Administration
Medication Administration
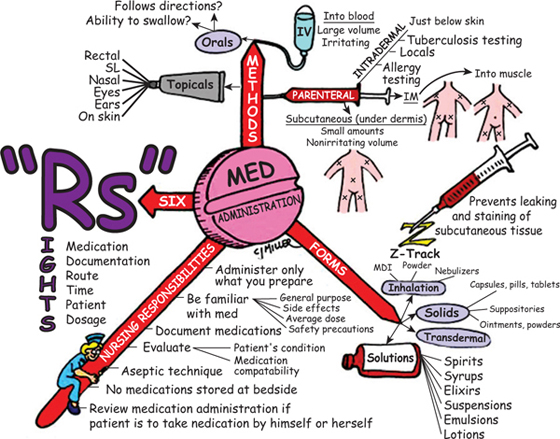
SIX RIGHTS OF MEDICATION ADMINISTRATION
ROUTES OF ADMINISTRATION
• Enteral or oral (most common)—ingested into gastrointestinal tract.
• Topical—absorbed across skin or mucous membrane.
• Inhalation—inhaled directly into lung to elicit local effects.
• Rectal and vaginal suppository—inserted for local effects.
NURSING IMPLICATIONS
1. Only administer medications you have prepared.
2. *Read medication label carefully; not all formulations of parenteral medications are appropriate for IV administration (e.g., regular insulin for IV use).*
• Why is this patient receiving this medication?
• What nursing observations will tell you the desired medication action is occurring?
• What are the nursing implications specific to this medication?
4. Do not leave medications at the bedside.
5. Check medication compatibility if administering IV.
6. *Medications prepared for one route may differ in concentration for another different route (e.g., epinephrine SC is concentrated, whereas IV preparation is dilute).*
• †Administering an SC epinephrine preparation IV could be fatal because of an overstimulation of the cardiac system.†
7. *Always check the patient’s armband before administering any type of medication.*
8. Have another nurse check medication calculations.
• *Do not inject more than 3 ml at one time.*
• Use the smallest needle necessary to administer medication correctly.
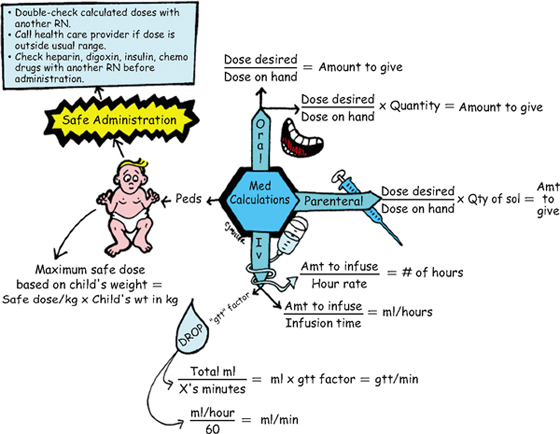
Medication Calculation
METHODS OF CALCULATION
• Drugs requiring individualized dosing can be calculated by body weight (BW) or body surface area (BSA).
NURSING IMPLICATIONS
1. Always have another registered nurse (RN) double-check medications when you have had to calculate the dosage.
2. Consult the health care provider if the dosage is outside the recommended range.
3. Do not administer medications if someone else has calculated the dose for you; *administer only those medications you have calculated and prepared.*
4. *Be very cautious about calculating drug dosages for pediatric patients.*
5. Just because an intravenous (IV) pump for the patient is in place, it does not mean that you do not need to know how many milliliters per hour you should be infusing. This infusion rate is important to know to set the pump and to check the accuracy of delivery.
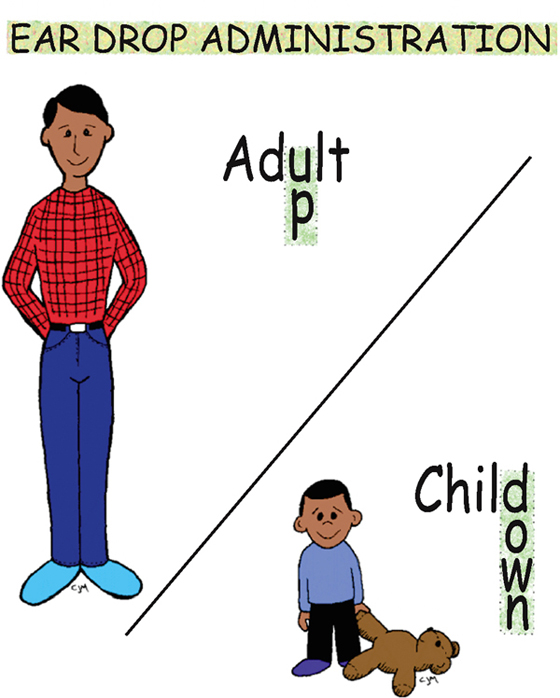
Ear Drop Administration
PROCEDURE
• Position patient supine on his or her side with affected ear up.
• *Medication should be at least room temperature, not cold.*
• *Open ear canal of an adult by drawing back on the pinna and slightly upward.*
• *Open ear canal of a child under 3 years of age by drawing back on the pinna and slightly downward.*
• Instill medication, and allow it to flow into the ear by gravity.
• Have patient remain supine for a few minutes to keep the medication from leaking out.
USES
NURSING IMPLICATIONS
1. *If medication is not instilled at room temperature, the patient may experience vertigo, dizziness, and nausea.*
2. †If ear drainage if observed, assess patient and determine whether the eardrum is ruptured. If ruptured, do not administer medication until health care provider is consulted.†
3. Do not occlude ear canal with dropper or syringe.
4. ‡Never force medication into an occluded ear canal; doing so creates pressure, which could damage or rupture the eardrum.‡
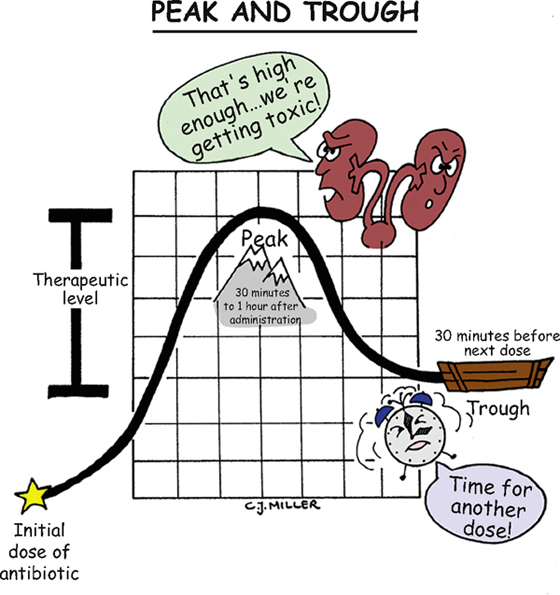
Peak and Trough
USES
• *Is primarily used to monitor levels of the aminoglycoside family of antibiotics.* Monitoring serum drug levels enables the physician to individualize dosage levels to maximum effectiveness, which allows drug levels to be at an effective but not toxic level.
NURSING IMPLICATIONS
1. *If the trough level is too high, toxicity can occur.* †Nephrotoxicity and ototoxicity are primary problems of the aminoglycosides.†
2. If the peak is too low, no or minimal therapeutic effect is achieved.
3. *Check laboratory values for peak and trough levels.*
4. *Report serum levels that are not within established ranges of peak and trough levels.*
5. Explain to the patient the purpose for the peak and trough levels.
6. Maintain accuracy of values; ensure that serum laboratory values are drawn at scheduled times.
7. Risk of toxicity is increased in patients with decreased renal function.
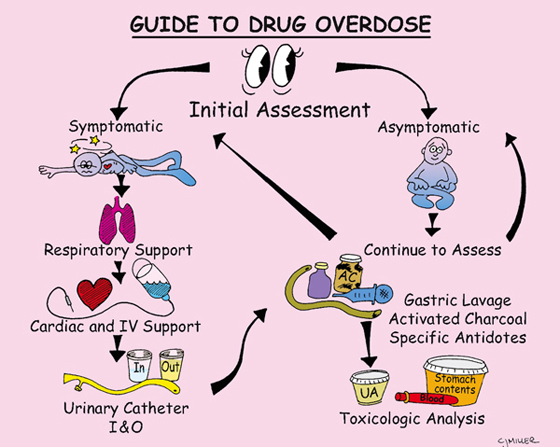
Guide to Drug Overdose
NURSING MANAGEMENT
1. *Make an initial assessment, including vital signs and level of consciousness.*
2. The specific drug taken in the overdose will dictate the treatment.
• Obtain information about amount of drug, time, and underlying medical problems.
• ‡Direct family member or other individual to bring drug and/or container to the emergency department.‡
3. Perform gastric lavage to remove unabsorbed drugs mechanically from the stomach.
4. Activated charcoal may be given to help bind drugs and keep them in the stomach and intestines.
• Activated charcoal reduces the amount of drug absorbed into the blood.
• The drug, bound to the charcoal, is then expelled in the stool.
5. †Respiratory and cardiac support may be required for symptomatic cases.†
6. *Intravenous lines, laboratory tests for toxicologic analysis, and a urinary catheter may also be ordered.*
Helpful mnemonic for opiate overdose:
Cool to the touch and unresponsive to pain.
Hunger diminished and scars over vein.
Pupils pinpointed and blood pressure low.
Urine diminished and breathing slow.
Another mnemonic to help you remember the most rapid (speedy) way toxins or medications enter the body:
4 Ss—Stick it, Sniff it, Suck it, Soak it
Stick: injection; Sniff: inhalation; Suck: ingestion; Soak: absorption
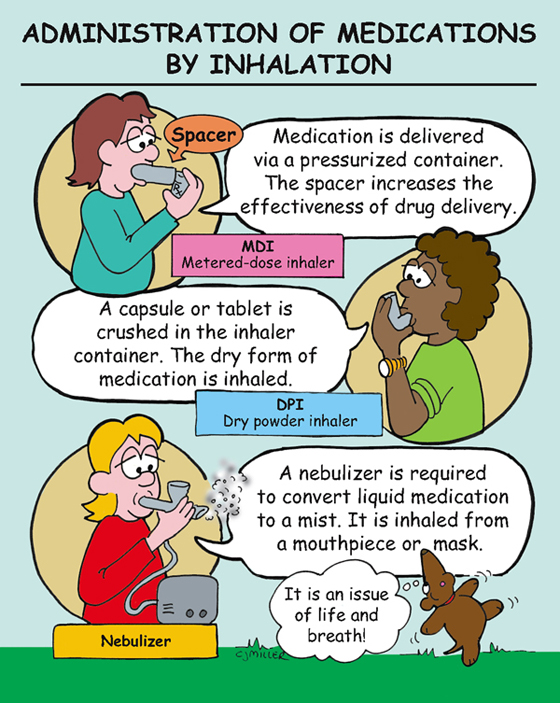
Administration of Medications by Inhalation
METERED-DOSE INHALER (MDI)
• Hand-held pressurized containers deliver a measured dose of medication with each “puff.”
• Dosing may require two “puffs”—patient should wait 1 minute between “puffs.”
• *Patient should hold his or her breath for approximately 10 seconds after inhalation.*
DRY POWDER INHALER (DPI)
• Each medication comes with a delivery system. Medication should be administered only with delivery system provided. No aerosol propellant is used.
• *Capsules and tablets are to be administered by inhalation only; medications are not to be taken by mouth.*
• Delivery system crushes medication to a fine powder to be inhaled.
• ‡After system is loaded, teach patient to cover mouthpiece and inhale deeply.‡
• Compared with MDIs, medication delivery is significantly more efficient.
SMALL-VOLUME NEBULIZERS
• A small machine converts a medication solution to a nebulized or mist form.
• *Determining whether a dilutant needs to be added to the medication to facilitate the delivery is important.*
• *Most effective method of delivery is via mouthpiece; however, medication may also be delivered via face mask.*
• ‡When the mist begins to form at the end of mouthpiece, ask patient to seal his or her mouth over mouthpiece and start a slow, deep breath; patient should hold his or her breath for a short time and then exhale slowly.‡
• ‡Mouth should be rinsed after treatment, and equipment should be rinsed and allowed to dry. Do not store wet equipment.‡
• ‡With inhaled steroid medications, mouth should be rinsed to prevent infections.‡
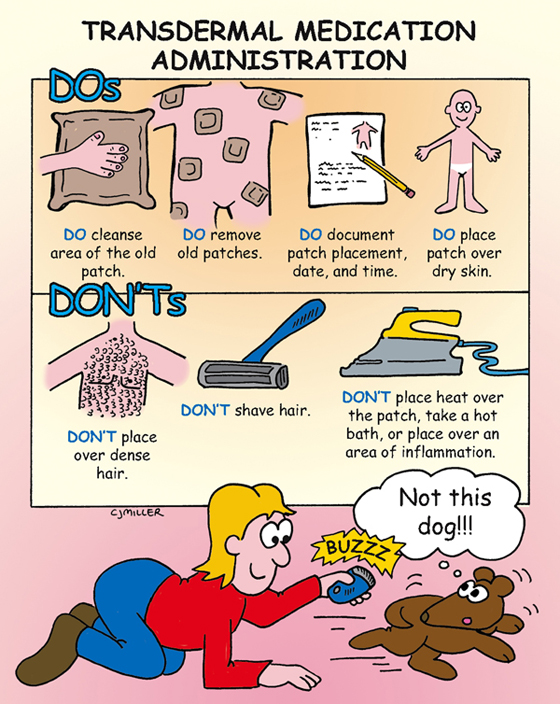
Transdermal Medication Administration
GENERAL
• Transdermal medications are administered topically, absorbed through the skin into the blood, and exert a systemic effect.
• Avoids first-pass metabolism, and decreases bioavailability of medication.
• Provides a controlled, constant release of medication.
• Patients who are obese or diaphoretic may have difficulty absorbing the medication.
• *If a patient is going to have a magnetic resonance imaging (MRI) examination, make sure the patch of transdermal medication does not contain a metallic component. The U.S. Food and Drug Administration (FDA) recommends that health care professionals note the presence of a patch when they refer patients for an MRI examination. The patch may be removed before the examination and replaced after.*
• *Heat increases the absorption of transdermal medications. Check with the practitioner before administering a medication patch to a patient who has a temperature higher than 102° F.*
• *Do not apply any heat over patch; doing so will increase absorption of medication.*
• *Do not allow medication to come in direct contact with fingers.*
ADMINISTRATION GUIDELINES
1. Follow principles of medication administration.
2. *Apply patch to dry, hairless area of subcutaneous tissue—preferably the chest, abdomen, or upper back.*
3. *Remove old patch and cleanse area; apply new patch in a different area.*
4. *Do not apply a patch over an area of emaciated skin or on an area with irritated or broken skin.*
5. *Do not apply an adhesive dressing over the patch.*
6. *Dispose old patches according to facility guidelines. Of specific concern is proper disposal of fentanyl patches.*