Forensic Emergency Medicine
Perspective
Clinical forensic medicine is the application of forensic medical knowledge and techniques to live patients in a clinical setting. European, Australian, and British physicians—known as police surgeons, forensic physicians, forensic medical examiners, or forensic medical officers1,2—have a long history of performing clinical forensic examinations,3 including evaluations of prisoners and victims of physical and sexual assault.4,5
All patients who are victims of physical or sexual assault, abuse, or trauma have forensic needs. When treating injuries without consideration of their forensic significance, physicians may misinterpret wounds, fail to recognize victims of abuse or domestic violence, and inadequately describe the physical appearance of the wounds. During the provision of patient care, evidence that can be of critical significance to criminal or civil proceedings can be lost, discarded, or inadvertently washed away,6–20 despite requirements by The Joint Commission (TJC) to “preserve evidentiary materials and support future legal actions.”21
Emergency medicine programs have identified and described the need for forensic training in their residency curricula.9,10,14,22 In 1991 the Department of Emergency Medicine at the University of Louisville School of Medicine collaborated with the Kentucky Medical Examiner’s Office and established the first clinical forensic medicine training and consultative program in the United States.9,13,19,20 In 2006, the American College of Emergency Physicians established the Forensic Medicine Section to provide emergency physicians with additional forensic resources and training.23 In 2010 the Louisville Police Department created a full-time clinical forensic medicine consultation service to provide forensic evaluations for living victims of crimes, staffed by a forensic emergency physician and three part-time forensic nurse examiners.
Forensic examinations are conducted with the consent of the patient, legal guardian, or court, or by implied consent. The evaluation includes a history and physical examination, photographs, and anatomic diagrams.22 Evidentiary material, including clothing, hair, blood, saliva, bullets, bomb fragments, and the like, are collected when indicated or when ordered by the court.24 If a patient has been admitted from the emergency department (ED) to surgery, an evaluation is done in the operating suite in conjunction with the trauma surgeons.25
In 2006 the British Royal College of Physicians established the Faculty of Forensic and Legal Medicine (FFLM) as the authoritative body on clinical forensic medicine in the United Kingdom.26 The FFLM has created training and certification programs and board-type certification examinations after 2 years of forensic practice for British physicians.26
Evaluations of gunshot and stab wounds, physical or sexual abuse, domestic violence, and motor vehicle–related trauma should be adequately documented for possible use in future legal proceedings. Documentation should include digital photographs as well as a narrative and diagrams.7–13,17–2225 However, in one trauma center, 70% of cases had improper or inadequate documentation, and 38% of cases had potential evidence improperly secured, incorrectly documented, or inadvertently discarded.8 When physical injuries are misinterpreted and these misinterpretations become the medical record or when valuable evidence is lost or destroyed in the process of providing patient care, there are consequences for the legal proceedings that may follow.3,6–20,26–30 These acts of omission or commission may deny patients their deserved redress in the justice system. To protect the interests of patients, EDs should implement protocols for wound documentation and evidence collection.11,12
Forensic Aspects of Gunshot Wounds
Firearms continue to be the second leading cause of injury-related deaths in the United States—30,913 firearm-related deaths in 2009—after motor vehicle trauma.31 Emergency physicians treat more than 115,000 victims of gunshot wounds, principally from handguns, each year.32 The direct and indirect costs associated with gunshot wounds total $36 billion annually.33
Errors of Interpretation and Terminology
The emergency physician is in the ideal position to evaluate and document the state of a gunshot wound because he or she sees and explores it before it is disturbed, distorted, or destroyed by surgical intervention.6–14,27,30 Documentation of gunshot wounds should include the anatomic location of the wound as well as its, size, shape, and distinguishing characteristics, and digital photographs of the wound should be taken. Wounds should be described according to the standard anatomic position with the arms to the sides and palms up.
Clinicians should not describe wounds as “entrance” or “exit” but should document, using appropriate forensic terminology, a detailed description of the wound, including its appearance, characteristics, and location without attempting to interpret the wound type or bullet caliber.27,34–39 Exit wounds are not always larger than entrance wounds, and wound size does not consistently correspond to bullet caliber.18,27,36–42
The size of any wound (entrance or exit) is determined by five factors: the size, shape, configuration or angle, and velocity of the projectile at the instant of impact with tissue and the physical characteristics of the impacted tissue itself. If the projectile is slowed and its shape unchanged on exiting the skin, the exit wound may be the same size as or smaller than the corresponding entrance wound.34,41,42 If the projectile increases its surface area by fragmenting or changing its configuration while maintaining a substantial velocity, the exit wound may be significantly larger than the entrance wound.34,36–42 If the bullet strikes bone, fragments may extrude from the exit wound and contribute to the size and shape of the wound. Tissue elasticity also affects the wound size so that entrance or exit wounds may be smaller, equal to, or larger than the projectile that caused them.40–42 Wounds on the palm or sole may appear as slits and can be easily mistaken for stab wounds.34,41,42
Inappropriate terminology should be avoided.8,37,41,42 One example of inappropriate terminology is the use of the obsolete term powder burns, rather than soot, to describe the carbonaceous material associated with close-range wounds.34,35,41,42 Powder burns are literally the thermal injuries associated with flaming black powder used in muzzle loaders, antique weapons, and blank cartridges. These injuries do not occur with the smokeless powder used in modern ammunition.
A treating physician may be requested to render factual testimony, expert testimony, or both in a criminal case. Expert forensic testimony rendered without an appropriate forensic examination or adequate forensic training may mislead participants in the criminal justice system (e.g., “the exit wound is always larger than the entrance wound”). Opinions related to entrance versus exit wounds or the range of fire can affect the determination of innocence or guilt.* The perennial speculation about entrance and exit wounds in the assassination of President Kennedy is one example of the significance of a forensic evaluation.29,30,44
Forensic Aspects of Handguns
Handgun Ammunition
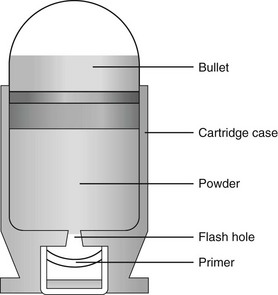
The cartridge, or round, is composed of the primer, the cartridge case, the powder, and the bullet (Fig. 65-1). The bullet is the projectile that is propelled out of the muzzle.
The primer is a small explosive charge in the base of the cartridge that ignites the gunpowder. The primer may contain lead, barium, or antimony. These materials may be deposited on the hands of the shooter, on the victim of a close-range assault, or on objects within a room in which the weapon was discharged.41
The cartridge case is typically made of brass, although other materials may be used. The function of the cartridge case is to slightly expand, sealing the chamber against the escaping gases and propelling the bullet down the barrel.41 On detonation, a cartridge case is imprinted with unique microscopic marks that are valuable evidence and should be preserved for law enforcement.
The gunpowder found in all commercial cartridges except blanks is smokeless powder made with a single base (nitrocellulose) or a double base (nitrocellulose and nitroglycerine).41 When a weapon is discharged, not all of the gunpowder is consumed. A percentage of the unburned or partially burned gunpowder will travel out of the end of the muzzle for a short distance (<48 inches). The distance depends on the physical characteristics and shape of the powder and the weapon’s barrel length.
Handgun Wound Ballistics
Wound ballistics is the study of the effects of penetrating projectiles on the body.39,45–50 Tissue disruption (wound severity) is directly related to the amount of kinetic energy ( ) transferred to it, not to the total amount of kinetic energy possessed by the bullet.39,41,45 Bullets fired from rifles generally have a higher velocity (1500 to 4000 ft/s) than do those fired from handguns (700 to 1600 ft/s). Rifle bullets have more kinetic energy and therefore a theoretically higher wounding potential, but wound severity is the result of multiple variables, the most important of which are bullet type (weight, deforming type, fragmenting type), bullet velocity, and the characteristics, location, and nature of the impacted tissue itself (tissue over bone or tissue over organs).39,41,46–50
) transferred to it, not to the total amount of kinetic energy possessed by the bullet.39,41,45 Bullets fired from rifles generally have a higher velocity (1500 to 4000 ft/s) than do those fired from handguns (700 to 1600 ft/s). Rifle bullets have more kinetic energy and therefore a theoretically higher wounding potential, but wound severity is the result of multiple variables, the most important of which are bullet type (weight, deforming type, fragmenting type), bullet velocity, and the characteristics, location, and nature of the impacted tissue itself (tissue over bone or tissue over organs).39,41,46–50
The principal mechanism for tissue damage by bullets is crushing. A bullet traveling through tissue generates two cavities, one permanent and the other temporary. The temporary cavity, a result of tissue stretching, lasts 5 to 10 msec from its generation until its collapse and leaves behind the permanently crushed tissue and the permanent cavity.39,41,45 The size of the permanent cavity varies with the size, shape, and configuration of the bullet. A hollow-point bullet that mushrooms can increase its diameter 2.5 times on impact and will increase the area of tissue crush 6.25 times compared with a nondeformed bullet.41
Forensic Evaluation of Handgun Wounds
Range of fire is the distance from the muzzle to the victim and can be divided into four general categories: contact, near-contact or close range, intermediate or medium range, and indeterminate or distant range (Table 65-1). The size of the entrance wound does not correlate with the caliber of the bullet41 because the entrance wounds over elastic tissue will contract around the tissue defect and have a diameter much less than the caliber of the bullet.34,41
Table 65-1
| RANGE | INCHES (BARREL TO SKIN) | PHYSICAL PROPERTIES |
| Contact | 0 | Soot, seared skin, triangular tears |
| Close | 0-6 | Soot, abrasion collar (abrasion collar may be obscured by soot) |
| Intermediate | <48 | Tattooing, abrasion collar |
| Distant or indeterminate | Any distance | Abrasion collar (intermediate objects will prevent soot and gunpowder from contacting the skin) |
Contact Wounds.: There are three subcategories of contact wounds: (1) tight contact, in which the muzzle is pushed hard against the skin; (2) loose contact, in which the muzzle is incompletely or loosely held against the skin; and 3) contact through clothing.
In a tight contact wound, all material—the bullet, gases, soot, the incompletely burned pieces of gunpowder, and metal fragments—is driven into the wound. These wounds can vary from a small hole with seared blackened edges from the discharge of hot gases and an actual flame to a gaping stellate wound (Fig. 65-2). Large wounds occur when the wound is inflicted over thin, inelastic or bony tissue, and the injected hot gases cause the skin to expand until it stretches and tears. These tears will have a triangular shape, with the base of the triangle overlying the entrance wound. Tears are generally associated with .32 caliber or greater, or magnum loads. Large stellate contact wounds are easily misinterpreted as exit wounds if the determination is based solely on their size (see Fig. 65-2B).34,41
Stellate tears are not pathognomonic for contact wounds, however. Tangential wounds, ricochet or tumbling bullets, and some exit wounds may also be stellate. These wounds’ appearance differs from a tight contact wound’s by the absence of soot and powder within the wound and a lack of seared wound margins.34,41,42
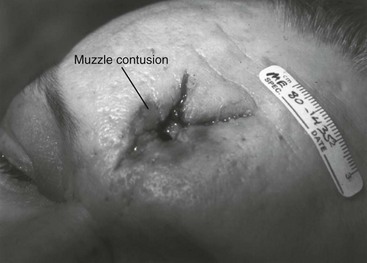
In some tight contact wounds, expanding skin is forced back against the muzzle of the gun, leaving a characteristic muzzle abrasion or muzzle contusion (Fig. 65-3).34,41,42 Patterns such as these should be documented before wound débridement or surgery because they are helpful in determining the type of weapon used (revolver vs. semiautomatic).25,41
Discharge of a weapon in contact with clothing results in the gases and soot being deposited between the garment and the skin. This results in a diffuse pattern of soot surrounding a wound with seared margins (see Fig. 65-2C).
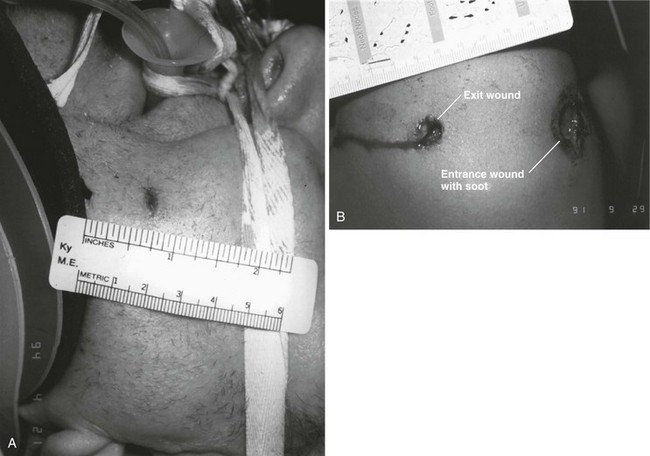
Close-Range Wounds.: Close range is the maximum range at which soot is deposited on the wound or clothing. The muzzle-to-target distance is usually less than 6 inches but may be as much as 12 inches.40–42 Beyond 6 inches, most of the soot usually falls away and does not reach the skin or clothing. The concentration of the soot varies inversely with the muzzle-to-target distance and is influenced by the type of gunpowder and ammunition used, the length of the weapon’s barrel, and the caliber and type of weapon itself (Fig. 65-4).
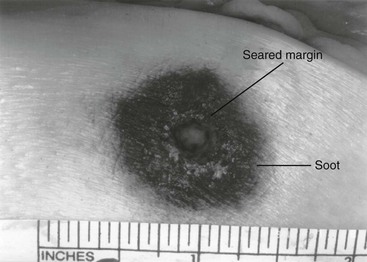
Figure 65-4 Close-range wound with soot deposition. Soot is associated with a range of fire of 6 inches or less.
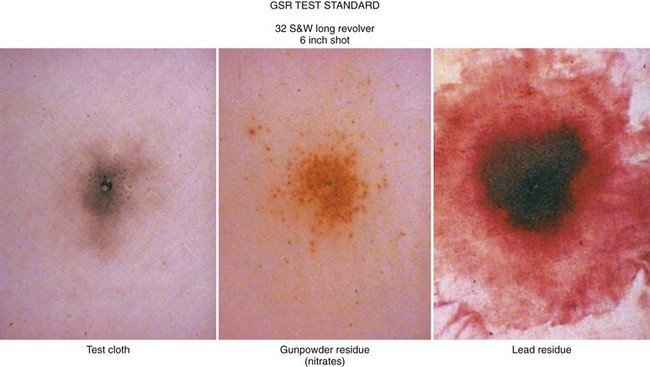
A precise range of fire (e.g., 2 inches vs. 5 inches) cannot be determined from examination of the wound alone. A forensic firearms examiner can attempt to reproduce the patient’s soot pattern on a target by test-firing the offending weapon at different ranges using ammunition similar to the ammunition that caused the wound (Fig. 65-5). The validation of this test and the determination of a range of fire depend on the accuracy and detail in the physician’s report regarding the size of the soot pattern. Because soot can be removed with débridement or wound cleansing, its presence and configuration around the wound should be noted and photographed before débridement unless the patient’s clinical condition precludes this attention to detail.25
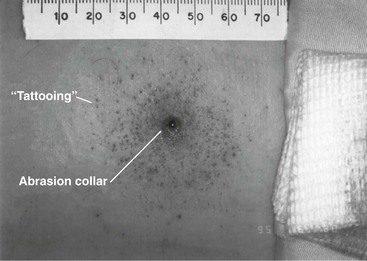
Intermediate-Range Wounds.: Tattooing, or stippling, is pathognomonic for an intermediate-range gunshot wound. Tattooing appears as punctate abrasions and is caused by contact with partially burned and wholly unburned pieces of gunpowder (Fig. 65-6). Tattooing or stippling cannot be wiped away. Tattooing rarely occurs on the palms of hands or soles of feet because of the thickness of the epithelium.41
Tattooing may occur as close as 1 cm to and as far away as 1.3 m from the weapon but is generally found at distances of 60 cm or less.40–42,51 The density of the tattooing and the associated pattern depend on the length of the barrel, the muzzle-to-skin distance, the type of gunpowder, the presence of intermediate objects, and the caliber and type of ammunition. Clothing, hair, or other barriers may prevent tattooing from occurring. The presence of partially or entirely unburned pieces of gunpowder and gunpowder residues on clothing or skin aids in determining the range of fire. On rare occasion, pieces of gunpowder can penetrate thin clothing and leave punctate abrasions (Fig. 65-7).
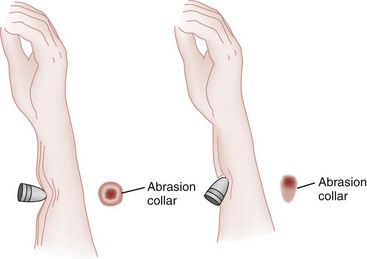
Long-Range Wounds.: The distant or long-range wound is inflicted from far enough away that only the bullet makes contact with the skin. There is no tattooing or soot. As the bullet penetrates the skin, the skin is indented, resulting in the creation of an abrasion collar, also called an abrasion margin, abrasion rim, or abrasion ring (Fig. 65-8).41,42 This collar is an abraded area of tissue that surrounds an entry wound as the result of friction between the bullet and the epithelium. The width of the abrasion collar varies with the angle of impact. Most entrance wounds will have an abrasion collar. Entrance wounds on the palms and soles are exceptions. These usually appear slitlike.41
Determining the range of fire may be complicated when clothing prevents the deposition of soot and powder on the skin. Without the overlying clothing or without information regarding the crime scene, the wound may appear to be from a distant range of fire. In reality, the range may have been close or intermediate. Conversely, a projectile discharged from a distant range of fire may mimic an intermediate range if it strikes an object, such as glass, that fragments. As with unburned gunpowder, when the glass fragments strike the skin, they may also cause punctate abrasions, resulting in pseudotattooing (Fig. 65-9).41,52
Atypical Entrance Wounds.: Atypical entrance wounds occur when a bullet encounters an intermediate object, such as a window, wall, or door, before striking the victim. The intermediate object may change the bullet’s size, shape, or path. Such changes can result in entrance wounds with large stellate configurations that mimic close-range or contact wounds (Fig. 65-10).53,54 Ricochet bullets may also cause atypical entrance wounds.
Graze wounds are atypical wounds from tangential contact with a passing bullet. Directionality of the bullet may be determined from a close examination of the wound.41,55,56 The bullet produces a trough with the formation of skin tags on the lateral wound margins that point toward the weapon and away from the direction in which the bullet was traveling (Fig. 65-11).55
Exit Wounds
The size of the exit wound is determined by the energy transferred from the bullet to underlying tissue and by the bullet’s size and configuration as it exits the skin (Fig. 65-12).41,42 When a bullet enters the skin, its configuration may change from its usual nose-first attitude owing to tumbling and yaw. A bullet that exits the skin sideways, or one that has increased its surface area by mushrooming or transferring its energy to underlying bone, will have an exit wound larger than its entrance wound.34,41
Atypical Exit Wounds.: A shored-exit wound is a wound that has an associated false abrasion collar. If the skin is pressed against or supported by a firm object or surface at the moment the bullet exits, the skin can be compressed between the exiting bullet and the supporting surface (Fig. 65-13).41,42,57 Examples of supporting structures include belts, floors, walls, doors, chairs, and mattresses.
Rarely, soot may also be present at an atypical exit wound site.58 If a contact entrance wound is located close to its associated exit wound, soot can be propelled through the short wound track and appear faintly on the exit wound surface (Fig. 65-14).
Forensic Evaluation of Centerfire Rifle Wounds.: Projectiles discharged from centerfire rifles have the potential to inflict massive tissue damage (Fig. 65-15). A bullet’s wounding potential is based on the kinetic energy it possesses. Centerfire bullets, .223 to .308 caliber, are similar in diameter to handgun ammunition, but based on the formula for kinetic energy ( ), their wounding potential is greatly enhanced by the higher velocity of the round.41 Injuries result from the transference of energy from the projectile to tissue, organs, and bony structures. With medium-velocity rounds (2000-3000 ft/s) and high-velocity rounds (>3000 ft/s), a temporary cavity is formed along the wound tract, which may be 11 or 12 times the diameter of the bullet. High velocity rounds can also cause tissue damage away from the physical tract taken by the projectile.45 Because of the amount of energy possessed and transferred to underlying tissue, exit wounds associated with centerfire rifles, in contrast to those associated with handguns, are generally larger than their corresponding entrance wounds (see Fig. 65-15).41,42
), their wounding potential is greatly enhanced by the higher velocity of the round.41 Injuries result from the transference of energy from the projectile to tissue, organs, and bony structures. With medium-velocity rounds (2000-3000 ft/s) and high-velocity rounds (>3000 ft/s), a temporary cavity is formed along the wound tract, which may be 11 or 12 times the diameter of the bullet. High velocity rounds can also cause tissue damage away from the physical tract taken by the projectile.45 Because of the amount of energy possessed and transferred to underlying tissue, exit wounds associated with centerfire rifles, in contrast to those associated with handguns, are generally larger than their corresponding entrance wounds (see Fig. 65-15).41,42
Entrance wounds associated with high-velocity, centerfire projectiles do not significantly differ from those of handguns. Entrance wounds will generally exhibit abrasion collars or microtears on the skin surface (Fig. 65-16). Wounds will also have associated soot deposition and tattooing, but because of a number of variables, such as muzzle length, amount of power in a given cartridge, muzzle configuration, and type of gunpowder, the range of fire in rifle wounds is not as clearly defined as in handgun wounds. The determination of an exact range of fire for rifles and shotguns is best established through controlled testing performed by a firearms examiner at a crime laboratory.
High-velocity bullets with jackets and lead cores generally break up into hundreds of fragments, called a “lead snowstorm,” on entering tissue, resulting in significant tissue damage (Fig. 65-17).41 If the tissue they penetrate is deep, the bullet fragments may fail to exit and remain embedded. It is therefore possible to sustain an injury from a high-velocity round and not exhibit an exit wound. High-velocity rounds with steel cores will almost uniformly exit intact.
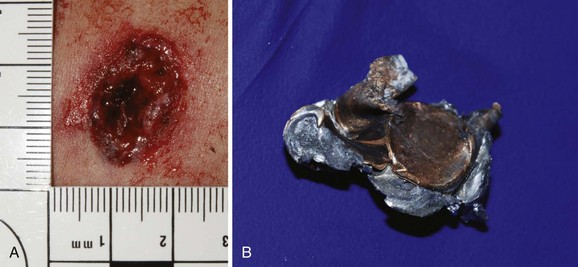
Forensic Evaluation of Shotgun Wounds.: Shotguns, have the barrel length of rifles, but can discharge pellets or single slugs down a smoothbore barrel. The caliber of a shotgun is defined by the term gauge. Historically, the gauge of a gun referred to “the number of lead balls of the given bore diameter that make up a pound”—for example, 12 lead balls to make 1 lb.41 A shotgun cartridge may contain only a single slug or may contain hundreds of pellets (Fig. 65-18A). Pellets range in diameter from 0.05 inch (#12 birdshot) to 0.36 inch (“000” buckshot). A shotgun cartridge is made of several components that will be of forensic value and should be collected in the ED (Fig. 65-18B).
Shotgun slugs are single projectiles that may weigh 200 times more than handgun ammunition—for example, a 12-gauge slug weighs 547 grams, and a .22 long rifle bullet weighs 2.6 grams (see Fig. 65-18B). The massive damage caused by slugs may obliterate the abrasion collar usually associated with entrance wounds. Shotgun slugs will almost uniformly exit the body with large exit wounds. The velocities of shotgun slugs are in the range of 1500 to 1800 ft/s.
Microscopic Examination of Wounds
The débrided epithelial margins of wounds should be submitted to the pathology department for a histologic examination. The microscopic presence of soot, gunpowder, and thermal damaged will help determine if the wound is an entrance or exit wound and the range of fire.58–60
Evidence
A victim’s clothing may yield information about a bullet’s range of fire and help distinguish entrance from exit wounds.* Clothing fibers will deform in the direction of the passing projectile.41,56 Gunpowder residues and soot will deposit on clothing as they do on skin. Residue may be invisible to the naked eye, but nitrites and vaporized lead can be visualized with standard forensic staining techniques. Some bullets, as they make initial contact with clothing, leave a lead or lubricant residue that is termed bullet wipe. Articles of clothing removed from a wounded patient need to be placed in separate paper bags to avoid cross-contamination of evidence.11,17
A gunshot residue (GSR) test may determine whether a victim or suspect has been in proximity to a weapon that has been discharged.41,61–70 The GSR test checks for the presence of invisible residues from the primer: barium nitrate, antimony sulfide, and lead peroxide. The presence of residue can be checked by (1) swabbing the palms and the dorsum of the hands with a 5% nitric acid solution and then analyzing the swabbed contents with atomic absorption spectrophotometry or (2) placing tape or an adhesive disk on the hands and then removing it for examination under a scanning electron microscope.
The specificity and sensitivity of the GSR test are unclear.41,61,69,70 Residue will deposit on the hands of the individual who fired the weapon in only 50% of cases.41 Residue may spread throughout a crime scene, and secondary contact with the weapon or furniture on which residue was deposited will result in a false-positive test result. The transference of residue from police officers to suspects has also been reported.70 The sensitivity of the test decreases with time, and law enforcement agents may not have access to a patient during the “golden hour.”41 Actions that decrease sensitivity include washing the skin with alcohol or betadine, placing tape on the skin, rubbing the hands against clothing, and placing plastic bags over the patient’s hands, which precipitates moisture on the skin. If a GSR test is to be performed or if soot is noted on the patient’s hand, paper bags should be placed over the hands early in the treatment.
The bullet, the bullet jacket, and the cartridge case are invaluable for identifying or excluding a suspect weapon.40,41 When a weapon is discharged, the discharge imprints multiple microscopic marks on the side of a bullet and on the bottom or side of the cartridge case.40,41 The markings result from the bullet’s contact with the tool marks or “rifling” in the gun’s barrel. These marks are unique to each barrel and are reproducible. These marks are the gun’s “fingerprint,” so to speak. Cartridge case marks are from contact with the firing pin, the breech lock, the magazine of semiautomatic weapons, and extractor and ejector mechanisms. These microscopic “fingerprints” can be obliterated by removing a bullet with hemostats or pickups.11,17,41 Bullets should be handled with gloves, and the tips of surgical instruments should be covered with gauze (Figs. 65-19 and 65-20) or plastic tips—”suture booties”—to ensure the preservation of these microscopic marks. It is not necessary to place initials or other markings on the bullet if adequate notes are made in the patient’s medical record regarding the chain of custody.11,17
Radiographs also help locate retained projectiles and may be of evidentiary value in determining the number of projectiles and the direction of fire.39–41,71
Forensic Aspects of Physical Assault
Studies estimate that up to 22 to 33% of patients in urban EDs are victims of domestic violence, yet very few are recognized as such.28,72–85 In a study of victims of domestic violence, 43% of patients with acute trauma came to the ED six or more times before they were identified as victims of abuse; nearly half of these patients came to the ED at least 12 times.84 Victims admitted to the trauma service also go unrecognized.85
Every weapon leaves a mark, design, or pattern stamped or imprinted on or just below the epithelium. The epithelial imprints of these weapons, called pattern injuries, are consistently reproducible.19,25,35,86 These injuries are classified into three major categories according to their source: blunt force, sharp force, and thermal.
Blunt Force Pattern Injuries
The most common blunt force injury is the contusion, along with abrasions and lacerations. A weapon with a unique shape or configuration may stamp a mirror image of itself on the skin (Box 65-1).19,35,86
Pattern Contusions.: A blow from a linear object leaves a contusion that is characterized by a set of parallel lines separated by an area of central clearing (Fig. 65-21).19,35,86 The blood underlying the striking object is forcibly displaced to the sides, which accounts for the pattern’s appearance (Fig. 65-22).

Figure 65-22 Pattern contusion with parallel lines and central clearing from contact with a baseball bat.
Circular or linear contusions suggest abuse or battery. Circular contusions 1.0 to 1.5 cm in diameter are consistent with fingertip pressure and grab marks (Fig. 65-23). One commonly overlooked anatomic location for fingertip pressure contusions is the medial aspect of the upper arm.35,86 The sole of a shoe from a kick or stomp may also leave a pattern contusion that can assist in identifying the assailant (Fig. 65-24).
Some injuries allegedly occur during police custody. Specific pattern contusions can include parallel contusions from a flashlight or nightstick. Handcuff or shackle marks are narrow parallel contusions or abrasions on the wrists or ankles. Handcuff and shackle marks are generally more prominent on the lateral aspects of the extremity.42
A bite mark may appear as a pattern contusion, an abrasion, or a combination of both (Fig. 65-25). Bite marks vary greatly in the quality of their identifiable features, depending on the location of the bite and the motion of the teeth relative to the skin. Some bite marks may not be readily identifiable as such and may appear as nonspecific contusions, abrasions, or contused abrasions.
When an acute bite mark is identified, care should be taken not to wash away potential evidence. The skin surface should be swabbed with a sterile cotton-tipped applicator moistened with sterile saline. DNA from buccal cells may also be deposited over an acute bite mark.11,17
When available, a forensic odontologist can evaluate a bite wound with accuracy. The use of alternative light sources, such as ultraviolet or infrared, may reveal a pattern contusion within or under the epithelium that is not visible to the naked eye.87 These light sources are routinely used by the forensic odontologist on bite marks that are faint, old, or difficult to identify.
The emergency physician may be asked to render an opinion regarding the age of a contusion. The development of a contusion is based on a number of variables: the amount of blunt force applied to the skin, the vascularity of the tissue, the oxygenation of the extravasated hemoglobin, the depth of the hematoma, skin tone, and the amount of blood that escapes into the surrounding tissue.88–90 As a result, no reproducible standard for the dating of a contusion is possible based on its color.88–90 New techniques based on reflectance spectrophotometry are currently being tested.91 A tissue biopsy examining the hemosiderin breakdown may be the only scientifically accepted method to determine the approximate age of a contusion.92
Pattern Abrasions and Lacerations.: A pattern abrasion is a rubbing or scraping away of the superficial layers of the epidermis, which is not important for treatment but may be invaluable from a forensic and injury reconstruction perspective.86
A laceration is defined as a tear in the skin produced by blunt trauma and should not be confused with an incised wound produced when a sharp-edged implement (e.g., knife, scalpel, or piece of glass) is drawn across the skin.19,35 A laceration has characteristically abraded or crushed skin edges and unique “tissue bridges” (Fig. 65-26).
Sharp Force Pattern Injuries
Forensic information can be gathered during the examination of a stab wound. Some of the characteristics of a knife blade, single edged or double edged, can be determined from visual inspection (Fig. 65-27A and B).19,86 Additional blade characteristics, such as serrated versus sharp, can be seen if the blade was drawn across the skin during its insertion or withdrawal (see Fig. 65-27C). Serrated blades do not always leave characteristic marks.19,86
When a patient claims to have been assaulted and the victim of a crime, his or her injuries become physical evidence. It is important for the treating physician, who may be called as an expert witness, to recognize patterns of self-inflicted injury to distinguish self-inflicted wounds from those sustained during an assault (Fig. 65-28 and Box 65-2).
Thermal Pattern Injuries
A thermal pattern injury is a common form of abuse or battery. The history should include the position of the patient relative to the thermal source. This information will help determine whether the injury was intentional or accidental.86
The severity of thermal or scald injury depends on the length of contact time and the temperature. Water causes full-thickness damage in 1 second at 158° F (70° C) and in 600 seconds at 120° F (48.9° C) (Fig. 65-29).93 Law enforcement routinely measures the household’s or institution’s water temperature in any investigation involving a scald injury.
Forensic Aspects of Motor Vehicle Trauma
Law enforcement officials investigating an incident involving serious or fatal injuries from a motor vehicle or pedestrian collision may benefit from information regarding injury patterns and the collection of trace evidence from the victim. This information can help determine whether an occupant was a driver or passenger. It may help to identify a suspect vehicle involved in a hit-and-run pedestrian collision or a pedestrian’s position (standing or lying) when struck in the roadway.42
Determination of a vehicle occupant’s role may be simple (e.g., if the driver is pinned behind the steering wheel) or complex (e.g., if the vehicle’s occupants are ejected). Many impaired drivers claim to be passengers. Short-lived evidence or pattern injuries that might be destroyed or altered in the delivery of patient care should optimally be preserved and photographed.94,95
An opinion on an occupant’s position should be avoided because an occupants’ role is difficult to determine based solely on the statements and physical findings in the ED.94,95 Such an opinion is best rendered by someone who has examined the scene, the vehicle, other occupants, and trace evidence; has reviewed postmortem examinations; and has had the collision reconstructed to determine vehicle dynamics (Box 65-3).94–96
Pattern Injuries
Matching pattern injuries with components within a vehicle often reveals an occupant’s position during a portion of the vehicle’s collision sequence.94–96 Common pattern contusions, abrasions, and lacerations are seen from steering wheels, air bags, air bag module covers, window cranks, radio knobs, door latches, dashboard components, and front and side window glass.94–98 An occupant’s movement and subsequent contact with a vehicle’s components are dictated by the forces applied to the vehicle through its interaction with the environment. Vehicle occupants, restrained or unrestrained, will initially move toward the primary area of impact.94 Movement within the vehicle is called occupant kinematics. Occupant movement toward the primary area of impact is described as a motion parallel and opposite to the principal direction of the force (PDOF) developed by the impacting object.94,95 The PDOF will predict the direction in which a particular occupant will move and therefore what component within the vehicle may be struck.
A deploying air bag may induce a pattern abrasion to the face, cornea, forearms, or other exposed tissue. Pattern lacerations, specific fracture patterns, and amputations are seen when the deploying air bag module cover impacts the hand or forearm (Fig. 65-30).97,98 The correlation of these injuries and the transfer of DNA from the driver or passenger to the deployed air bag are helpful in assessing an occupant’s role as driver or passenger.97,98

Figure 65-30 A traumatic partial amputation of the hand resulted from contact with a deploying air bag module cover.
Laminated glass (windshields) and tempered glass (side and rear windows) produce pattern injuries. The windshield has two layers of glass laminated together with a thin layer of clear plastic sandwiched between. Laminated glass breaks into shards on impact and causes linear incised wounds. Tempered or safety glass is a single layer of glass that breaks into small cubes when fractured, imparting a “dicing” pattern to the skin (Fig. 65-31).42,94,95
Trace Evidence
Clothing, shoes, and biologic standards (hair, tissue, and blood) may determine an occupant’s role.95–99 The soles of leather shoes may reveal the imprint of the gas or brake pedal (Fig. 65-32). Preservation of clothing permits the comparison of clothing fibers with those fibers transferred to vehicle components during the collision.95–99 Imprints of fabric may also be transferred to components within the vehicle, including the steering wheel. Contact with the windshield often transfers hair and tissue to the glass. Glass collected from within a patient’s wound can be matched with a particular window within the vehicle. Airbags can be an excellent source of trace evidence. Examples of transferred evidence include skin, blood, makeup, and hair (Fig. 65-33).97,98
Evaluation of Pedestrian Collisions
Approximately 59,000 people were killed or seriously injured in pedestrian collisions in 2009100; 87% are struck by a vehicle’s front bumper or grill area.100 When struck by the front of a vehicle, a standing adult will sustain “bumper injuries,” which include open and closed fractures of the tibia and fibula, soft tissue damage, and pattern injuries from vehicle components and hardware.42
A victim who is struck from behind may have pattern contusions on the calf or thigh (Fig. 65-34), whereas pattern contusions from a grill on the anterior aspect of the thigh indicate the pedestrian was standing and facing the vehicle. Pedestrians struck by a glancing portion of a vehicle may also display a pattern injury (Fig. 65-35). Victims who are run over may display a tire tread pattern (Fig. 65-36). Tire marks and the absence of bumper injuries suggest that the patient was supine or prone in the roadway before he or she was run over (Box 65-4).
Law Enforcement Exemptions to the Health Insurance Portability and Accountability Act
Title 45 Part 164 of the Health Insurance Portability and Accountability Act (HIPAA) of 1996 permits hospitals to disclose, without patient consent, to investigating law enforcement agencies specific information regarding a victim or suspect. Section 45 CFR 164.512 permits the release of protected health information, without a court order, “in response to a law enforcement official’s request for such information for the purpose of identifying or locating a suspect, fugitive, material witness, or missing person.”101 A hospital or physician may disclose the information listed in Box 65-5 only to an investigating law enforcement officer.
References
1. Doney, IV. Police surgeons of the United Kingdom. Am J Forensic Med Pathol. 1984;5:185.
2. McLay, WDS. Clinical Forensic Medicine. London: Pinter; 1990.
3. Eckert, W. The development of forensic medicine in the United Kingdom from the 18th century. Am J Forensic Med Pathol. 1992;13:124.
4. Payne-James, JJ, Dean, PJ. Assault and injury in clinical forensic medical practice. Med Sci Law. 1994;34:202.
5. Beran, RG. The teaching of legal medicine in Australasia. J Forensic Leg Med. 2007;14:284–288.
6. Goldsmith, MF. U.S. forensic pathologists on a new case: Examination of living patients. JAMA. 1986;256:1685.
7. Smialek, JE. Forensic medicine in the emergency department. Emerg Med Clin North Am. 1983;1:1685.
8. Carmona, R, Prince, K. Trauma and forensic medicine. J Trauma. 1989;29:1222.
9. Ryan, MT. Clinical forensic medicine. Ann Emerg Med. 2000;36:271.
10. Wiler, JL, Bailey, H, Madsen, TE. The need for emergency medicine resident training in forensic medicine. Ann Emerg Med. 2007;50:733.
11. Eisert, PJ, et al. Development of forensic evidence collection guidelines for the emergency department. Crit Care Nurs Q. 2010;33:190.
12. Sharma, BR. Clinical forensic medicine—management of crime victims from trauma to trial. J Clin Forensic Med. 2003;10:267.
13. Smock, WS, Nichols, GR, Fuller, PM. Development and implementation of the first clinical forensic medicine training program. J Forensic Sci. 1993;38:835.
14. Smock, WS. Development of a clinical forensic medicine curriculum for emergency physicians in the USA. J Clin Forensic Med. 1994;1:27.
15. Smock, WS, Ross, CS, Hamilton, FN. Clinical forensic medicine: How ED physicians can help with the sleuthing. Emerg Legal Brief. 1994;5:1.
16. Eckert, WG, et al. Clinical forensic medicine. Am J Forensic Med Pathol. 1986;7:182.
17. Wick, JM. Don’t destroy the evidence!. AORN J. 2000;72:807.
18. Godley, DR, Smith, TK. Some medicolegal aspects of gunshot wounds. J Trauma. 1977;17:866.
19. Smock, WS. Forensic aspects of motor vehicle trauma. In: Olhaker JS, Jackson MC, Smock WS, eds. Forensic Emergency Medicine. 2nd ed. Philadelphia: Lippincott: Williams & Wilkins; 2006:72–84.
20. Busuttil, A, Smock, WS. Training in clinical forensic medicine in Kentucky. Police Surg. 1990;14:26.
21. The Joint Commission, Hospital Accreditation Standards. 2009.
22. Berger, N, Jones, J, Smock, WS. Clinical forensic medicine. In: The Medical Student Survival Guide. Dallas: Emergency Medicine Resident’s Association; 2007:166–168.
23. New forensic medicine section being formed. EM Today. www.acep.org, 2006.
24. Wade C, ed. FBI Forensic Sciences Handbook. Quantico, Va: Federal Bureau of Investigation, 2003.
25. Smock, WS. Forensic photography. In: Stack LB, Storrow AB, Morris A, Patton DR, eds. Handbook of Medical Photography. Philadelphia: Hanley & Belfus; 2001:397–408.
26. Stark, MM, Norfolk, GA. Training in clinical forensic medicine in the UK—perceptions of current regulatory standards. J Forensic Leg Med. 2011;18:264.
27. Collins, KA, Lantz, PE. Interpretation of fatal, multiple, and exiting gunshot wounds by trauma specialists. J Forensic Sci. 1994;39:94.
28. McLeer, SV, Anwar, RA, Herman, S, Maquiling, K. Education is not enough: A systems failure in protecting battered women. Ann Emerg Med. 1989;18:651.
29. Breo, DL. JFK’s death: The plain truth from the MDs who did the autopsy. JAMA. 1992;267:2794.
30. Randall, T. Clinicians’ forensic interpretations of fatal gunshot wounds often miss the mark. JAMA. 1993;269:2058.
31. Centers for Disease, Control and Prevention (CDC): Deaths: Preliminary data for 2009. Natl Vital Stat Rep 2011;Vol. 59:No. 4. http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_04.pdf.
32. Centers for Disease. Control and Prevention (CDC): Surveillance for fatal and nonfatal firearm-related injuries—United States, 1993-1998. MMWR CDC Surveill Summ. 2001;50:1.
33. Corso, PS, Mercy, JA, Simon, TR, Finkelstein, EA, Miller, TR. Medical costs and productivity losses due to interpersonal and self-directed violence in the United States. Am J Prev Med. 2007;32:474.
34. Dana, SE, DiMaio, VJM. Gunshot trauma. In: Payne-James J, Busuttil A, Smock W, eds. Forensic Medicine: Clinical and Pathological Aspects. London: Greenwich Medical Media; 2003:149–168.
35. Smock, WS. Forensic medicine: Pattern injuries of domestic violence, assault and abuse. In: Knoop KH, Stack LB, Storrow AB, eds. Atlas of Emergency Medicine. 2nd ed. New York: McGraw-Hill; 2002:565–576.
36. Marlowe, AL, Smock, WS. The forensic evaluation of gunshot wounds by prehospital personnel. Proc Am Acad Forensic Sci. 1996;2:149.
37. Fackler, ML, Riddic, KL. Clinicians’ inadequate descriptions of gunshot wounds obstruct justice: Clinical journals refuse to expose the problem. Proc Am Acad Forensic Sci. 1996;2:150.
38. DiMaio, VJM, Spitz, WU. Variations in wounding due to unusual firearms and recently available ammunition. J Forensic Sci. 1972;17:377.
39. Fackler, ML. Wound ballistics: A review of common misconceptions. JAMA. 1988;259:2730.
40. Fatteh, A. Medicolegal Investigation of Gunshot Wounds. Philadelphia: Lippincott; 1976.
41. DiMaio, VJM. Gunshot Wounds, 2nd ed. Boca Raton, Fla: CRC Press; 1999.
42. Spitz, WU. Medicolegal Investigation of Death, 4th ed. Springfield, Ill: Charles C Thomas; 2006.
43. Apfelbaum, JD, Shockley, LW, Wahe, JW, Moore, EE. Entrance and exit gunshot wounds: Incorrect terms for the emergency department? J Emerg Med. 1998;16:741.
44. Breo, DL. JFK’s death: Part II—Dallas MDs recall their memories. JAMA. 1992;267:2791.
45. Sellier, KG, Kneubuehl, BP. Wound Ballistics and the Scientific Background. Amsterdam: Elsevier; 1994.
46. Le Garde, LA. Gunshot Injuries, 2nd rev ed. Mt Ida, Ark: Lancer Militaria; 1991.
47. Lindsey, D. The idolatry of velocity, or lies, damn lies, and ballistics. J Trauma. 1980;20:1068.
48. Lindsey, D. Review of Management of Gunshot Wounds by Ordog. Am J Emerg Med. 1989;7:117.
49. Fackler, ML. Review of Management of Gunshot Wounds by Ordog. Ann Emerg Med. 1988;17:1004.
50. Barach, EM, Tomlanovich, MC. Civilian gunshot wounds: determinants of injury. J Trauma. 1988;28:1610.
51. Mason, JK. The Pathology of Trauma, 2nd ed. London: Hodder & Stoughton; 1993.
52. Dixon, DS. Tempered plate glass as an intermediate target and its effects on gunshot wound characteristics. J Forensic Sci. 1982;27:205.
53. Stahl, CJ, et al. The effect of glass as an intermediate target on bullets: Experimental studies and report of a case. J Forensic Sci. 1979;24:6.
54. Donoghue, ER, Kalelkar, MB, Richmond, JM, Teas, SS. Atypical gunshot wounds of entrance: An empirical study. J Forensic Sci. 1984;29:379.
55. Dixon, DS. Determination of direction of fire from graze gunshot wounds. J Forensic Sci. 1980;25:272.
56. Dixon, DS. Determination of direction of fire from graze gunshot wounds of internal organs. J Forensic Sci. 1984;29:331.
57. Dixon, DS. Characteristics of shored exit wounds. J Forensic Sci. 1981;26:691.
58. Adelson, L. A microscopic study of dermal gunshot wounds. Am J Clin Pathol. 1961;35:393.
59. Murphy, GK. The study of gunshot wounds in surgical pathology. Am J Forensic Med Pathol. 1980;1:123.
60. Torre, C, Varetto, L, Ricchiardi, P. New observations on cutaneous firearm wounds. Am J Forensic Med Pathol. 1986;7:186.
61. Lee, HC, Palmbach, T, Miller, MT. Henry Lee’s Crime Scene Handbook. San Diego: Academic Press; 2001.
62. Molina, DK, Martinez, M, Garcia, J, DiMaio, VJ. Gunshot residue testing in suicides. Part I: Analysis by scanning electron microscopy with energy-dispersive x-ray. Am J Forensic Med Pathol. 2007;28:187.
63. Molina, DK, Martinez, M, Garcia, J, DiMaio, VJ. Gunshot residue testing in suicides. Part II: Analysis by inductive coupled plasma-atomic emission spectrometry. Am J Forensic Med Pathol. 2007;28:191.
64. Adeyl, O, Duval, JV, Dupre, ME, Andrew, TA. Role of chemical tests and scene investigation in determination of range of fire. Am J Forensic Med Pathol. 2005;26:166.
65. Santos, A, Magalhaes, T, Vieira, DN, Almeida, AA. Firing distance estimation through the analysis of the gunshot residue deposit pattern around the bullet entrance hole by inductively coupled plasma-mass spectrometry: An experimental study. Am J Forensic Med Pathol. 2007;28:24.
66. Tillman, J. Automated gunshot residue particle search and characterization. J Forensic Sci. 1987;32:62.
67. Kee, TG, Beck, C. Casework assessment of an automated scanning electron microscope/microanalysis system for the detection of firearms discharge particles. J Forensic Sci Soc. 1987;27:321.
68. Zeichner, A, Levin, N. Casework experience of GSR detection in Israel, on samples from hands, hair, and clothing using an autosearch SEM/EDX system. J Forensic Sci. 1995;40:1082.
69. Zoja, R, Lazzaro, A, Battistine, A, Gentile, G. Detection of gunshot residues on cadaveric skin using sodium rhodizonate and a counterstain. Biotech Histochem. 2006;81:151.
70. Gialamas, DM, et al. Officers, their weapons and their hands: An empirical study of GSR on the hands of non-shooting police officers. J Forensic Sci. 1995;40:1086.
71. Dixon, DS. Gunshot wounds: Forensic implications in a surgical practice. In: Ordog GJ, ed. Management of Gunshot Wounds. New York: Elsevier, 1988.
72. Kothari, C, Rhodes, KV. Missed opportunities: Emergency department visits by police-identified victims of intimate partner violence. Ann Emerg Med. 2006;47:190.
73. Tilden, VP. Response of the health care delivery system to battered women. Issues Ment Health Nurs. 1989;10:309.
74. Randall, T. Domestic violence intervention calls for more than treating injuries. JAMA. 1990;254:939.
75. McLeer, SV, Anwar, RA. The role of the emergency physician in the prevention of domestic violence. Ann Emerg Med. 1987;16:1155.
76. Morrison, LJ. The battering syndrome: A poor record of detection in the emergency department. J Emerg Med. 1988;6:521.
77. Tilden, VP, Shepherd, P. Increasing the rate of identification of battered women in an emergency department: Use of a nursing protocol. Res Nurs Health. 1987;10:209.
78. Goldberg, W, Carey, AL. Domestic violence victims in the emergency setting. Top Emerg Med. 1982;3:65.
79. Delahunta, EA. Hidden trauma: The most missed diagnosis of domestic violence. Am J Emerg Med. 1995;13:74.
80. Grunfeld, AF, Ritmiller, S, Mackay, K, Cowan, L, Hotch, D. Detecting domestic violence against women in the emergency department: A nursing triage model. J Emerg Nurs. 1994;20:271.
81. Isaac, NE, Sanches, RL. Emergency department response to battered women in Massachusetts. Ann Emerg Med. 1994;23:85.
82. Abbott, J, Johnson, R, Koziol-McLain, J, Lowenstein, SR. Domestic violence against women: Incidence and prevalence in an emergency department population. JAMA. 1995;273:1763.
83. Gremillion, DH, Evins, G. Why don’t doctors identify and refer victims of domestic violence? N C Med J. 1994;55:428.
84. Davis, JW, Parks, SN, Kaups, KL, Bennink, LD, Bilello, JF. Victims of domestic violence on the trauma service: Unrecognized and underreported. J Trauma. 2003;54:352.
85. Chambliss, LR, Bay, RC, Jones, RF. Domestic violence: An educational imperative? Am J Obstet Gynecol. 1995;172:1035.
86. Smock, WS. Recognition of pattern injuries in domestic violence victims. In: Siegel JA, Saukko PJ, Knupfer GC, eds. Encyclopedia of Forensic Sciences. San Diego: Academic Press; 2000:384–390.
87. Patno, K, Jenny, C. Who slapped that child? Child Maltreat. 2008;13:298.
88. Maguire, S, Mann, MK, Sibert, J, Kemp, A. Can you age bruises accurately in children? A systemic review. Arch Dis Child. 2005;90:187.
89. Bariciak, ED, Plint, AC, Gaboury, I, Bennett, S. Dating of bruises in children: An assessment of physician accuracy. Pediatrics. 2003;112:804.
90. Dimitrova, T, Georgieva, L, Pattichis, C, Neofytou, M. Qualitative visual image analysis of bruise age determination: A survey. Conf Proc IEEE. Eng Med Biol Sci. 2006;1:4840.
91. Hughes, VK, Langious, NE. Use of reflectance spectrophotometry and colorimetry in a general linear model for the determination of the age of bruises. Forensic Sci Med Pathol. 2010;6:275.
92. Vanezis, P. Interpreting bruises at necropsy. J Clin Pathol. 2001;54:348.
93. Katcher, ML. Scald burns from hot tap water. JAMA. 1981;246:1219.
94. Smock, WS, Nichols, GR, 2nd., Fuller, PM, Weakley-Jones, B. The forensic pathologist and the determination of driver versus passenger in motor vehicle collisions. Am J Forensic Med Pathol. 1989;10:105.
95. Smock, WS. Driver versus passenger in motor vehicle collisions. In: Siegel JA, Saukko PJ, Knupfer GC, eds. Encyclopedia of Forensic Sciences. San Diego: Academic Press; 2000:24–32.
96. Blackbourne, BD. Injury-vehicle correlations in the investigation of motor vehicle accidents. In: Wecht CH, ed. Legal Medicine Annual 1980. New York: Appleton-Century-Crofts; 1980:1–19.
97. Smock, WS, Nichols, GR. Airbag module cover injuries. J Trauma. 1995;38:489.
98. Smock, WS. Airbag related injuries and deaths. In: Siegel JA, Saukko PJ, Knupfer GC, eds. Encyclopedia of Forensic Sciences. San Diego: Academic Press; 2000:1–8.
99. Laing, DK, et al. A fiber data collection for forensic scientists: Collection and examination methods. J Forensic Sci. 1987;32:364.
100. National Highway Traffic Safety Administration. Traffic Safety Facts 2009. Washington, DC: Department of Transportation; 2010.
101. Department of Health and Human Services. Health Insurance Portability and Accountability Act of 1996 (HIPPA), Title 45, Part 164, Subpart E, § 164.512. http://edocket.access.gpo.gov/cfr_2002/octqtr/45cfr164.512.htm.