CHAPTER 10
Acromioclavicular Injuries
Definition
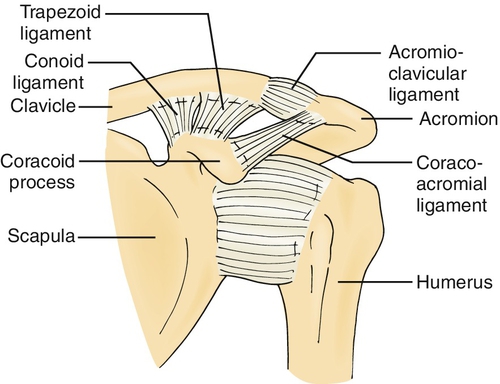
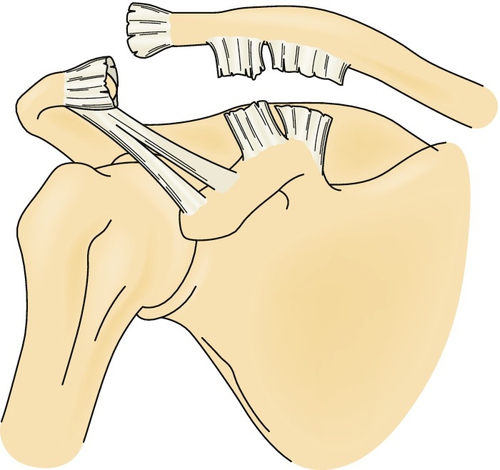
The acromioclavicular joint is a diarthrodial joint found between the lateral end of the clavicle and the medial side of the acromion [1]. The joint is surrounded by a fibrous capsule and stabilized by ligaments. The acromioclavicular ligaments cross the joint. Three ligaments begin at the coracoid process on the scapula and attach to the clavicle (trapezoid and conoid ligaments) or the acromion (coracoacromial ligament) (Fig. 10.1). This complex provides passive support and suspension of the scapula from the clavicle while allowing rotation of the clavicle to be transmitted to the scapula [1,2].
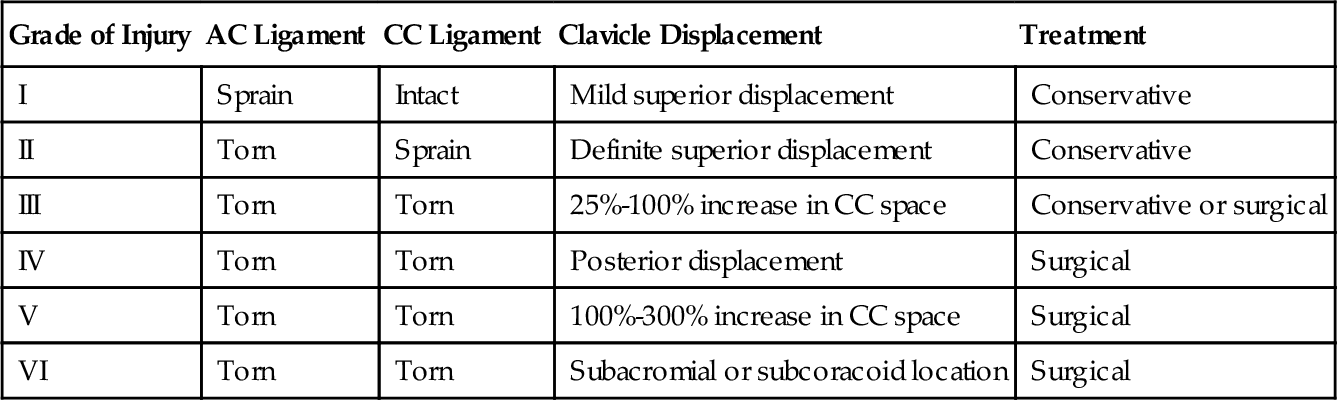
Injuries to the acromioclavicular complex are graded I to VI (Table 10.1). Injuries to the acromioclavicular joint were originally classified as grades 1, 2, and 3 by Tossy [3]. This classification was extended to include more complicated injuries, and grades 4, 5, and 6 were described. The extended grading system uses roman numerals [4].
The coracoacromial (lateral) ligament is not disrupted in injuries to the acromioclavicular joint. Therefore the fibrous connection persists between structures of the scapula emanating anteriorly and posteriorly [5]. In rare instances, there is an intra-articular fracture of the distal clavicle in addition to the ligamentous injuries [6].
There are few demographic data on differences of the disorder based on gender. Problems with the acromioclavicular joint can be associated with trauma and with overhead and throwing activities. Higher grade injuries are more likely to be due to trauma, such as auto accidents, falls, or sports injuries [7]. Concomitant injuries can vary on the basis of age; 86% of individuals older than 50 years have rotator cuff tears [8].
Most patients with grade I or grade II injuries respond to conservative measures and become asymptomatic within 3 weeks [9].
Symptoms
Patients often provide a history of trauma to the shoulder or in the vicinity of the acromioclavicular joint. Participants in contact or collision sports (e.g., football, downhill skiing) are particularly susceptible. Patients seek care because of pain in the anterior and superior aspect of the shoulder [2]. This radiates into the base of the neck and the trapezius or deltoid muscles or down the arm in a radicular pattern [2,5,10].
Patients may describe pain brought on by activities of daily living that bring the arm across the chest (e.g., reaching into a jacket pocket) or behind the back (e.g., tucking in a shirt). Pain can also occur with shoulder flexion (reaching overhead) or with adduction of the arm across the chest. Patients may not have pain at rest and may be able to complete many activities without discomfort.
Physical Examination
Appropriate examination for suspected acromioclavicular injuries includes an examination of the neck and shoulder joint and girdle to eliminate the possibility of a radiculopathy or referred pain. Patients should have normal neck and neurologic examination findings. The presence of neurologic or vascular injury suggests that a greater degree of trauma has been sustained [5].
On inspection, there may be a raised area at the acromioclavicular joint. This is caused by depression of the scapula relative to the clavicle or swelling of the joint itself. This area is commonly tender to touch. On active range of motion, the patient may complain of pain or wince near the extreme of shoulder flexion.
Shoulder range of motion is typically within normal limits. Supporting the arm at the elbow and gently directing the arm superiorly may decrease the pain and allow more complete assessment of the patient’s shoulder range of motion. The pain may become worse as the shoulder is further flexed, whether it is done actively or passively. This is in distinction to impingement syndromes, which often hurt at a particular point in the arc of motion but are painless as the motion proceeds. Pain is typically absent with static manual muscle testing of the rotator cuff. Rotator cuff injuries will be painful with activation of the muscles of the rotator cuff. These problems are best identified with the shoulder in a neutral position (i.e., elbow next to the body) because the rotator cuff muscles are in a lengthened position and are easily made symptomatic.
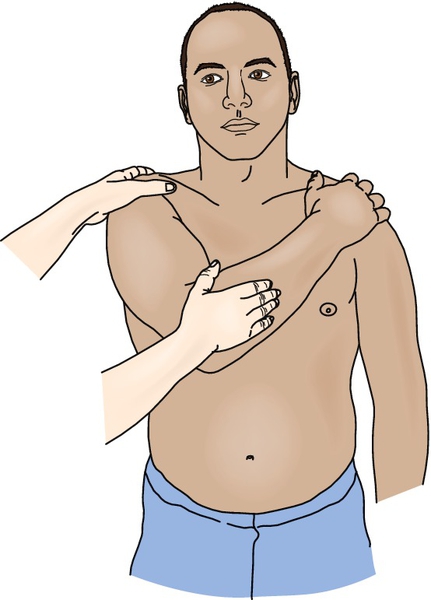
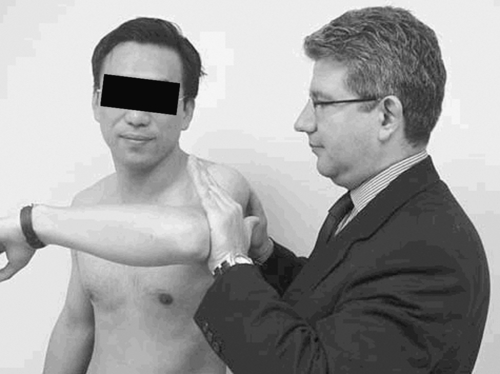
Special tests to identify acromioclavicular joint disease attempt to compress the joint. The most common test is the cross-body adduction test (Fig. 10.2). The shoulder is abducted to 90 degrees and the elbow is flexed to the same degree. The clinician then brings the arm across the patient’s body until the elbow approaches the midline (or the patient reports pain) [2].
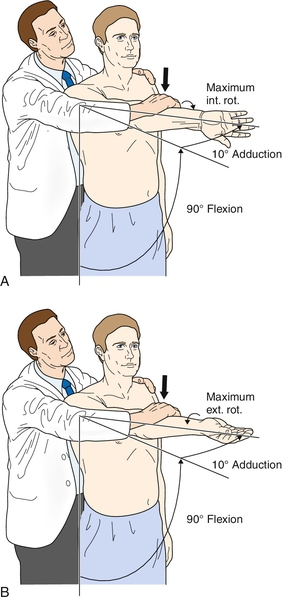
Other tests help differentiate between impingement syndrome and acromioclavicular joint pain. If the shoulder is passively flexed while it is internally rotated, the greater tuberosity can pinch (impinge) the supraspinatus tendon and subacromial bursa. The same test performed with the shoulder externally rotated will compress the acromioclavicular joint without impinging the subacromial space [11]. In the active compression test, the shoulder is flexed to 90 degrees and then adducted to 10 degrees (Fig. 10.3). The patient first maximally internally rotates the arm and then tries to flex the shoulder against the clinician’s resistance. This puts pressure on the acromioclavicular joint and may reproduce pain if disease is present. The test is repeated with the shoulder in full external rotation. This will put stress on the biceps tendon and its labral attachment while excluding the acromioclavicular joint [12].
In the acromioclavicular resisted extension test, the shoulder is abducted to 90 degrees and adducted across the body to 90 degrees (Fig. 10.4). The examiner resists active shoulder extension. A positive test result reproduces pain in the acromioclavicular joint. A combination of these tests will improve the diagnostic accuracy over isolated tests [13].
The Paxinos sign, along with bone scan, has a high degree of diagnostic accuracy in acromioclavicular joint disease [14]. The examiner stands behind the patient and, using the hand contralateral to the affected shoulder, stabilizes the clavicle and pushes the acromion into the clavicle with the thumb. The test response is considered positive if pain occurs or increases in the region of the acromioclavicular joint; the test response is considered negative if there is no change in the pain level (Fig. 10.5).

Functional Limitations
Reaching up, reaching across the body, and carrying heavy weights are limited because of pain. Patients may have no pain at rest and little or no pain with many activities. Patients may complain of difficulty with putting on a shirt, combing the hair, and carrying a briefcase or grocery bag. Most recreational activities, especially those that incorporate throwing, will be limited as well. Sleep may be affected because of pain, especially when rolling over on the affected side.
Diagnostic Studies
Because this is often a traumatic injury, radiographs are important in most cases and should be obtained to rule out fracture as well as to assess the severity of the injury (Fig. 10.6). Views should include an anteroposterior view, a lateral Y view, and an axillary view. It is important to let the radiologist know that injury to the acromioclavicular joint, not just the shoulder, is in question. Stress or weighted views are usually not helpful and cause undue pain without improving the accuracy of diagnosis [2,15]. Overpenetration of films may make the interpretation of the acromioclavicular joint and distal clavicle difficult [5].

A 15-degree cephalad anteroposterior view helps diagnose sprains by decreasing x-ray penetration and showing separation between the acromion and clavicle, whereas the 40-degree cephalic tilt anteroposterior view should be used for suspected fractures of the clavicle. If the fracture is medial to the coracoclavicular ligaments, both anterior and posterior 45-degree views should be obtained [5]. Typically, the decision to obtain these views is made by a radiologist.
Certainly, if there are concerns about a fracture or arthrosis and the x-ray images do not provide confirmation, further evaluation with a bone scan [2,5] or magnetic resonance imaging (MRI) may be indicated [16]. MRI evaluation of symptomatic acromioclavicular joints revealed that 80% had active bone edema in the distal clavicle or acromion or on both sides, but no asymptomatic patients had this finding [17]. MRI will detect the extent of acromioclavicular arthrosis more frequently than conventional radiology [18]. MRI does not appear to add any further information to the clinical assessment [19].
Ultrasonography is a reproducible method of evaluating the joint space and joint capsule, but the measurements may vary from those obtained by MRI [20]. The findings on ultrasound evaluation correlate well with the diagnosis obtained by clinical examination and radiography [21].
Treatment
Initial
Initial treatment depends on the degree of injury and the patient’s activity and goals.
Type I and type II injuries are exclusively treated nonoperatively, whereas type IV, type V, and type VI injuries require surgery. Treatment of type III injuries is controversial (see Table 10.1).
The initial phase of treatment for all injuries not going to surgery (i.e., type I, type II, and some type III) includes rest, ice, and possibly a sling or brace for 1 to 6 weeks (2 to 3 weeks average). Over-the-counter or prescription non-narcotic analgesics are usually sufficient. Nonsteroidal anti-inflammatory drugs can be used for pain and inflammation. Injections into the joint can also be done in the initial phase of treatment for immediate pain control and to help confirm the diagnosis. Injections have been done acutely with immediate return to activity in low-grade injuries.
Rest should be relative, that is, the patient should avoid aggravating activities but should not be immobilized if at all possible.
Ice massage can be done over the painful area for 5 to 10 minutes every 2 hours, as needed. An ice pack can be used for 20 minutes at a time and also can be repeated every 2 hours. The usual precautions for the use of cold modalities should be followed.
Type I and type II sprains can be treated with a sling to help support the arm and shoulder. This should be used symptomatically and discontinued for painless activities and when the patient’s pain is under control.
Type III injuries have been treated operatively and nonoperatively (Fig. 10.7). In the majority of published studies and reference texts, orthopedists favor nonoperative treatment as a rule, even in throwing athletes [5,15,22–24]. One study suggested greater long-term satisfaction in patients who had surgery but showed no difference in range of motion or strength [25]. Most patients have no long-term difficulty with nonoperative management. There are also reports of high complication rates with surgery [5,24]. Surgery may be considered in symptomatic individuals with type III injuries and in those who do not respond to conservative measures.
One approach for type III injuries is to treat conservatively with relative rest, support, modalities, medications for symptoms, and gradual return to activity during 6 to 12 weeks. If there is a significant limitation in function, including avocational or sport activities, or if the patient is not progressing as expected, further evaluation is warranted [5]. Unlike with musculotendinous injuries, delayed surgery does not lead to poorer outcomes.
Rehabilitation
Physical or occupational therapy can be ordered to assist with education of the patient, pain control, and, in later stages, gradual range of motion and strengthening exercises. Modalities to control pain can include, in addition to ice, ultrasound and phonophoresis with 10% lidocaine. Alternatively, interferential current can be used. As pain is controlled, motion can be obtained in a pain-free range. Codman and pendulum exercises can progress to active or active-assisted range of motion to restore shoulder flexion and abduction, both individually and in combination. In the initial phase of a rehabilitation program, it is reasonable to avoid painful positions or movements. These include extremes of flexion—even when they are done passively—and adduction across the chest. When the shoulder is pain free and has full range of motion, rehabilitation can progress to gradual strengthening and return to activity. A typical shoulder strengthening rehabilitation program can be used. Light dumbbell exercises with 1 to 5 pounds to strengthen the internal and external rotators or resistance bands can be used initially. This program can be advanced to isolate the shoulder abductors and to incorporate internal and external rotator strengthening at different degrees of shoulder abduction. Further progression depends on the patient’s goals and requires incorporation of the scapular stabilizers and training in coordinated movements.
Postoperative rehabilitation varies by the type of injury (type III–type VI), acute versus chronic repair, surgical technique employed, and surgeon. Typically, there is a period of immobilization or support with a sling (1-6 weeks). Passive, active-assisted, or active range of motion exercises may be allowed during this time. In some instances, daily activities will be allowed, but strengthening and heavy lifting are not.
Strengthening exercises may begin as soon as 2 weeks or as many as 3 months postoperatively, depending on the repair. Return to sports may take 8 weeks and be as long as 6 months. Given the variety of recommendations, good communication with the orthopedic surgeon is essential [7,26–28].
Procedures
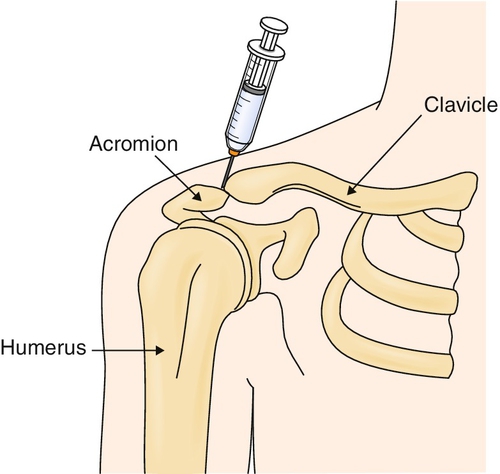
Patients with acromioclavicular joint pain due to type I or mild type II injuries can receive injections and return to play or work during the same day or competitive event with little risk of injury as long as they have full functional range of motion and symmetric strength. For diagnostic purposes, a local anesthetic injection may confirm the diagnosis of a type I sprain if the patient has complete pain relief immediately after the injection. Intra-articular injection of a combination of a local anesthetic and a corticosteroid may give immediate and longer acting relief. Injections into the joint can be done for higher grade injuries as well as to give quick symptomatic relief. However, this is not a substitute for relative rest in more seriously injured joints (type II and higher), and 1 week of avoiding provocative maneuvers after the injection is advised [2]. The blind or palpation approach to acromioclavicular joint injection is done with the patient sitting or supine with the shoulder propped under a pillow. The acromioclavicular joint is injected under sterile conditions with use of a 25-gauge, 11⁄2-inch disposable needle and a local anesthetic or anesthetic and corticosteroid combination (Fig. 10.8). Typically, a 1- to 3-mL aliquot of solution is injected (e.g., 1 mL of 1% lidocaine mixed with 1 mL of betamethasone). Keep in mind that the acromioclavicular joint is small and close to the surface.
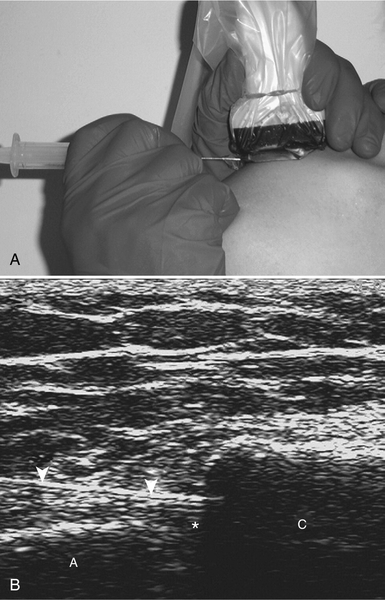
Ultrasound guidance of the acromioclavicular joint injection can improve the accuracy of the injection [29,30]. Injection by the palpation method is truly in the joint 40% to 60% of the time [29,31]. Use of ultrasound [29,30] or an image intensifier [31] ensures 100% accurate needle placement. It is not clear that use of ultrasound improves outcome [30]. The ultrasound-guided approach is somewhat different (Fig. 10.9) as a lateral to medial approach is advocated [29].
Postinjection care should include local icing for 10 to 15 minutes and instructions to the patient to avoid aggravating activities for at least 1 week.
Surgery
Type IV, type V, and type VI injuries are forms of dislocation of the acromioclavicular joint. These need to be reduced surgically with some form of reconstruction attempted. Early referral is indicated to minimize pain and dysfunction. Because the scapula is no longer suspended from the clavicle, the deltoid and trapezius muscles will become involved in an attempt to hold the scapula in place. These muscles may have been injured directly and therefore are ill-suited to take on the role of suspending the arm. The result is more significant pain and a greater chance for prolonged disability.
If the patient has sustained a fracture, surgery may be necessary, and referral to an orthopedist is appropriate. The severity of the injury depends on whether the fracture is medial to the coracoclavicular ligaments or involves the acromioclavicular joint itself. Fractures medial to the ligaments can result in displacement of the clavicle, and the patient therefore runs the risk of delayed union or nonunion. The displacement can look like a type II or type III sprain. Careful examination of the location and degree of pain should suggest an injury to the clavicle. Regardless, radiographs are indicated to assess the possibility of fracture.
Fractures into the joint are likely to lead to arthrosis in the future. These patients may not need surgery initially—that will be decided by the patient and the orthopedist—but may require a protracted conservative course of symptomatic treatment.
Resection of the distal clavicle, tacking of the acromion to the clavicle, re-creation of the ligaments, and screw fixation of the acromioclavicular joint or of the clavicle to the coracoid process have been used to stabilize the joint. The goal of any surgical procedure is to try to re-create a stable, pain-free joint [5].
Postoperative outcome of surgical repair of type V injuries was excellent in 11 of 12 patients after 2 years [7]. Twenty-one years after surgical treatment of type III injuries, 92% of patients had satisfactory results and no pain and would have the procedure again [32].
Potential Disease Complications
Patients may be left with a “bump” due to the depression of the acromion relative to the clavicle. This should be expected and is unavoidable without surgery. Acromioclavicular joint pain due to chronic instability is the most common complication [5,33]. Degenerative arthritis can occur because of the injury or instability. This can be treated symptomatically with modalities and injections. One in five patients with a grade I or grade II injury will have restriction in range of motion, but less than 10% will have symptoms that restrict daily or athletic activity [34].
If the pain persists, surgery should be considered. In one study, more than 25% of patients with grade I or grade II injuries required surgery 2 years after the injury [10].
Concomitant disorders of the glenohumeral joint complex can develop along with acromioclavicular arthrosis. These include rotator cuff tears, glenoid labrum tears, glenohumeral arthrosis, and biceps tendon disease [9].
Potential Treatment Complications
Analgesics and nonsteroidal anti-inflammatory drugs have well-known side effects that most commonly affect the gastric, hepatic, and renal systems. Cyclooxygenase 2 inhibitors may have fewer gastric side effects, but cardiovascular risks should be considered. Injection of the joint with too long a needle may result in injection into the subacromial space. This can cause diagnostic confusion, if not outright injury [2]. Injections can also be associated with infection in rare cases.
Direct complications of surgery can include infection, pain, wound or skin breakdown, and hypertrophic scar [5,23,35]. After surgery, there can be a recurrence of the deformity [23,25], hardware failure or migration [6,23,32,35], or limitation of movement. Pain may persist as a result of insufficient resection, weakness, or joint instability [2]. Acromioclavicular arthrosis may develop after surgery, although this may not adversely affect the patient’s function [7,32].
Recalcification after acromioclavicular joint resection can be a cause of pain and may require revision of the distal clavicle resection [35]. Likewise, distal osteolysis of the clavicle can occur, requiring revision surgery [36]. Coracoclavicular ligament ossification may develop, although this is not typically painful [32].