Vaginal Bleeding
Perspective
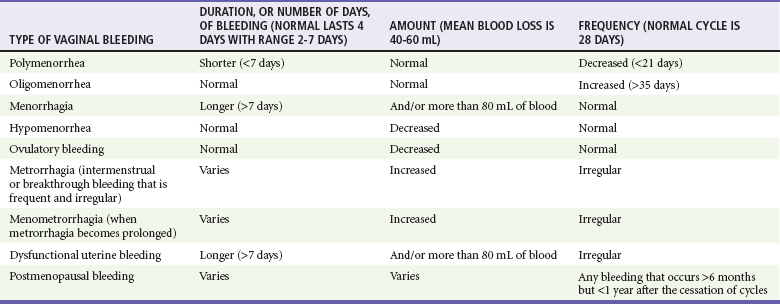
Vaginal bleeding includes uterine and extrauterine causes. Uterine causes include the constellation of normal uterine bleeding, abnormal uterine bleeding, and dysfunctional uterine bleeding, which is abnormal uterine bleeding in the absence of organic disease. Normal menstrual bleeding occurs cyclically in women who have achieved menarche (the onset of menses), mean age 12.5 years, until menopause (the cessation of menses), mean age 51 years, in North America. The normal cycle, defined as the first day of bleeding of one cycle to the first day of bleeding of the next cycle, lasts 28 days, plus or minus 7 days, and the average volume of blood loss is 60 mL. Vaginal bleeding is defined temporally as midcycle (ovulatory, or at the release of an ova), premenstrual, menstrual, and postmenstrual. Abnormal vaginal bleeding is classified on the basis of the duration, amount, and frequency of bleeding (Table 34-1). Abnormal vaginal bleeding occurs in women of all ages, and it can result from a number of causes, including anatomic abnormalities, complications of pregnancy, hematologic disorders, infections, malignancies, medications, obesity, systemic diseases, and endocrinologic imbalances. Premenarchal or postmenopausal vaginal bleeding is rarely life-threatening, but bleeding as a complication of pregnancy has a significantly increased risk of morbidity and mortality for the mother and fetus1,2 (see Chapter 178).
Epidemiology
Approximately 5% of women aged 30 to 45 years will see a physician for vaginal bleeding annually. Menorrhagia (regular heavy bleeding) secondary to anovulation is seen in 10 to 15% of all gynecologic patients. Excessive menstrual bleeding accounts for two thirds of all hysterectomies and most endoscopic endometrial destructive surgery. The consequences of menorrhagia include anemia and iron deficiency, reduced quality of life, and increased health care costs.3 Because black women are more likely to have leiomyomas (fibroids), they experience disproportionately more morbidity from menorrhagia. Invasive neoplasms of the female pelvic organs account for almost 15% of all cancers in women. The most common of these malignancies is uterine cancer, specifically, endometrial cancer. Approximately 10% of postmenopausal bleeding is eventually diagnosed as endometrial cancer. Endometrial cancer is associated with obesity, diabetes mellitus, anovulatory cycles, nulliparity, and age older than 35 years. Both squamous cell carcinoma and adenocarcinoma of the cervix are causally related to infection with the human papillomavirus (HPV), especially types 16 and 18. Smoking and possible dietary factors, such as decreased circulating vitamin A, appear to be cofactors. Preinvasive cancer (cervical intraepithelial neoplasia [CIN III]) is a common diagnosis in women 25 to 40 years of age.
Pregnant Patients
Vaginal bleeding after the 20th week of gestation occurs in approximately 4% of pregnancies; approximately 30% of cases are caused by placental abruption (abruptio placentae), and 20% are caused by placenta previa. The most common cause of postpartum hemorrhage in the first 24 hours is uterine atony, but after 24 hours the presence of retained products of conception is the more frequent cause.4
Pathophysiology
Causes of vaginal bleeding in nonpregnant women are classified as ovulatory, anovulatory, and nonuterine. Ovulation bleeding, a single episode of spotting between regular menses, is quite common. Approximately 90% of dysfunctional uterine bleeding cases result from anovulation, and the other 10% of cases occur with ovulatory cycles. When ovulation does not occur, there is overgrowth of the endometrium because of estrogen stimulation without progesterone to stabilize growth. This results in a persistent proliferative endometrium. Patients at the extremes of menarche are more likely to have endocrinologic causes of disruption of the hypothalamic-pituitary-ovarian system resulting in anovulation. In addition, disruption of this axis is seen with excessive stress, weight loss, and exercise. Bleeding outside the uterus also is considered, including lesions of the vulva, vagina, or cervix, as well as uterine tumors, adnexal masses, and urethral, rectal, and anal disorders.5 Prepubertal female children may have foreign bodies, genital trauma, or severe vulvovaginitis causing mucosal breakdown and hemorrhage. Exogenous hormone use, most commonly in progesterone-only oral contraceptives and in intrauterine devices, is very common in reproductive-age women. Leiomyomas (fibroids) cause hemorrhage by disrupting the endometrial vascular supply and the ability of the uterus to contract to stop bleeding. Cervical and endometrial polyps have vascular pedicles and are prone to bleed.
Pregnant Patients
The differential diagnosis of vaginal bleeding in early pregnancy (before the 20th week of gestation) includes ectopic pregnancy; spontaneous, threatened, complete, incomplete, inevitable, missed, or infected (septic) abortions; implantation bleeding; cervicitis; cervical conditions such as polyp or ectropion; bleeding from the urinary or gastrointestinal tract; trauma and cervical carcinoma; and gestational trophoblastic disease (hydatidiform mole, molar pregnancy). Risk factors for ectopic pregnancy include tubal abnormalities caused by past infection, surgical scarring, or assisted reproductive techniques. Disruption of the blood supply to the ectopic gestational sac can cause hemorrhage into the fallopian tube, or the size of the developing fetus can lead to rupture through the tubal wall.6,7 Life-threatening vaginal bleeding after the first trimester is often a result of placental abruption. This can occur spontaneously or secondary to abdominal trauma with transmission of forces to the uterus. An increased incidence is seen in association with cocaine use, hypertension, preeclampsia, HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome, smoking, increased maternal age, and abnormal implantation of the placenta (e.g., placenta previa, accreta, increta, or percreta). Placenta previa occurs when the implanted placenta overlays the cervical os. Bleeding is caused by partial separation of the placenta from the uterine wall. Postpartum uterine atony occurs when myometrial dysfunction prevents the uterine corpus from contracting, allowing continued bleeding at the placental site. Atony is more likely to occur with conditions that overdistend the uterus, such as polyhydramnios, multiparity, prolonged labor, induced labor, high Pitocin use during labor, precipitous labor, magnesium therapy, or intrauterine infection (chorioamnionitis).8 Complications of pregnancy, including vaginal bleeding, are discussed in Chapter 178.
Diagnostic Approach
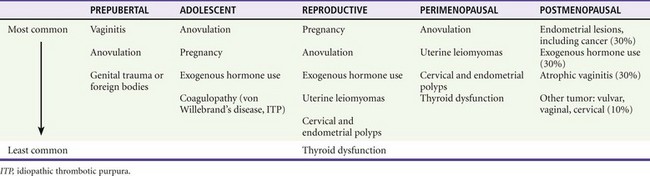
The differential diagnosis can be categorized by age of presentation and frequency of cause (Table 34-2). Primary coagulation disorders account for almost 20% of acute menorrhagia in adolescents. Von Willebrand’s disease is the most common; however, myeloproliferative disorders and immune thrombocytopenia are also possibilities.9 Ectopic pregnancy should be considered in all women of childbearing age with abdominal or pelvic complaints or with unexplained signs or symptoms of hypovolemia. Additional uterine disorders include endometrial cancer, endometriosis, leiomyomata, adenomas, and sarcomas.