CASE 1 Restenosis of a Drug-Eluting Stent
Case presentation
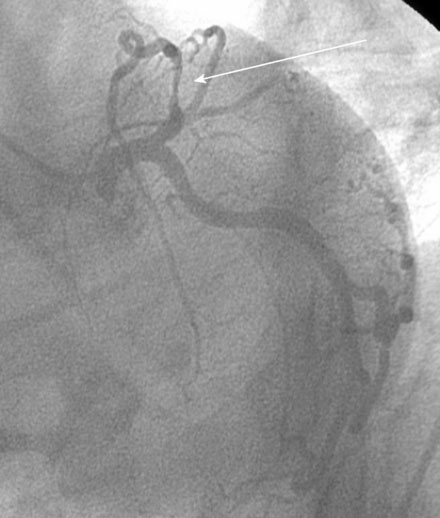
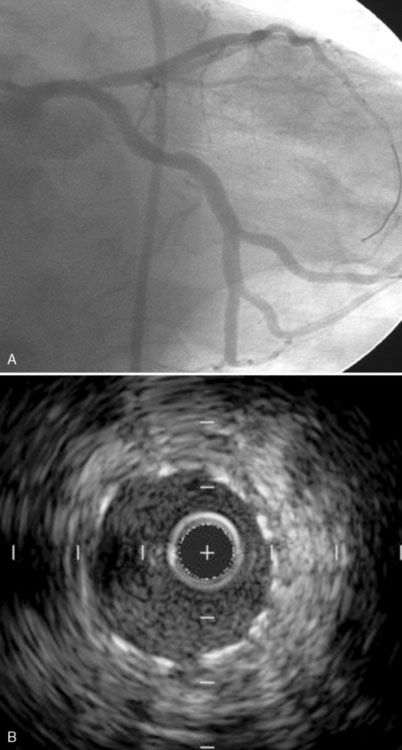
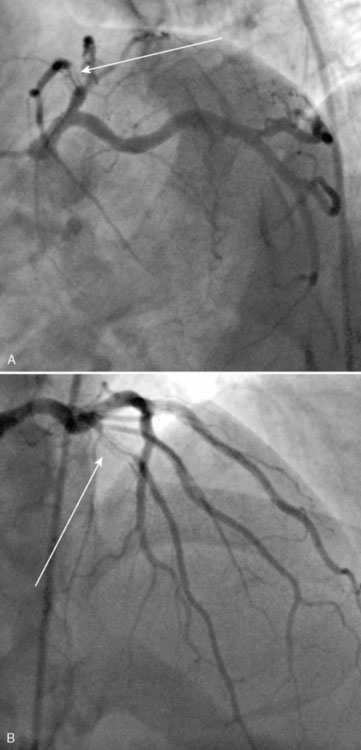
Two years earlier, he first developed classic effort angina. An abnormal stress test led to a coronary angiogram, which revealed a severe stenosis in the proximal segment of the left anterior descending coronary artery (Figure 1-1 and Video 1-1). This was treated with a 3.0 mm diameter by 23 mm long sirolimus-eluting stent, with an excellent angiographic result (Figure 1-2 and Video 1-2). His angina completely resolved; however, 10 months after the procedure, he developed recurrent effort angina. Coronary angiography confirmed severe, focal, in-stent restenosis within the proximal edge of the drug-eluting stent (Figure 1-3). Balloon angioplasty using a 3.0 mm noncompliant balloon dilated to 16 atmospheres improved the angiographic appearance (Figure 1-4 and Video 1-3) and resolved the patient’s symptoms. However, 6 months later (and 9 months before his current presentation) the development of recurrent angina prompted another angiogram. A second recurrence of in-stent restenosis within the proximal left anterior descending artery stent (Figure 1-5 and Video 1-4) was treated with a 3.0 mm diameter by 30 mm long zotarolimus-eluting stent, again with good angiographic result (Figure 1-6A). Intravascular ultrasound performed after this procedure demonstrated excellent stent apposition throughout the stented segment (Figure 1-6B). He remained symptom-free for 6 months until this presentation.
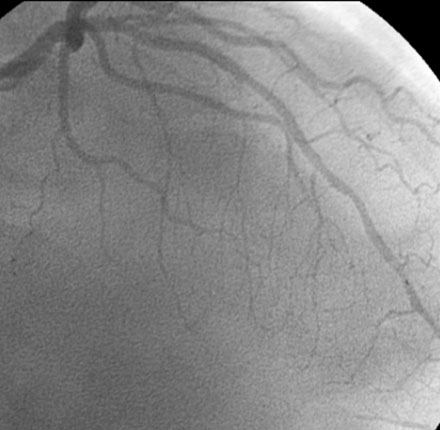
FIGURE 1-4 This is the result after balloon angioplasty of the restenotic lesion in the proximal left anterior descending artery shown in Figure 1-3.
Cardiac catheterization
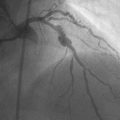
Coronary angiography again demonstrated severe narrowing of the entire stented segment of the proximal left anterior descending artery (Figure 1-7 and Video 1-5), consistent with diffuse in-stent restenosis.
Discussion
Coronary stents reduced the rate of restenosis compared to balloon angioplasty1,2; however, restenosis rates following stent placement remained unacceptably high with 15% to 20% of patients undergoing target vessel revascularization procedures within 9 months of stent implantation. Certain patient subsets, including diabetics and patients with long lesions in small caliber arteries, had rates of restenosis approaching 50% with bare-metal stents. Drug-eluting stents dramatically reduced clinical restenosis rates to about 5% to 10% in all subsets and have become the standard of care for prevention of in-stent restenosis.3,4
The mechanism of restenosis after balloon angioplasty is due to elastic recoil and negative vessel remodeling (or vessel shrinkage), while intimal proliferation is the principal mechanism causing in-stent restenosis. The important patient factors associated with bare-metal stent restenosis include diabetes mellitus, female gender, early recurrence, and chronic renal failure. The angiographic and lesion characteristics consistently associated with bare-metal stent restenosis include small vessel diameter, long lesion and stent length, complex lesion subsets (particularly bifurcation and ostial stenoses and chronic total occlusion), and in-stent restenosis lesions. Small final luminal diameter after stenting is also a factor, with optimal outcomes associated with a minimal cross-sectional area greater than 7.0 mm2 by intravascular ultrasound.5
Optimal treatment of in-stent restenosis of a bare-metal stent depends on whether the intimal proliferation is focal (less than 10 mm long) or diffuse (more than 10 mm long and typically involving the entire stent length). Focal in-stent restenosis can be successfully treated with balloon angioplasty with low rates of recurrence; intravascular ultrasound can assist the operator in determining whether stent underexpansion led to the episode of restenosis and can be used to assess the result after angioplasty. Diffuse in-stent restenosis is more problematic, with high rates of recurrence with most conventional therapies including balloon angioplasty, rotational atherectomy, and repeat bare-metal stenting. Local delivery of gamma or beta radiation via brachytherapy devices reduces restenosis, but is cumbersome and has been mostly abandoned. Currently, the treatment of choice for bare-metal stent restenosis is the use of drug-eluting stents.6
Although uncommon, restenosis of a drug-eluting stent can be particularly stubborn to manage and is associated with high rates of subsequent recurrence, as is demonstrated in the case presented here. Among drug-eluting stents, there is no clear difference in rates of restenosis between stent types, although there appears to be greater late lumen loss with paclitaxel-eluting stents compared to sirolimus-eluting stents.7 Intimal proliferation remains the dominant mechanism for drug-eluting stent restenosis; however, many of the episodes occur at the stent edges, and most are focal in-stent restenosis. Presumed causes include stent underexpansion, stent fracture, nonuniform drug deposition or polymer disruption during insertion of the stent, and drug resistance. Predictors are essentially the same as for bare-metal restenosis and include stent length, diabetes, post-procedure minimal luminal diameter, and complex lesion morphology.
1 Fischman D.L., Leon M.B., Baim D.S., Schatz R.A., Savage M.P., Penn I., Detre K., Veltri L., Ricci D., Nobuyoshi M., Cleman M., Heuser R., Almond D., Teirstein P.S., Fish R.D., Colombo A., Brinker J., Moses J., Shaknovich A., Hirshfeld J., Bailey S., Ellis S., Rake R., Goldberg S. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. N Engl J Med. 1994;331:496-501.
2 Serruys P.W., DeJaegere P., Kiemeneij F., Macaya C., Rutsch W., Heyndrickx G., Emanuelsson H., Marco J., Legrand V., Materne P., Belardi J., Sigwart U., Colombo A., Goy J.J., Van Den Heuvel P., Delcan J., Morel M. A comparison of balloon expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. N Engl J Med. 1994;331:489-495.
3 Weisz G., Martin B., Leon M.B., Holmes D.R., Kereiakes D.J., Popma J.J., Teirstein P.S., Cohen S.A., Wang H., Cutlip D.E., Moses J.W. Five-year follow-up after sirolimus-eluting stent implantation results of the SIRIUS (sirolimus-eluting stent in de-novo native coronary lesions) trial. J Am Coll Cardiol. 2009;53:1488-1497.
4 Stone G.W., Ellis S.G., Cannon L., et al. Comparison of a polymer-based paclitaxel-eluting stent with a bare-metal stent in patients with complex coronary artery disease: a randomized controlled trial. JAMA. 2005;294:1215-1223.
5 Hong M.K., Park S.W., Mintz G.S., Lee N.H., Lee C.W., Kim J.J., Park S.J. Intravascular ultrasonic predictors of angiographic restenosis after long coronary stenting. Am J Cardiol. 2000;85:441-445.
6 Kastrati A., Mehilli J., von Beckerath N., Dibra A., Hausleiter J., Pache J., Schuhlen H., Schmitt C., Dirschinger J., Schomig A., ISAR-DESIRE Study Investigators. Sirolimus-eluting stent or paclitaxel-eluting stent vs. balloon angioplasty for prevention of recurrences in patients with coronary in-stent restenosis: A randomized controlled trial. JAMA. 2005;293:165-171. for the
7 Cosgrave J., Melzi G., Corbett S., Biondi-Zoccai G.G.L., Agostoni P., Babic R., Airoldi F., Chieffo A., Sangiorgi G.M., Montorfano M., Michev I., Carlino M., Colombo A. Comparable clinical outcomes with paclitaxel- and sirolimus-eluting stents in unrestricted contemporary practice. J Am Coll Cardiol. 2007;49:2320-2328.