration of the drug DFl18 ‘ at the discretion of the nurse in charge but not more than every four hours’ (Kuhse & Singer 1985: 2, [emphasis added]). Since John Pearson had no organic pain syndrome as such, it would seem that the DFl18 was prescribed for the purposes of sedating him and suppressing his hunger sensations.
However we look at this case, it is clear that what Dr Arthur ordered was not nursing care, or, if it was, it was highly negligent nursing care. For example, feeding only water to an infant who is demonstrably able to take and tolerate a full and nourishing fluid regime falls far short of reasonable and acceptable standards of nursing care, as does the administration of a narcotic to an infant who does not have a pathological pain state. It also falls far short of accepted medical standards of care and is highly questionable legally (McStay 2003; Craig 1996, 1994; Ashby & Stoffell 1995, 1991; Wilkes 1994). Let us explore this claim further.
Nurses are formally educated to assess individuals’ fundamental health needs, to diagnose needs deficits (i.e. health problems) and to plan nursing interventions aimed at helping people to meet their own health needs. Nurses are also formally educated to evaluate the outcomes of their nursing interventions and to modify their plans of care if an individual’s health needs and health goals have, for some reason, not been met. Among the ten or so basic health needs which nurses are taught to assess are nutrition (including hydration), comfort (including being pain-free) and safety (including being kept free of the harms that might be caused by the over-prescription or inappropriate prescription of certain drugs). The formal education given to nurses in this area provides the minimal legal standard of reasonable and acceptable nursing care. Any nurse who fails to assess and diagnose correctly a person’s health problems and plan nursing interventions to help meet the health needs of a patient is practising below a reasonable and acceptable standard of nursing care, and is thus practising negligently.
Even if hunger is conceded as a genuine ‘pain state’, this still does not justify the administration of large doses of narcotics or sedatives, nor does it rescue nurses administering these from culpability (McStay 2003). There are at least two reasons for this. First, it is not normal practice to administer large doses of narcotics or sedatives to alleviate hunger pain. If it were, patients hungry from, say, pre- and post-operative fasting would be routinely administered narcotics or sedatives as part of their care. As we know, this is not done. Nurses should be rightly suspicious of medical prescriptions directing the administration of potentially lethal doses of narcotics or sedatives to infants who are not dying from the natural progression of a life-threatening disease, who do not have a genuine pathological pain state, and who are suffering hunger only from not being fed adequately.
A second reason why narcotic or sedative administration is not justified in the case of hungry severely disabled newborns is that there is no clinical basis for preferring a narcotic agent or a sedative agent over a bottle of milk for alleviating these infants’ so-called ‘pain states’ and associated distress. As a general rule, narcotics are prescribed only for extreme pathological pain states or where other non-narcotic agents are known to be ineffective in alleviating a given type of pain. In less extreme pain states, the tendency is to prescribe non-narcotic agents (such as aspirin or paracetamol), or even to avoid prescribing analgesia altogether, with preference being given to other methods of pain management such as exercise, change of bodily position, massage, physiotherapy, transneuronal stimulation, the administration of antacids, and, in the case of babies and infants, simply nursing them on one’s lap and spending time with them. Since hunger is not generally regarded as an extreme pain state (in fact hunger is not even listed as a pain state in general analgesic guidelines and manuals), it is again highly suspect that narcotics should be chosen as a preferred ‘treatment’ option over the simple administration of a bottle of milk or other means of artificial nutrition and hydration which could be provided safely — even at the end stage of life (see, e.g. Steiner 1998). Similarly, sedatives are usually prescribed for children only as a last resort. Where children’s distress can be easily resolved by feeding them and/or nursing them on one’s lap, there seems little to justify the administration of potentially lethal doses of a given sedative or narcotic analgesic.
It is, I think, fairly obvious that ‘nursing care only’ orders, as given by doctors in the case of severely disabled newborns (as well as other cases), are prescriptions for deliberately ‘hastening death’. It is also clear that, by so ordering ‘nursing care only’, doctors are placing nurses in a position of legal negligence and possibly of even committing homicide. Obvious as these points are, however, they have been conveniently ignored by some courts. In the case of Dr Leonard Arthur, the suggestion that John Pearson had been killed by the nursing care only order was dismissed. Significantly, the defence council’s success was largely based on showing that ordering ‘nursing care only’ was proper medical practice (Kuhse & Singer 1985: 9). In this case, the judge ignored any thought that the attending nurses had acted negligently by giving ‘water only’ to a hungry infant otherwise capable of feeding, and had effectively committed homicide by giving potentially lethal doses of narcotics to an infant who did not have a genuine organic pain syndrome (see also Gunn & Smith 1985). Following his trial at Leicester in November 1981, Dr Arthur was acquitted of the criminal charges brought against him. His acquittal is reported to have sparked ‘rejoicing’ (Kuhse & Singer 1985: 10).
The Danville case
On 6 May 1981, Siamese twins were born at a hospital in Danville, Illinois. The babies were joined at the waist with three legs. Upon seeing the deformity, the attending anaesthetist passed the order: ‘Don’t resuscitate, let’s just cover the babies’ (Robertson 1981: 5; Horan 1982). The father of the twins, also a doctor, gestured support for the anaesthetist’s decision. It was later revealed that the decision to let the infants die had been made on little more than a visual impression of the infants’ condition. Robertson (1981) writes that in fact no assessment was made to check whether there was any brain damage, whether the twins could be separated, or what their prognosis was. No effort was made to explore either adoption or institutional alternatives for the babies. The decision was made in ignorance, and furthermore was made at the most stressful point in time — at delivery. Nevertheless, an order was written in the medical notes not to feed the babies, and they were taken to the newborn unit to die.
Nurses involved in caring for the twins became increasingly uncomfortable with the decision to withhold feeds from the babies. And it is claimed that at least one of the nurses ‘fed the babies several times’ (Robertson 1981: 5). The case received public attention after an anonymous caller reported it to the Illinois Department of Children and Family Services. Upon receiving the call the department immediately investigated the caller’s claim, and the babies were transferred to another hospital for assessment and care. Later, in an unprecedented step, criminal charges were filed against both the parents and the doctors for ‘conspiracy to commit murder and endangering the life and health of children’ (Robertson 1981: 5). In the legal case that followed, nurses described how the twins ‘cried in pain because they were hungry; how the cries dwindled down to whimpers as they were starved to death, how the skin started to wrinkle …’ (Robertson 1981: 6; see also Horan 1982).
As in the Dr Leonard Arthur case, nurses were once again placed in a legally and morally intolerable position on account of a ‘routine’ medical order to withhold nourishment. What made the medical directives in both cases seriously problematic was that they both required nurses to administer terminal sedation to, and to withhold feeds from, babies who were otherwise able to tolerate ‘normal’ feeding; who were not in a terminal phase of an illness; and who, with appropriate care and treatment, had a good prospect of recovery and living. Even if the babies were in a terminal phase of illness, the medical directives were still morally and legally wrong. Consider the following.
Medical directives to withhold or withdraw nutrition and hydration
People at the end stage of their illness, because of being in pain or severe distress and/or being sedated, may invariably reach a point where they cannot take food and fluids ‘naturally’ — that is, voluntarily by mouth, with or without assistance, in order to satisfy their hunger and thirst (Ashby & Mendelson 2003: 262). Here the question arises of: How should clinicians (doctors and nurses alike) respond to this situation?
The issue of withholding or withdrawing nutrition and hydration from patients at the end stage of life has been one of the most contentious issues in palliative care (see, in particular, the vitriolic debate between Craig 1994, 1996 and Ashby & Stoffell 1991, 1995). Basically there are two points of view:
1. hydration and nutrition should be administered (artificially, if necessary) to patients regardless of the terminal phase of their illness (Craig 1996, 1994)
2. there should be a gradual reduction and eventual cessation or non-initiation of treatment as the patient’s condition deteriorates (Ashby & Stoffell 1995, 1991).
Those who argue that hydration and nutrition should continue to be provided — even at the end stage of life — contend that if fluids are withheld or withdrawn from patients they will inevitably enter into a state of dehydration which, in turn, will result in ‘circulatory collapse, renal failure, anuria and death’ (Craig 1994: 140). In short, without hydration and nutrition, patients who are heavily sedated will die — whatever the underlying pathology (Craig 1994: 140). Furthermore, dehydration can lead to severe complications that may unacceptably alter the patient’s quality of life while they are dying; such complications can include: ‘increased asthenia, nausea, postural hypotension, fever with no underlying infectious process, increased risk of bed sores, and constipation’ as well as the ‘accumulation of opioid metabolites, grand-mal seizures, and hyperalgesia’ (Steiner 1998: 8, 12).
Another complication of dehydration is that of patients suffering from intolerable thirst and hunger during the terminal phase of their illness (see McCann et al 1994). On this, Craig argues (p 142):
It is widely assumed that a terminally ill patient is not troubled by hunger or thirst but this is difficult to substantiate as few people return from the grave to complain.
Finally, some worry that doctors might ‘get it wrong’ (i.e. make diagnostic errors) and accordingly patients might not only die ‘poorly’, but needlessly. On this point Craig contends (1994: 140):
Diagnostic errors can also occur. A reversible psychosis or confusional state can be mistaken for terminal delirium, aspiration pneumonia for tracheal obstruction, obstruction [of the bowel] due to faecal impaction for something more sinister, and so on. The only way to ensure that life will not be shortened is to maintain hydration during sedation in all cases whereby inability to eat and drink is a direct consequence of sedation, unless the relatives request no further intervention, or the patient has made his/her wishes known to this effect.
Not all, however, share these views and argue that a gradual reduction and eventual cessation or non-initiation of treatment as the patient’s condition deteriorates is not only clinically indicated, but also ethically mandated (Ashby & Stoffell 1995, 1991; see also Ashby & Mendelson 2003; McStay 2003). Proponents of this view argue that if and when a patient is in the terminal phase of illness:
no form of artificial hydration or alimentation is undertaken, all measures not required for comfort are withdrawn, and no treatment-related toxicity is acceptable unless the effects of this are less than the benefits achieved by the treatment. For example, artificial hydration may be required in the terminal phase to satisfy thirst or other symptoms attributable to lack of fluid intake.
(Ashby & Stoffell 1995: 136)
The view that hydration and nutrition should not be continued to be provided during the terminal phase of an illness rests on concerns that such treatment is more likely to add to the distress of the dying person, rather than provide relief. For example, research has shown that artificial hydration provided intravenously can lead to a range of associated medical conditions and complications including: vital organ failure from fluid overload (this can lead to such conditions as pulmonary and cerebral oedema and their associated complications); infection and bacteraemia from catheter and cannulation sites; arterial perforation, thrombosis, cardiac arrhythmias, cardiopulmonary arrest and pneumothorax during/following insertion of central venous lines; and pulmonary emboli (Steiner 1998: 8–9). Fluids administered long term (i.e. for periods longer than 2–3 weeks) via either nasogastric tubes of gastrostomy (e.g. percutaneous endoscopic gastrostomies or ‘PEG’ tubes) have also been associated with serious complications such as: diarrhoea due to osmotic load; aspiration pneumonia (due to tube displacement/the regurgitation and aspiration of gastric contents); metabolic abnormalities; mechanical difficulties (e.g. blocking of the tube, nasal irritation or erosion, tube displacement) (Steiner 1998: 11–12). Research in this area remains limited, however, and it is conceded by all parties that until a sound body of ‘gold standard’ research (including randomised controlled trials as well as rich qualitative studies) is available, and key questions answered about both the physiology and lived experiences of the administration of fluids to terminally ill (and sedated) patients, it is unlikely that the strongly polarised views on the matter will be resolved, or, at least, satisfactorily adjudicated. As Steiner (1998) notes, however, conducting such research may be difficult because of the ethical issues involved.
Disputes aside, there does appear to be a consensus in the field that a gradual reduction and eventual cessation of artificial hydration and alimentation (AHA) is appropriate during the terminal phase of care (Ashby & Mendelson 2003; McStay 2003; Steiner 1998; Parkash & Burge 1997; Ashby & Stoffell 1995, 1991; Craig 1994; Ahronheim & Gasner 1990; Belcher 1990; Sykes 1990; Lynn 1989). The critical issue here, however, is identifying and deciding correctly the point at which a patient is, on the balance of probabilities, in the ‘terminal mode phase in which death seems inevitable and imminent’ (Ashby & Stoffell 1991: 1323) — bearing in mind that ‘identifying the time of actual dying’ is easier in retrospect than prospect (Gillon 1994: 131).
Concurring with Ramsey (1976), Dyck (1984) and Grisez and Boyle (1979), Ashby and Stoffell (1995) contend that it is possible to distinguish between ‘those persons who are dying and those who are not’. Objective clinical standards enabling determinations to be made that ‘death is imminent’ include: demonstrated disease progression, vital organ failure, and the subjective (psychological, emotional and intuitive) responses of the patient and/or those close to them indicating that the ‘end is near’ (Ashby & Stoffell 1995, 1991). During this stage, the intake of food and fluid decreases ‘naturally’, although ‘both are always available (that is — they are never withdrawn)’ if the patient wants it. Ashby and Stoffell (1991) suggest that reassurance may also need to be provided to the family/support carers during this phase ‘that dying people usually want only enough food and drink to keep them comfortable — and frequent mouth care’ (Ashby & Stoffell 1991: 1323; for a helpful qualitative study on family perspectives on the issue of hydration in terminal care, see Parkash & Burge 1997).
Essential hydration (i.e. hydration necessary to control the symptoms of thirst) as well as analgesia can be provided safely and simply during the terminal phase by subcutaneous fluid infusion (or hypodermoclysis). This ‘rediscovered’ technique (first used in the 1940s and 1950s, but which was largely superseded by intravenous therapy technology that was developed at the time) is generally well tolerated, has a low incidence of adverse events, and last in situ longer (Steiner 1998: 9–11). Accordingly, it has gained considerable acceptance in palliative care over the past decade and is used widely (Ashby & Stoffell 1995; Bruera et al 1990; Fainsinger et al 1994; Sasson & Shvartzman 2001; Steiner 1998). To some extent, the use of hypodermoclysis has resolved some of the practical dilemmas and disputes about the provisions of food and fluids during the terminal phase of an illness; moral questions remain, however. Whether starting, stopping or not starting artificial hydration and alimentation, the criteria for deciding what to do ultimately rests on whether the dying person’s moral interests are being served by the decisions that are made. Here the critical question arises of: How best to decide what thosemoral interests are? (an issue that will be considered further in Chapter 12 on ‘End-of-life decision-making and the nursing profession’).
P osition statements on euthanasia/assisted suicide and the nursing profession
A pressing question currently facing the nursing profession concerns what, if any, formal position nurses ought to take on the euthanasia/assisted suicide issue? For many, this question remains an open one. For some, the failure by some nursing organisations to formulate a firm position, either way, on the euthanasia/assisted suicide question is untenable and paradoxical — paradoxical since even a ‘non-position’ is a position (Johnstone 1996a).
Significantly, there is no universally agreed nursing position on the ethics of euthanasia/assisted suicide; different nursing organisations in different countries hold quite distinct and sometimes opposing views on the matter, and on whether it is appropriate for nurses to assist with euthanatic procedures (Johnstone 1996b: 32–43). For example, whereas some nursing organisations (such as the Royal College of Nursing in the UK, and the American Nurses’ Association in the US) have stated positions firmly rejecting the role of the nurse in participating in or assisting with active voluntary euthanasia and/or assisted suicide, others (such as the National Nurses’ Association in the Netherlands) have stated positions supporting the role of the nurse in assisting with euthanasia/assisted suicide (Johnstone 1996b: 32–43). While there does seem to be some agreement among nursing organisations on the matter of patients’ rights to self-determination, and to die with dignity and peace (Johnstone 1996b: 38), this support has stopped short of being translated into a frank pro-euthanasia/assisted suicide position with the matter tending to be left to individual nurses to decide on the basis of conscience.
In several respects it is not surprising that there exists moral uncertainty and disagreement among members of the nursing profession about the ‘rightness’ and ‘wrongness’ of euthanasia/assisted suicide; about the kind of position the nursing profession should take, if at all; and, in the event of euthanasia/assisted suicide being decriminalised, about what kind of role nurses should play in the medically assisted deaths of patients. Many people hold differing views on these and related issues, and there is no reason why nurses should be any exception in this regard. Furthermore, it is important that this moral uncertainty and disagreement exists — a point that is not always understood. Nurses like other members of the community should not fear moral uncertainty. Appropriately placed it fosters what I shall call here ‘moral vigilance’ — a moral ‘watchfulness’ that can and does provide an important ‘check and balance’ against moral complacency. Neither should nurses fear moral disagreement or the diversity of opinion underpinning it (provided, of course, this does not spill over into violence, as has happened with the abortion debate where, it will be recalled, pro-life supporters have murdered pro-choice supporters in the name of upholding their ‘pro-life’ beliefs). As has long been recognised in philosophy, disagreement is the beginning of our thinking, not its end. Philosophical disagreement can help to stimulate our moral imagination and wisdom, and to sharpen and refine our moral thinking. In this respect, moral disagreement can, paradoxically, be creative and protective, not destructive; it can enable us to discover new solutions which might otherwise have alluded us — to see not just new things, but to engage in a new way of thinking about the things we have discovered. Moral uncertainty and disagreement, therefore, can both provide important beginning points for developing our moral thinking and finding sustainable and satisfying moral stances from which to view the world and guide our moral conduct. Consider the following case scenario.
A few years ago I was participating in a panel discussion on euthanasia and assisted suicide which had been scheduled during a 1-day seminar on the topic. During the panel discussion (in which a number of distinguished guests participated) I noticed a young woman (a nurse) crying silently in the audience. Concerned about this young woman’s obvious distress, I approached her during the morning tea break to ask if she wished to discuss with me what was troubling her. This she agreed to do. Upon hearing her story, I asked whether she would be willing to share her situation with the rest of the seminar participants once the proceedings recommenced after the morning tea break. This she also agreed to do. When the proceedings of the seminar recommenced, I had the opportunity to call on the young woman to share her feelings about the topic under discussion. She bravely faced her audience and related the following:
I am sitting here listening to you all. And I am so envious because you all seem to be so sure about where you stand on the [euthanasia] issue. You are either for or against it. But I do not have the benefit of such certainty. I simply do not know where I stand and this makes me feel very upset. You see, it is like this: I am a ‘good Catholic girl’, with a good Catholic education. My church tells me ‘euthanasia is wrong’ and that I must not support it. But then, I am also a nurse. I believe I am a good nurse and I believe in nursing. And my profession tells me I must support patients’ rights — I must be an advocate for my patients’ rights. And then there are my patients. Sometimes my patients want to die and ask for assistance to die. And I want to do what is right by them. And then there is me, the human being, torn between what my church tells me I should do, what my profession tells me I should do, and what my patients want me to do. I just feel so torn, because I really feel so uncertain about what is the right thing to do. I just don’t know. I just don’t know which side of the fence I should be on. And I feel that somehow maybe I am stupid or deficient because of this — especially when I listen to all of you here being so sure about the positions you are holding.
With this brave and frank admission came other admissions from other people in the audience; significantly, and contrary to superficial appearances, most of the people attending the seminar felt the way this nurse did, but had been unable to say so publicly. We then spent some time exploring the permissibility of feeling ‘uncertain’ about new and previously unexplored ethical issues, of taking the time necessary to consider other points of view and to explore possible answers to the difficult questions raised, and to ultimately reach a position on the issues identified that the person in question could ‘live with’.
Some time later the nurse in question contacted me. She had reasoned the issue through and had reached a position about which she felt confident at both a personal and professional level. What had helped her most in reaching this position was peer support, and the ‘permission’ her peers had given her to take the time she needed to ‘think through’ the issues at hand. She also particularly valued the opportunity the seminar had provided in regard to exposing her not just to the issues raised but to the many different points of view expressed in response to them. But most important of all, she valued being able to share her story, and in this sharing to ‘make visible’ a problem that she was soon able to discover was not hers alone.
Coming to terms with the complex questions raised by the euthanasia/assisted suicide issue requires a systematic response by both individual nurses and the broader nursing profession. Specifically, it requires nurses to gain knowledge and understanding of the profound ethical, legal, cultural, clinical and political dimensions of euthanasia/assisted suicide, and the influence these dimensions have on the profession and practice of nursing (Johnstone 1996a). Equally important, it requires peer support and understanding among nurses and a recognition that the euthanasia/assisted suicide question is not — and never has been — simple and clear-cut.
In concluding this section, there is much to suggest that in order for a position statement on euthanasia/assisted suicide to be meaningful to members of the nursing profession, it must minimally reflect that euthanasia and assisted suicide are controversial moral issues, that there exists a diversity of opinion on whether euthanasia and assisted suicide are morally justified, and that nurses are likely to encounter this diversity of opinion during the course of their work. Further, such a position statement must also reflect that there exists a diversity of opinion on whether nurses have a legitimate role to play in providing medically assisted deaths to patients and that all nurses have a responsibility to ensure that they are reliably informed about the ethical, legal, cultural, political and clinical dimensions and implications of euthanasia and assisted suicide as a ‘health care’ option.
C onclusion
Euthanasia and assisted suicide are issues that have obvious significance for members of the nursing profession. While nurses can choose to accept or reject the findings of public debate on the euthanasia/assisted suicide issue, they cannot ignore them since, to do so, would be to risk not just their own moral interests, but importantly the interests of patients for whose care they share responsibility.
The issues of euthanasia and assisted suicide have not been widely discussed in the nursing literature, and the need to do so is long overdue. If this neglect is not redressed, it will be to the peril of the nursing profession, as the experiences of nurses in the Northern Territory of Australia and the Netherlands (discussed in this chapter) remind us. It will be recalled, for instance, that in 1996, Northern Territory nurses had to confront the reality of being enabled by law to participate in euthanasia and assisted suicide before the broader nursing profession had reached a position on the matter and had determined what it regarded as ‘acceptable standards of nursing practice’ in relation to the actual practice of euthanasia/assisted suicide. In the Netherlands, meanwhile, nurses had to confront the reality that they could be successfully prosecuted for performing euthanasia even when such an action was in accordance with legally prescribed criteria. And in the aftermath of Hurricane Katrina in the US, nurses had to confront the reality of being poorly prepared when confronted by a natural disaster and their inability to safely evacuate patients in their care. Nurses are — and have always been — in a tenuous position in regard to their role in participating in end-of-life practices. It is timely that this tenuous position is addressed in the interests of reducing not just the vulnerability of nurses, but of the patients otherwise reliant on nurses for quality care at the end stages of their lives.
Case scenario
In 1996, in what is believed to be the first case of its kind in Australia, a nurse was charged with murder after he turned off the life support machine sustaining the life of a 37-year-old woman (and mother of three) who was suffering from a rare and crippling brain disease. Although there was some suggestion that the woman was ‘brain dead’, she had not been ‘formally declared dead’ (Donovan 1996: 2). It was also alleged in media reports that ‘the appropriate documents required to remove treatment from a comatose patient had not been signed at the time of the woman’s death’ (Walsh & Pirrie 1996: 1). Media reports also claimed that the nurse took the action he did on the grounds that he ‘believed that he was acting in the patient’s best interests’ (Walsh & Pirrie 1996: 2) and that he believed he had the permission of the woman’s husband (Das 1996: 7).
The case was reported to have focused ‘national attention on the care and treatment of incompetent and severely brain damaged patients’ and to have revived ‘the whole euthanasia question’; the case was also reported to have focused attention ‘on hospital guidelines and regulations on the care of brain-damaged patients’ (Walsh & Pirrie 1996: 2). Later media reports further suggested that the case had shown ‘that there was a “demarcation dispute” about who had the right to disconnect life support machines.’ (Das 1996: 7).
CRITICAL QUESTIONS
1. Were the nurse’s actions in this case tantamount to an act of euthanasia, assisted suicide, ‘mercy killing’ or homicide?
2. Accepting for arguments sake that the nurse’s actions were not homicidal (the nurse was in fact acquitted of the charges against him), were they morally justified? If so, on what grounds? If not, why not?
3. If euthanasia and assisted suicide were legalised, should provisions be included to legitimate the role of nurses to assist in patient deaths? If so, what role specifically should nurses have?
4. Should the nursing profession formally support the legalisation of euthanasia and assisted suicide and engage in political activism to achieve law reform in this area? Upon what basis do you rest your arguments in support of your views?