Chapter 60 Transplantation of Organs
Rehabilitation to Maximize Outcomes
Historical Success and Rehabilitation Options
As the volume of organ transplants performed each year surges and the types of transplants become diversified, there is an increasing need for proper rehabilitation care for transplant recipients (Figure 60-1).155 Functional restoration of persons who have undergone organ transplant surgery is an important priority of the physical medicine and rehabilitation team and has emerged as a global rehabilitation priority.113 Just as transplantation surgery can add years to life, transplant rehabilitation can add life to years.
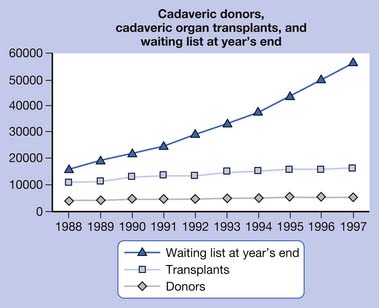
FIGURE 60-1 Cadaveric donors, cadaveric organ transplants, and waiting list at year’s end
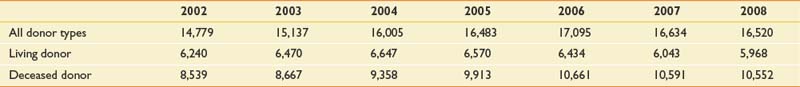
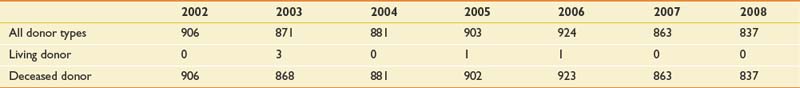
(From http://optn.transplant.hrsa.gov/latestData/rptData.asp; and http://www.ustransplant.org/annual_reports/current/103_dh.htm.)
The rapidly evolving, innovative methods of preventing or minimizing organ transplant-related infection and rejection have resulted in improved survivorship among organ transplant recipients.1 The availability of more potent immunosuppressive drugs with reduced side effects has significantly improved health outcomes and enabled patients to be transferred earlier to the acute rehabilitation unit.125 The preemptive application of acute immunosuppressive therapies, such as monoclonal and polyclonal antibodies, has facilitated successful organ transplantation surgery and subsequent rehabilitation functional restoration.44 Ongoing developments in the science of human leukocyte antigen (HLA) matching and the perfection of the HLA Registry process have considerably improved outcomes for bone marrow transplant recipients.59 Methods of transplanting end-stage renal disease (ESRD) patients by combining renal transplantation with perioperative bone marrow transplant (without the benefit of HLA matching and without maintenance immunosuppression) have recently been reported.68 Optimization of surgical technique has led to both an increase in the number of transplant surgeries performed annually, as well as an expansion in the diversity and complexity of these procedures. Prominent examples include the emergence of groundbreaking new transplantation procedures, including face transplant,37 multiple limb transplantation,38 and “domino organ transplants.”2 Many of these breakthroughs have sparked a surging demand for rehabilitation services. A renewal of academic interest in organ transplantation rehabilitation has resulted in a growing body of medical literature, including journal articles and book chapters dedicated to transplantation rehabilitation.114,155
Federal agencies in cooperation with the National Institute of Allergy and Infectious Diseases and the National Library of Medicine have established a unique public database containing results of blood and marrow stem cell transplants involving unrelated donors.48 This database is particularly useful to patients undergoing blood and marrow transplants and is accessible to physicians, researchers, and patients online at http://www.ncbi.nih.gov/mhc. This database includes fundamental demographic information such as gender, ethnicity, age, and genetic data on more than 1400 transplant donors and recipients worldwide, transplant recipient survival rates, as well as data on the relationship between transplantation and major histocompatibility complex genes. This latter information can assist doctors to better predict whether a recipient will “accept” or “reject” transplantation from a particular donor source. This novel resource promises to assist physicians in the evaluation of risks and benefits of transplantation for various clinical conditions. For the physiatrist providing preoperative/pretransplant consultative input, the data gleaned from this source can help predict outcomes and guide posttransplant rehabilitation.
Organ transplantation, despite its recognition as one of the “modern miracles” of contemporary medicine, is also fraught with many ethical and moral dilemmas. Choosing appropriate selection criteria is just one of the myriad philosophical issues present in organ transplantation.139 Despite the advances in organ transplantation medicine, an international crisis continues to loom in organ transplantation because the demand for organs radically outnumbers the available organ donors. (UNOS/OPTN unpublished data, 2010). This unmet need creates many ethical questions.21 National organizations within the United States such as the United Network for Organ Sharing (UNOS) and the Organ Procurement and Transplant Network (OPTN) exist to alleviate this exigency. OPTN is a private, not-for-profit, federally contracted transplant network established by the U.S. Congress under the National Organ Transplant Act of 1984 that united all the professionals involved in the transplantation and donation system. OPTN works to increase the effectiveness and efficiency of organ sharing as well as equalize the national system of organ allocation. A secondary goal is to increase the supply of donated organs available for transplantation. UNOS is responsible for administering the OPTN under contract with the Health Resources and Services Administration of the U.S. Department of Health and Human Services. Together UNOS and OPTN work collaboratively to establish organ transplantation policies and procedures. Assurance of positive functional outcomes posttransplantation remains a major goal. As a result of these efforts, physiatrists are likely to see a future surge in the number of transplantation patients seeking rehabilitation.
Chapter Focus
This chapter provides a general overview of the subject of organ transplantation and rehabilitation. Although solid organ transplantation rehabilitation is the primary focus, reference is made to recent developments in bone marrow and hematologic transplantation that have an impact on physiatry. A general background discussion of the relevance of physical medicine and rehabilitation to the transplantation process is offered. This is followed by a systematic consideration of rehabilitation principles and techniques that can improve patient outcome and quality of life. Of the more than 21 transplantable organ systems, this chapter will address the four most common ones seen in physiatric practice, that is, heart, lung, liver, and kidney. Special attention is also given to new frontiers in organ transplantation rehabilitation. Because transplant rehabilitation is such a nascent field, there is a scarcity of literature outlining the fundamental principles of the transplantation rehabilitation process.153
Physiatric Interventions in Enhancing Outcomes
Enhancement of quality of life is a primary goal of transplantation rehabilitation.155 Maintaining the physiatric spirit of “adding life to years as well as adding years to life” holds particular significance to rehabilitation of transplant survivors because these patients have often endured years of chronic end organ deterioration followed by prolonged organ waiting. The goal of transplant rehabilitation is to improve functional outcome and facilitate the return to a fulfilling life and lifestyle. Optimal physiatric management of a person who has survived transplantation requires a comprehensive, multidisciplinary, structured, and integrated approach.137
It is essential that a functional and medical baseline before surgery is established. The physiatric evaluation should include a comprehensive medical history and elaboration of functional deficits associated with end-stage organ damage. The physiatrist should conduct a thorough musculoskeletal, neurologic, and functional assessment of the patient (Box 60-1). Emphasis should be placed on the maintenance of bodily systems that are likely to be adversely affected by immobilization. This includes contracture prevention, deep vein thrombosis and pulmonary embolism preventive measures, skin maintenance, and preservation of bowel and bladder function. The prevention of disuse atrophy of major muscle groups can be addressed through bedside isometric exercise protocols. A therapeutic plan emphasizing exercise and remobilization should be developed and implemented that takes into account the patient’s presurgical functional status. As always, physiatrists must consider the psychosocial status of each patient and the impact the impairment will have on handicap and disability.130 Communication with other members of the transplant team is essential during each step of the process.
Close ongoing daily observation is essential after transplantation to ensure adequate immune system suppression, prevent opportunistic infection, and maintain rehabilitation goals.22 Emphasis should be placed on the underlying functional, medical, socioeconomic, and psychologic needs of the patient.98 The rehabilitation team should possess knowledge of the clinical aspects of acute and chronic rejection in all types of transplantation surgeries. Because transplant recipients typically present with a multitude of medical comorbidities, it is important to include any appropriate precautions in the rehabilitation plan. Careful consideration of exercise prescription should be made.26
The physiatrist must be aware of the side effects of the numerous medications used posttransplant. A summary of the side effects of some of the most frequently used immunosuppressive agents is provided in Table 60-1. See Table 60-2 for the monitoring parameters for immunosuppressive medication. Neuromusculoskeletal complications after transplant are extremely common. The physiatrist needs to sort through the extensive differential diagnoses of these impairments (Table 60-3).
Table 60–1 Systemic and Metabolic Effects of Transplant Rejection Drugs
| Drug | Adverse Effects | Clinical Manifestations |
|---|---|---|
| Azathioprine |
ALT, Alanine aminotransferase; AST, aspartate aminotransferase; BUN, blood urea nitrogen; GI, gastrointestinal; TTP, thrombotic thrombocytopenic purpura.
Table 60-2 Immunosuppressive Medication Monitoring for Physiatrists
| Drug | Side Effects | Monitor |
|---|---|---|
| Prednisone | ||
| Cyclosporine | ||
| Azathioprine |
BUN, Blood urea nitrogen; CBC, complete blood count; GI, gastrointestinal; Hct, hematocrit; LFT, Liver function test.
Table 60-3 Neuromusculoskeletal Complications After Transplantation and Their Possible Etiologies
| Complication | Etiologies |
|---|---|
| Delirium | Intensive care unit psychosis, hyponatremia, hypernatremia, hypoglycemia, sepsis, hypotension, hypoxemia, medications, encephalitis (bacterial, fungal, or viral) |
| Stroke | Embolic, watershed infarct from hypotension, mycotic aneurysm, vasculitis (sirolimus-induced) |
| Paraparesis | Spinal cord infarction, myelopathy |
| Peripheral neuropathy | Critical illness, metabolic, diabetic, transplant medications (cyclosporine, FK506, sirolimus), nerve impingements (brachial plexus, accessory, axillary, median, ulnar, femoral, sciatic, peroneal) |
| Tremor | Cyclosporine, tacrolimus, sirolimus |
| Myopathy | Critical illness, steroid, statin, cyclosporin |
| Contracture | Positioning, graft vs. host disease, nephrogenic |
| Osteoporotic fracture | Steroids, immobility |
Rehabilitation Through Renal Transplantation
As the number of people with end-stage renal failure continues to increase, kidney transplantation is being performed with increased frequency and improved outcome. From 1998 to 2004, there has been a steady increase in the number of kidneys transplanted (Table 60-4). In 2003 to 2004, there were 16,004 kidney transplants, representing an increase of 3552 since 1998. Despite the increase in kidney transplants, there has been a decrease in the number of kidney–pancreas transplants (Table 60-5). Compared with the 972 simultaneous kidney–pancreas transplants (SKPT) performed in the United States in 1998, there has been a significant decrease to approximately 881 of these procedures in 2003 to 2004. Recent literature has demonstrated that the long-term survival of SKPT recipients is superior to that of cadaver kidney transplant recipients with type 1 diabetes. There is no difference, however, in survival of SKPT recipients and living donor kidney recipients with type 1 diabetes at up to 8 years follow-up.109
Fatigue and problems with the performance of the activities of daily living (ADL) pose limitations to patients with ESRD.52 Many renal failure patients are unable to perform even the most basic tasks of everyday life. A majority of patients are unable to work because they are physically unable to sustain their energy levels. However, the greatly enhanced survival rates of patients who have received a transplant, coupled with the net increase in procedures performed annually, have resulted in a growing number of patients who now require rehabilitation and restorative services.
Complications that can surface during the postoperative period include infection, bleeding, and rejection. The rehabilitation team must be aware of the signs of kidney rejection. Acute rejection is frequently heralded by anorexia, malaise, fever, hypertension, leukocytosis, blood urea nitrogen (BUN) elevation, and kidney enlargement with localized tenderness. Immunosuppressant medications, including prednisone, azathioprine, and cyclosporine, carry a host of side effects and reactions. Evidence of kidney rejection, which includes graft site tenderness, reduced urinary output, elevated temperature, and edema, can arise during postacute rehabilitation. (See Box 60-2 for a list of the clinical signs associated with kidney transplant rejection.)
Options to Enhance Exercise After Kidney Transplantation
A number of important physiologic factors affect the renal transplant recipient’s ability to exercise. Chronic renal failure is well known to induce stress on the cardiovascular system.101 Metabolic abnormalities, such as imbalance of electrolytes, including sodium and water retention, can augment right and left ventricular preload. As circulatory volume expands, hypertension is exacerbated and increased afterload is maintained. This situation frequently leads to the development of cardiac hypertrophy, greater ventricular stiffness, and diminished compliance.
The ability to exercise can be maximized in several ways, including exercise training and treatment with recombinant human erythropoietin (epoetin). However, recent data have uncovered physiologic limitations to exercise capacity that are not simply overcome by exercise training or normalization of hematocrit.99 Exercise training after renal transplant results in higher levels of measured and self-reported physical functioning, although exercise alone does not affect body composition.100 A successful kidney transplant can greatly increase exercise capacity to near-normal values for sedentary healthy individuals.41
Exercise training after transplant further increases exercise capacity and counteracts some of the negative side effects of glucocorticoid therapy, such as muscle wasting and excessive weight gain. Studies have shown that before epoetin administration, exercise training alone in patients on dialysis can increase exercise tolerance by 25%. Similar but smaller increases are observed after correction of anemia with epoetin. Physiatrists frequently need to encourage renal patients to exercise and improve their physical functioning by overcoming their fatigue.100 Renal rehabilitation is an essential therapeutic method for improving physical fitness, social functioning, and well-being, and is reflected by an increase in health-adjusted quality of life among ESRD and posttransplant patients.
Just as the ability to exercise is significantly impaired in chronic renal patients, patients who have received transplanted kidneys also demonstrate exercise intolerance.42 Several factors contribute to this challenge, including skeletal muscle atrophy, anemia, and cardiovascular deconditioning.
Kidney transplants are often performed in conjunction with pancreas transplants for patients with severe end-organ damage resulting from diabetes mellitus. An increasing number of these patients are surviving and moving on to rehabilitation and vocational rehabilitation services (Figure 60-2).93
Rehabilitation of the Person Through Cardiac Transplantation
Heart Transplant Epidemiology
Since the inauguration of the procedure in 1967, the survival rate of patients undergoing heart transplant continues to improve.126 With constant refinements in surgical technique, more than 2000 heart transplants had been performed throughout the world by 1990. As a result of the increase in organ availability and surgical capacity in the United States, the waiting list of candidates decreased 45%, from 2414 in 1997 to 1327 in 2006. Patients on the waiting list are assigned a level of urgency based on medical condition and requirements for continuous circulatory support. The highest priority candidates, designated as status 1A, require hospitalization with continuous mechanical circulatory support, such as an implanted cardiac pump or aortic balloon pump. Status 1B patients can remain at home but require continuous intravenous inotropes and an occasional ventilator. Most wait-list candidates are listed as status 2. Outcomes are improving as well, and heart transplant recipient survival has exceeded 92% at 3 months, 88% at 1 year,92 and 85% at 5 years.32 The Stanford Group has recently reported on their 20-year survivors, who require ongoing treatment for a variety of problems including hypertension (87%), malignancy (44%), vasculopathy (43%), and diabetes (14%).32
It is estimated that survival rates after heart transplantation will continue to improve with careful systematic patient selection, better surgical techniques, lower rejection rates, and continuous rehabilitation.66,122,152
Rehabilitation Before the Heart Transplant
Congestive heart failure (CHF) that is unresponsive to medical therapy is not only a primary impairment but also a major indicator for heart transplantation. The disease processes leading to CHF include idiopathic cardiomyopathy, viral myocarditis, ischemic heart disease, and valve dysfunction.62,79 It is essential that the assessments of both the cardiologist and the physiatrist be integrated to better understand the disease process and its probable impact on the patient’s quality of life. This assessment includes quantification of circulatory impairments, exercise performance, associated diagnoses, and the health of other organ systems.19
The success of heart transplantation depends on careful selection of suitable patients (Box 60-3). The most successful outcomes depend on identifying candidates who have the physical capacity that would enable them to maximally benefit from the new heart and rehabilitation.126 During the period of heart procurement, implantation of devices, such as the Ventes left ventricular assist devices, the HeartMate, and total artificial heart, can improve tolerance for activity and allow preliminary rehabilitation.43,108 Careful surveillance for declining cardiac function and irreversible heart disease helps manage a patient before transplantation. Several criteria used for cardiac transplant candidate selection are outlined in Box 60-4.133
Complications After Cardiac Transplantation
The cardiac rehabilitation team should be familiar with the complications of transplantation to recognize and treat problems that might affect patients’ functional performance. Coordination of care and communication between the cardiac surgeon, cardiologist, and the physiatrist is essential for success. The main complication posttransplant is allograft failure from rejection. Secondary complications include problems related to immunosuppression, such as infection, neurotoxicity, renal toxicity, hypertension, and various metabolic abnormalities. One study of cardiac transplant recipients on an inpatient rehabilitation unit uncovered multiple secondary complications, including hypertension, nutritional limitations, neuromuscular deficits, and compression fractures.62 Stress fractures of the weight-bearing limbs have also been described83 and are most likely due to steroid-induced osteoporosis. Monitoring vitamin D levels and supplementation with 1000 to 2000 units daily reduce risk. Physiatrists should be clinically familiar with these problems and be prepared to evaluate and treat them.
Many patients develop hypertension as a result of cyclosporine-induced renal vasoconstriction superimposed on chronic renal hypoperfusion, third spacing of fluids, and an abnormal distribution of blood flow.24,45,86,95 Cyclosporine is believed to cause afferent glomerular arteriolar vasoconstriction through an increase in transmembrane calcium flux in mesangial and vascular smooth muscle cells.83,95 Blood pressures should be closely monitored, with morning blood pressure values used as a guide for antihypertensive therapy.24,99 In most cases this can be achieved without interruption of the exercise therapy regimen. Alternative cyclosporine dosing regimens, calcium channel antagonists, and angiotensin-converting enzyme inhibitors are preferred therapies to promote arteriolar dilation.18,82,142 Proper management of the hypertension facilitates full participation in rehabilitation.
Cardiac transplantation itself can cause neurologic complications, including metabolic encephalopathy, stroke, central nervous system infection, seizures, and psychosis. These potential complications are most likely to present during the acute posttransplant period, although they can also surface during the rehabilitative/restorative phase.124 The mechanisms for strokes include particulate embolism, air embolism, and inadequacy of perfusion during the transplantation procedure. Careful review of mental status, perceptual sensation, and motor function is an essential part of the physiatric consultation in the postoperative phase.
Acute rejection in cardiac transplantation is a major complication that can be heralded by fulminant CHF, accumulation of peripheral edema, premature atrial contractions, a diastolic gallop, and sudden marked reduction in exercise capacity. Chronic rejection can also progress with accelerated graft atherosclerosis.30,146 At 1 year posttransplantation, 10% to 15% of patients develop accelerated graft atherosclerosis, which increases to 35% to 50% by the fifth postoperative year.35,122 Cardiac denervation produces an up-regulation of muscarinic receptors, which facilitates increased calcium influx in the coronary arteries of the transplanted heart. This causes diffuse circumferential narrowing of the arterial luminal diameters. This type of coronary artery disease ultimately is a key barrier to the long-term survival of cardiac transplant patients. Recent studies, however, suggest that it can be prevented and improved with calcium channel blockers.119,122 This condition should be placed on the problem list, and a plan should be designed for its prevention, surveillance, and acute management.
Beyond the postoperative complications outlined above, the leading cause of death in post–cardiac transplant patients is infection.88,143 The types of infections include mediastinitis, pneumonia, urinary tract infections, and intravenous catheter-induced sepsis.55,88,143 Such problems tend to develop during the first 2 years after the cardiac transplant.14,89 Bacterial and viral infections account for 47% and 41% of infections, respectively. Infections caused by fungus and protozoa account for 12% of posttransplant morbidity. This makes it imperative that infection control techniques be used, especially adequate washing of the hands for a full 30 seconds or use of an equivalent topical antiseptic or both before and after direct contact with the transplant patient.