CHAPTER 1 Autonomic Nervous System
1 Describe the autonomic nervous system
The autonomic nervous system (ANS) is a network of nerves and ganglia that controls involuntary physiologic actions and maintains internal homeostasis and stress responses. The ANS innervates structures within the cardiovascular, pulmonary, endocrine, exocrine, gastrointestinal, genitourinary, and central nervous systems (CNS) and influences metabolism and thermal regulation. The ANS is divided into two parts: the sympathetic (SNS) and parasympathetic (PNS) nervous system. When stimulated, the effects of the SNS are widespread across the body. In contrast, PNS stimulation tends to produce localized, discrete effects. The SNS and PNS generally have opposing effects on end-organs, with either the SNS or the PNS exhibiting a dominant tone at rest and without exogenous stimulating events (Table 1-1). In general the function of the PNS is homeostatic, whereas stimulation of the SNS prepares the organism for some stressful event (this is often called the fight-or-flight response).
| Sympathetic Nervous System | Parasympathetic Nervous System |
|---|---|
| Arterioles | Sinoatrial node |
| Veins | Gastrointestinal tract |
| Sweat glands | Uterus |
| Urinary bladder | |
| Salivary glands | |
| Iris | |
| Ciliary muscle |
KEY POINTS: Autonomic Nervous System 
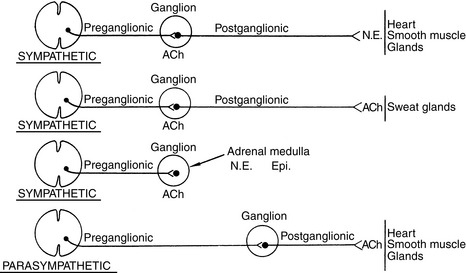
2 Review the anatomy of the sympathetic nervous system
Preganglionic sympathetic neurons originate from the intermediolateral columns of the thoracolumbar spinal cord. These myelinated fibers exit via the ventral root of the spinal nerve and synapse with postganglionic fibers in paravertebral sympathetic ganglia, unpaired prevertebral ganglia, or a terminal ganglion. Preganglionic neurons may ascend or descend the sympathetic chain before synapsing. Preganglionic neurons stimulate nicotinic cholinergic postganglionic neurons by releasing acetylcholine. Postganglionic adrenergic neurons synapse at targeted end-organs and release norepinephrine (Figure 1-1).
3 Elaborate on the location and names of the sympathetic ganglia. Practically speaking, what is the importance of knowing the name and location of these ganglia?
4 Describe the postganglionic adrenergic receptors of the sympathetic nervous system and the effects of stimulating these receptors
There are α1, α2, β1, and β2 adrenergic receptors. The A1, A2, and B2 receptors are postsynaptic and are stimulated by the neurotransmitter norepinephrine. The A2 receptors are presynaptic, and stimulation inhibits release of norepinephrine, reducing overall the autonomic response. Molecular pharmacologists have further subdivided these receptors, but this is beyond the scope of this discussion. Dopamine stimulates postganglionic dopaminergic receptors, classified as DA1 and DA2. The response to receptor activation in different sites is described in Table 1-2.
TABLE 1-2 End-Organ Effects of Adrenergic Receptor Stimulation
| Receptor | Organ | Response |
|---|---|---|
| β1 | Heart | Increases heart rate, contractility, and conduction velocity |
| Fat cells | Lipolysis | |
| β2 | Blood vessels | Dilation |
| Bronchioles | Dilation | |
| Uterus | Relaxation | |
| Kidneys | Renin secretion | |
| Liver | Gluconeogenesis, glycogenolysis | |
| Pancreas | Insulin secretion | |
| α1 | Blood vessels | Constriction |
| Pancreas | Inhibits insulin release | |
| Intestine, bladder | Relaxation but constriction of sphincters | |
| α2 | Presynaptic nerve endings | Inhibits norepinephrine release |
| Dopamine-1 | Blood vessels | Dilates renal, coronary, and splanchnic vessels |
| Dopamine-2 | Presynaptic endings | Inhibits norepinephrine release |
| Central nervous system | Psychic disturbances |
5 Review the anatomy and function of the parasympathetic nervous system
Preganglionic parasympathetic neurons originate from cranial nerves III, VII, IX, and X and sacral segments 2-4. Preganglionic parasympathetic neurons synapse with postganglionic neurons close to the targeted end-organ, creating a more discrete physiologic effect. Both preganglionic and postganglionic parasympathetic neurons release acetylcholine; these cholinergic receptors are subclassified as either nicotinic or muscarinic. The response to cholinergic stimulation is summarized in Table 1-3.
TABLE 1-3 End-Organ Effects of Cholinergic Receptor Stimulation
| Receptor | Organ | Response |
|---|---|---|
| Muscarinic | Heart | Decreased heart rate, contractility, conduction velocity |
| Bronchioles | Constriction | |
| Salivary glands | Stimulates secretion | |
| Intestine | Contraction and relaxation of sphincters, stimulates secretions | |
| Bladder | Contraction and relaxation of sphincters | |
| Nicotinic | Neuromuscular junction | Skeletal muscle contraction |
| Autonomic ganglia | SNS stimulation |
SNS, Sympathetic nervous system.
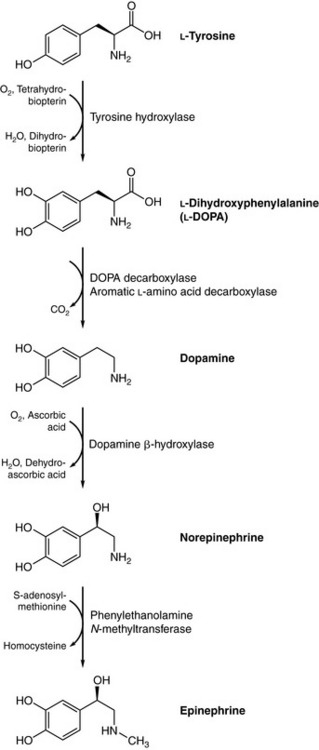
7 Review the synthesis of dopamine, norepinephrine, and epinephrine
The amino acid tyrosine is actively transported into the adrenergic presynaptic nerve terminal cytoplasm, where it is converted to dopamine by two enzymatic reactions: hydroxylation of tyrosine by tyrosine hydroxylase to dopamine and decarboxylation of dopamine by aromatic l-amino acid decarboxylase. Dopamine is transported into storage vesicles, where it is hydroxylated by dopamine β-hydroxylase to norepinephrine. Epinephrine is synthesized in the adrenal medulla from norepinephrine through methylation by phenylethanolamine N-methyltransferase (Figure 1-2).
11 Review the sympathomimetics commonly used in the perioperative environment
Direct-acting sympathomimetics are agonists at the targeted receptor, whereas indirect-acting sympathomimetics stimulate release of norepinephrine. Sympathomimetics may be mixed in their actions, having both direct and indirect effects. Practically speaking, phenylephrine (direct acting) and ephedrine (mostly indirect acting) are the sympathomimetics commonly used perioperatively. Also, epinephrine, dopamine, and norepinephrine may be used perioperatively and most often by infusion since their effects on blood pressure, heart rate, and myocardial oxygen consumption can be profound. Dopamine is discussed in Chapter 15.