Chapter 60 The pancreas as a site of metastatic cancer
Overview
Resection has become an established part of the standard therapy for liver and lung metastases of several primary tumors (Fong et al, 1999; Quiros & Scott, 2008). Unlike liver and lung, the pancreas is an uncommon site of metastases. In autopsy series, 3% to 12% of patients with diffuse metastatic disease have pancreatic involvement (Showalter et al, 2008), and metastases account for only about 2% to 4% of malignant lesions in the pancreas (Showalter et al, 2008; Strobel et al, 2009). However, this number is increased up to 40% in patients with a pancreatic mass and a history of malignant disease (Roland & van Heerden, 1989; Z’Graggen et al, 1998).
Metastases to the pancreas may occur as isolated lesions or with additional extrapancreatic metastases that are technically resectable; isolated pancreatic metastases are very rare. Until recently the available data on resection for pancreatic metastases were based only on small series and multiple case reports. However, recent larger series and meta-analyses suggest that resection for pancreatic metastases is safe and associated with a favorable long-term outcome in appropriate patients (Reddy et al, 2008; Reddy & Wolfgang, 2009; Strobel et al, 2009; Tanis et al, 2009). This is best documented for metastastic renal cell carcinoma (RCC), the most frequent primary tumor of isolated pancreatic metastases (Sellner et al, 2006; Tanis et al, 2009). Based on these recent data, pancreatic resection can be recommended as part of an interdisciplinary treatment in metastatic disease to the pancreas.
Results of Surgery for Pancreatic Metastases
Because isolated pancreatic metastases and metastases with localized, treatable extrapancreatic disease are uncommon, the results of pancreatic resection for metastases are not as well documented as for the liver or lung (Fong et al, 1999; Internullo et al, 2008). Until recently, the available literature was based only on smaller series and multiple case reports, which inherently tend to be biased toward the report of favorable results. However, in recent years, resection for metastases to the pancreas has been used more frequently, resulting in several larger series and, most recently, meta-analyses. This change occurred for several reasons. In the last decades, morbidity and mortality rates of pancreatic surgery decreased considerably, and pancreatic surgery can now be considered a safe procedure when performed by experienced surgeons (see Chapter 62A, Chapter 62B ). With the development of more effective drugs and tailored chemotherapy, the prognosis of metastatic disease has largely improved for several tumor entities. Also, with standardized follow-up programs after resection for cancer and with broader use of cross-sectional imaging, pancreatic metastases are more frequently detected at a resectable stage. Finally, the decision for resection of a pancreatic metastasis is more frequently made in an interdisciplinary setting, such as by tumor boards, which are established in most centers.
Safety of Resection for Pancreatic Metastases
In a recent review of 19 series, a mortality rate of 1.2% and a morbidity rate of 38.3% were reported for resection of isolated pancreatic metastases (Reddy & Wolfgang, 2009). Resections for metastatic disease may be more difficult than resections for primary pancreatic tumors because of the necessity of extensive adhesiolysis after previous surgery in approximately 80% of patients and because of the necessity of multivisceral resections. Our series, which included 41% multivisceral resections, reported a mortality rate of 4.4% and a morbidity rate of 33% (Strobel et al, 2009). These findings are comparable to the data reported for primary pancreatic malignancies and show that resection for pancreatic metastases can be performed safely by specialized surgeons.
Oncologic Outcome of Resection for Pancreatic Metastases
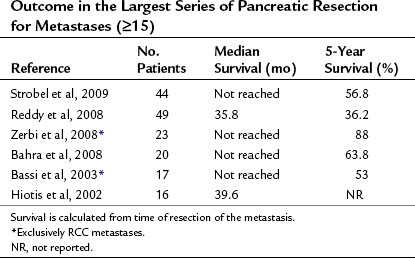
The follow-up results of the largest studies of resection for pancreatic metastases are summarized in Table 60.1 and show a very favorable outcome. However, most series include several primary tumor entities, and conclusions about individual tumor types must be made with great caution. RCC is, by far, the most frequent primary tumor associated with resectable, isolated pancreatic metastases. The frequency of various primary tumors derived from surgical series is given in Table 60.2. The data for resection of RCC metastatic to the pancreas are summarized in Table 60.3; they show considerably longer survival rates compared with the mixed group of other histologies (see Table 60.1). Two systematic reviews of 236 and 311 published cases of surgery for RCC pancreatic metastases (Sellner et al, 2006; Tanis et al, 2009) report 5-year survival rates of about 75% after radical resection. However, because both reviews included case reports and smaller series, they may overestimate survival rates because of publication bias. However, RCC histology was also associated with improved outcome in several of the published series, including that of the authors (Eidt et al, 2007; Hiotis et al, 2002; Reddy et al, 2008; Strobel et al, 2009).
Table 60.2 Pathologic Diagnosis in Patients with Pancreatic Resections for Metastases
| Primary Tumor Type | No. Patients | % of Total |
|---|---|---|
| Renal cell cancer | 181 | 63.1 |
| Colorectal cancer | 22 | 7.7 |
| Sarcoma | 17 | 5.9 |
| Melanoma | 13 | 4.5 |
| Gastric cancer | 10 | 3.5 |
| Lung cancer | 9 | 3.1 |
| Gallbladder cancer | 8 | 2.9 |
| Breast cancer | 6 | 2.1 |
| Ovarian cancer | 5 | 1.7 |
| Gastrointestinal stromal tumor | 2 | 0.7 |
| Esophageal cancer | 2 | 0.7 |
| Mesenteric fibromatosis | 2 | 0.7 |
| Schwannoma | 2 | 0.7 |
| Merkel cell carcinoma | 1 | 0.3 |
| Seminoma | 1 | 0.3 |
| Teratocarcinoma | 1 | 0.3 |
| Hemangiopericytoma | 1 | 0.3 |
| Urinary bladder cancer | 1 |