Topic 1 Coronary circulation
Coronary blood flow
Oxygen consumption of myocardium at rest = 8–10 ml/min/100 g.
The heart receives ~5% of total cardiac output.
During exercise myocardial oxygen consumption can increase to > 40 ml/min/100 g.
Coronary anatomy
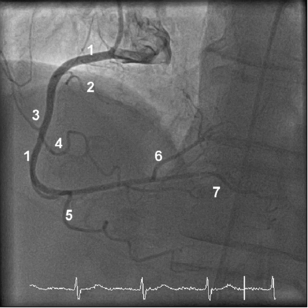
Right coronary artery (RCA) (see Figure 1.1)
Arises from the right coronary sinus.
The posterolateral branch supplies the basal posterolateral LV wall.
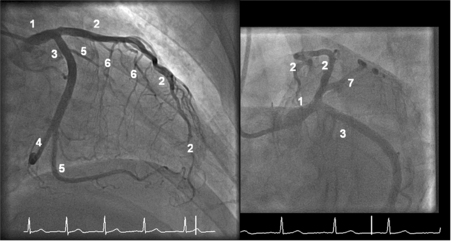
Left coronary artery (see Figure 1.2)
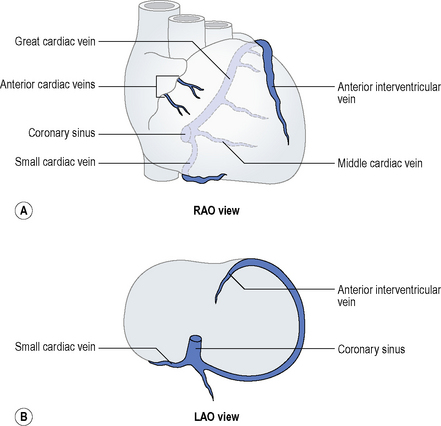
Coronary venous anatomy
Most venous drainage of the heart passes into the right atrium via the coronary sinus, the ostium of which lies in the posteroinferior interatrial septum. It receives blood from the middle cardiac vein (which runs in the posterior interventricular groove, alongside the posterior descending artery) and it is in continuity with the great cardiac vein (which runs parallel to the left circumflex artery). The anterior interventricular vein runs with the left anterior descending artery and drains into the great cardiac vein. The great cardiac vein also receives tributaries from the left marginal vein and left posterior vein. The small cardiac vein receives tributaries draining the right ventricle and also drains into the coronary sinus. The anterior cardiac vein returns blood separately to the right atrium and there are additional small veins that open directly into the cardiac chambers. The coronary venous anatomy when viewed in the LAO and RAO configurations is displayed in Figure 1.3.
Coronary artery anomalies
Congenital coronary artery anomalies include:
Clinically important anomalies
Anomalies associated with adverse events include: