The Gastrointestinal System
SYSTEMWIDE ELEMENTS
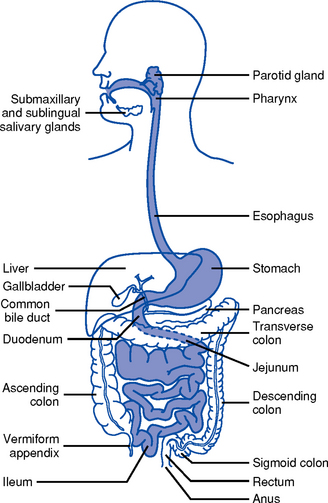
1. Upper gastrointestinal (GI) tract (Figure 8-1)
i. Lips, gums and teeth, and inner structures of the cheeks, tongue, hard and soft palate, and salivary glands
ii. Chewing prepares food by softening and moving it around, mixing it with saliva, and forming a bolus
iii. Skeletal muscles for chewing are coordinated by cranial nerves V, VII, IX, X, XI, XII
iv. Saliva aids in swallowing; approximately 570 ml/day of saliva is secreted. Submandibular, parotid, and sublingual salivary glands along with minor salivary glands in the oral mucosa secrete mixed saliva, which is 99% water and 1% solids, and includes electrolytes and organic protein molecules.
i. Extends from the cricoid cartilage to the level of the sixth cervical vertebra
ii. Swallowing receptors are stimulated by the autonomic nervous system when a food bolus moves toward the back of the mouth. The motor impulses to swallow are transmitted via cranial nerves V, IX, X, and XII.
i. Transports food from the mouth to the stomach and prevents retrograde movement of the stomach contents
ii. Collapsible tube about 25 cm long that lies posterior to the trachea and the heart
(a) Begins at the level of the sixth cervical vertebra and extends through the mediastinum and diaphragm to the level of the first thoracic vertebra, where it attaches to the stomach below the level of the diaphragm
(b) Upper portion of the esophagus is striated skeletal muscle, which is gradually replaced by smooth muscle so that the lower third of the esophagus is totally smooth muscle
(c) Motor and sensory impulses for swallowing and food passage derive from the vagus nerve. Lower esophagus also innervated by splanchnic and sympathetic neurons. Food moves by the strong muscular contraction of peristalsis and by gravity. In the absence of gravity, nutrients transported by muscular contractions.
(d) Sphincters: Hypopharyngeal (proximal) prevents air from entering the esophagus during inspiration; gastroesophageal (distal) prevents gastric reflux into the esophagus
(a) Arterial supply: Celiac trunk includes the gastric, pyloric, right, and left gastroepiploic arteries
(b) Venous drainage: Splanchnic bed drains the entire GI tract; gastric vein drains the stomach and esophagus
(c) Direct drainage into the azygous and hemiazygous veins of the mediastinum; all of these then drain into the portal vein
i. Food storage reservoir and site of the start of the digestive process. Normal capacity is 1000 to 1500 ml but can hold up to 6000 ml.
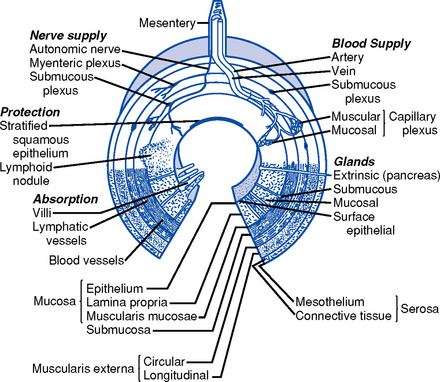
ii. Layers of the stomach and intestinal wall (Figure 8-2)
(a) Mucosa: Cells produce mucus that lubricates and protects the inner surface. These cells are replaced every 4 to 5 days. This layer receives the majority of the blood supply of the stomach.
(1) Epithelium: Contains the gastric, cardiac, fundic, and pyloric glands
a) Gastric cells: Contain microvilli that monitor intragastric pH
b) Cardiac glands: Secrete alkaline mucus, a lubricant that continually bathes and protects the epithelial lining from autodigestion
(2) Lamina propria: Contains lymphocytes; site of gut immunologic response
(b) Submucosa: Contains connective tissue and elastic fibers, blood vessels, nerves, lymphatic vessels, and structures responsible for secreting digestive enzymes
(c) Circular and longitudinal smooth muscle layers: Continue the modification of food into a liquid consistency and move it along the GI tract. Movements are tonic and rhythmic, occurring every 20 seconds. Electrical activity is constantly present in the smooth muscle layers.
(1) Hormone secreted in response to distention of antrum or fundus by food
(2) Stimulates secretion of hydrochloric acid by the parietal cells and secretion of pepsin by chief cells
(b) Histamine: Hormone secreted by mast cells in the presence of food that is critical to the regulation of gastric acid secretions
(a) Is proportional to the volume of material in the stomach
(b) Depends on the character of the ingested material: Liquids, digestible solids, fats, indigestible solids
(c) Factors accelerating gastric emptying: Large volume of liquids; anger; insulin
(d) Factors inhibiting gastric emptying: Fat, protein, starch, sadness, duodenal hormones
(1) Coordinated by the vomiting center in the medulla in response to afferent impulses from various regions of the body
(2) Stimuli that induce vomiting: Tactile stimulation to the back of the throat, increased intracranial pressure (ICP), intense pain, dizziness, anxiety
(3) Autonomic nervous system discharge may precede vomiting: Sweating, increased heart rate, increased salivation, nausea, muscular force by the diaphragm and abdomen
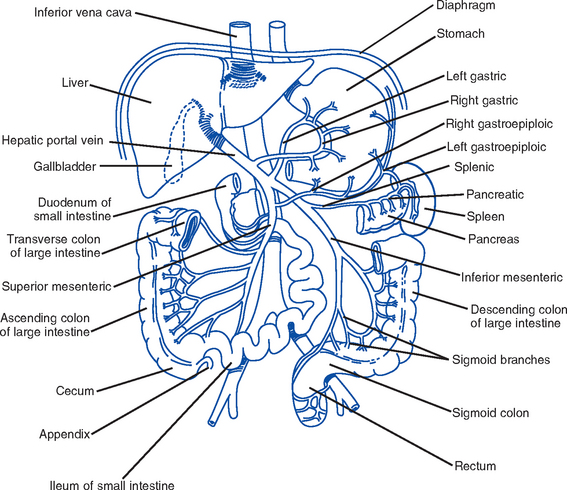
(a) Arterial: Celiac artery flows into the right gastric artery, left gastric artery, gastroduodenal artery, and finally into the right gastroepiploic artery; the splenic artery flows into the left gastroepiploic artery
(b) Venous drainage: Splanchnic bed drains the entire GI tract, the gastric vein drains the stomach and esophagus; both vessels drain into the portal vein
(a) Intrinsic nervous system (intramural neurons) within the wall of the GI tract is independent of central nervous system controls
(1) Myenteric (Auerbach’s) plexus: Located between the circular and longitudinal muscles; stimulation increases muscle tone, contractions, velocity, and excitation of the digestive tract
(2) Submucosal (Meissner’s) plexus: Located between the circular and submucosal layers; influences secretions of the digestive tract; contains secretomotor and enteric vasodilator neurons
(b) Extrinsic system: Via the central nervous system, parasympathetic system, and sympathetic system
(1) Parasympathetic: Fibers arise from the medulla and spinal segments (i.e., vagus nerves)
a) Cranial segments: Transmission via the vagus nerve; innervate the stomach, pancreas, and first half of the small intestine
b) Sacral segments: Innervate the distal half of the large intestine, sigmoid, rectum, and anus
c) Enhances function of the intrinsic nervous system and the secretion of acetylcholine
d) Increases glandular secretion and muscle tone; decreases sphincter tone
(2) Sympathetic: Motor and sensory fibers arise from the thoracic and lumbar segments; distribution is via the sympathetic ganglia (i.e., celiac plexus)
2. Middle GI tract: Small intestine
a. Approximately 5 m long; extends from the pylorus to the ileocecal valve
b. Consists of three divisions: Duodenum, jejunum, ileum
c. Primary function is absorption of nutrients
d. Layers of the intestinal wall (Figure 8-2)
i. Mucosa: Innermost layer; receives the majority of the blood supply; the predominant site of nutrient absorption
(a) Epithelium: Covered with villi and microvilli that increase the surface area of the small intestine several hundred times; contain glands, crypts of Lieberkühn (intestinal glands) that secrete approximately 2 L of fluid every 24 hours and goblet cells that secrete mucus
(b) Lamina propria: Contains lymphocytes; site of gut immunologic responsiveness
ii. Submucosa: Contains loose connective tissue and elastic fibers, blood vessels, lymphatic vessels, and nerves
iii. Muscularis: Muscle layer; function is involuntary and involved in motility
iv. Serosa: Outermost layer; protects and suspends intestine within the abdominal cavity
e. Peristalsis: Propulsive movements that move the intestinal contents toward the anus. Approximately 3 to 5 hours is necessary for passage through the entire small intestine.
i. Arterial: Derived from the celiac artery (first portion of the duodenum) and the superior mesenteric arteries (remainder of the duodenum, jejunum, ileum, cecum)
ii. Venous drainage: Splanchnic bed drains the entire GI tract
g. Innervation: Same as for stomach
h. Small intestine digestive enzymes not secreted, but integral components of the mucosa
i. Bile and pancreatic enzymes are secreted into the duodenum
ii. In the jejunum and the ileum, food is digested and absorbed
iii. Up to 3000 ml/day of digestive enzymes (e.g., lipase, amylase, maltase, and lactase)
i. Secretin: Secreted by the mucosa of the duodenum in response to acidic gastric juice from the stomach and to alcohol ingestion
(a) Augments the action of cholecystokinin (CCK)
(b) Stimulates release of the alkaline component of pancreatic juice and the secretion of water
ii. CCK: Secreted by the mucosa of the jejunum in response to the presence of fat, protein, and acidic contents in the intestine
(a) Increases contractility and emptying of the gallbladder and blocks the increased gastric motility caused by gastrin
(b) Stimulates secretion of pancreatic digestive enzymes, bicarbonate, and insulin
iii. Gastric inhibitory peptide (GIP): Secreted by the mucosa of the upper portion of the small intestine in response to the presence of carbohydrates and fat in the intestine; inhibits gastric acid secretion and motility, slowing the rate of gastric emptying
iv. Vasoactive intestinal peptide: Secreted throughout the gut in response to acidic gastric juice in the duodenum
(a) Main effects are similar to those of secretin
(b) Stimulates the secretion of intestinal juices to decrease the acidity of chyme and inhibits gastric secretion
v. Somatostatin: Secreted throughout the intestine in response to vagal stimulation, ingestion of food, and release of CCK, GIP, glucagon, and secretin
(a) Inhibits the secretion of saliva, gastric acid, pepsin, intrinsic factor, and pancreatic enzymes
(b) Inhibits gastric motility, gallbladder contraction, intestinal motility, and blood flow to the liver and intestine
vi. Serotonin: Secreted throughout the intestine in response to vagal stimulation, increased luminal pressure, and the presence of acid or fat in the duodenum; inhibits gastric acid secretion and mucin production
j. Functions: Almost all absorption occurs in the small intestine via four mechanisms: Active transport, passive diffusion, facilitated diffusion, and nonionic transport
i. Vitamins are absorbed primarily in the intestine by passive diffusion, except for the fat-soluble vitamins, which require bile salts for absorption, and vitamin B12, which requires intrinsic factor
ii. Water absorption: Approximately 8 L of water per day is absorbed by the small intestine
iii. Electrolyte absorption: Most occurs in the proximal small intestine
iv. Iron absorption: Absorbed in the ferrous form in the duodenum
v. Carbohydrate absorption: Complex carbohydrates are broken down into monosaccharides or basic sugars (fructose, glucose, galactose) by specific enzymes (e.g., amylase, maltase)
vi. Protein absorption: Protein is broken down into amino acids and small peptides; essential amino acids are lysine, phenylalanine, isoleucine, valine, methionine, leucine, threonine, and tryptophan
i. Approximately 6.5 cm in diameter and 1.5 m long; extends from terminal ileum at the ileocecal valve to the rectum
ii. Ileocecal valve: Prevents return of feces from the cecum into the ileum
i. Cecum: Blind pouch to which the appendix is attached; about 2.5 cm from the ileocecal valve
ii. Ascending colon: Extends from the cecum to the lower border of the liver, where it forms the right hepatic flexure
iii. Transverse colon: Crosses the upper half the abdominal cavity, curving downward at the lower end of the spleen at the left colonic (splenic) flexure anterior to the small intestine
iv. Descending colon: Extends from the splenic flexure to the sigmoid colon
v. Sigmoid colon: S-shaped curve extending from the descending colon to the rectum
c. Layers of the large intestine wall (Figure 8-2): No villi and no secretion of digestive enzymes. Layers similar to those of the middle GI tract with exceptions:
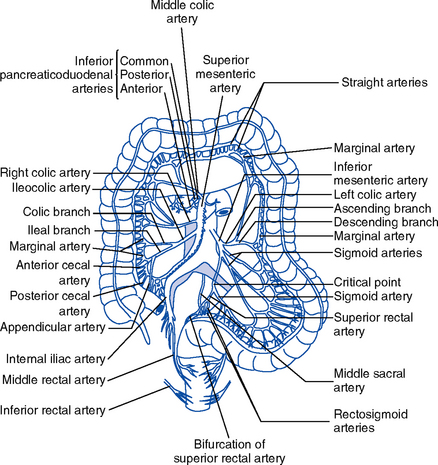
(a) Superior mesenteric artery supplies the ascending colon and part of the transverse colon
(b) Inferior mesenteric artery feeds the transverse colon, sigmoid colon, and upper rectum
(c) Hypogastric arteries give rise to the middle and inferior rectal and hemorrhoidal arteries
(d) Rectal arteries, which arise from the internal iliac arteries, supply the distal rectum
i. Absorption of water and electrolytes: Approximately 500 ml of chyme (the byproduct of digestion) enters the colon per day and, of this, 400 ml of water and electrolytes are reabsorbed
ii. Breakdown of cellulose by enteric bacteria
iii. Synthesis of vitamins (folic acid, vitamin K, riboflavin, nicotinic acid) by enteric bacteria
iv. Storage of fecal mass until it can be expelled from the body
(a) Takes approximately 18 hours from the time food enters the colon until the intestinal contents reach the distal portion of the colon
(b) Time from ingestion of food to defecation of the residue may be 24 hours or longer
(a) Peristalsis: Propulsive movements that push GI contents toward the anus
(b) Haustral churning is the major type of movement in the colon
(c) Factors that enhance motility: Bacterial enterotoxins, viral infections of the gut, regional enteritis, ulcerative colitis, increased bile salts, osmotic overload, laxatives
(d) Factors that inhibit motility: Low-bulk diet, parenteral nutrition, bed rest, dehydration, ileus, fasting, drugs
(e) Poor motility causes more absorption, and the development of hard feces in the transverse colon causes constipation
(f) Aging causes a reduction in peristalsis and decreased GI motility throughout the GI system
f. Innervation: Same as for the stomach and small intestine
i. The gut encounters a variety of potentially harmful substances daily; these can include natural toxins in food, insecticides, preservatives, chemical waste products, and airborne particulate matter that is swallowed.
ii. Mechanisms exist within the GI tract to protect the integrity of the gut and thus the individual
iii. Fluid and cellular layers
(a) Aqueous layer: Stationary layer immediately adjacent to the microvillus border of the enterocytes; consists of acids, digestive enzymes, and bacteria depending on the location in GI lumen
(b) Mucosal barrier: Physical and chemical barriers that protect the wall of the gut from harmful substances. Surfaces of the stomach, intestine, biliary and pancreatic ducts, and gallbladder have cells that synthesize and release mucus.
(c) Epithelial cells: Tight junctions between cells regulated by hormones and cytokines make them relatively impervious to large molecules and bacteria; rapid proliferation of cells minimizes the adherence of flora. The level of permeability varies within the various segments of the GI tract.
(d) Mucus-bicarbonate barrier: Forms a layer of alkalinity between the epithelium and luminal acids that neutralizes the pH and protects against surface shear
iv. Motility: Prevents bacteria in the distal small intestine from migrating proximally into the sterile parts of the upper GI system
(1) Expulsion of toxic substances as a result of stimulation of the vomiting center in the medulla
(2) Barrier against the reflux of duodenal contents back into the stomach
(b) Colon: Moves pathogens and potential carcinogens out of the body
v. Gut immunity: Necessary because the gut is a reservoir of potentially pathogenic bacteria
(a) B lymphocytes that bear surface immunoglobulin A (IgA) or synthesize secretory IgA that prevents antigens from binding to mucous cells
vi. Gastric acid: Intragastric pH below 4.0 is essential
vii. Commensal bacteria: Natural gut flora are stable and protective in a healthy person by competing with pathogenic species for nutrients and attachment sites, and produce inhibitory substances against pathogenic species
(a) Stomach, duodenum, and jejunum are sterile
(b) Ileum contains aerobic and anaerobic bacteria: Dietary intake is a major factor in determining intestinal flora
(c) Large intestine contains large numbers of aerobic and anaerobic bacteria, and smaller numbers of yeast and fungi
viii. Impaired gut barrier function facilitates bacterial translocation, which is the egress of bacteria and/or their toxins across the mucosal barrier and into the lymphatic vessels and portal circulation
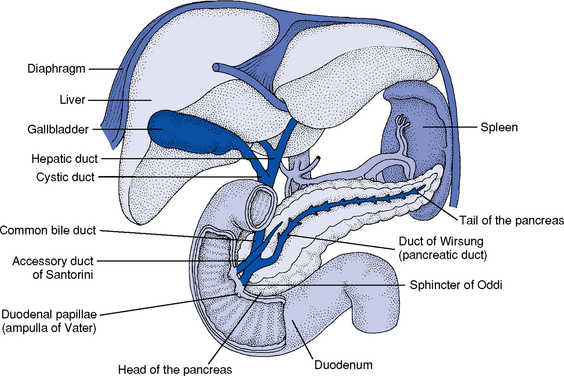
4. Accessory organs of digestion (Figure 8-4)
i. Largest solid organ, weighing approximately 3 lb (1500 g), located in the right upper quadrant, beneath the diaphragm
ii. Consists of three lobes divided into eight independent segments, each of which has its own vascular inflow, outflow, and biliary drainage. Because of this division into self-contained units, each can be resected without damaging those remaining.
(a) Right lobe: Anterior (segments V and VIII) and posterior (segments VI and VII)
(b) Left lobe: Medial (segment IV) and lateral (segments II and III); the left lobe extends across the midline into the left upper quadrant
iii. Microscopically the liver consists of functional units called lobules composed of portal triads in which the bile ducts, hepatocytes, and artery are located. The portal triads are then bounded by sinusoids and a central vein. A cross section of a classic lobule or acinus is hexagonal.
iv. Blood supply (Figure 8-5): Derived from both a vein and an artery
(a) 25% of cardiac output flows through the liver per minute
(b) Portal vein (after draining the mesenteric veins and pancreatic and splenic veins) and hepatic artery (off the aorta via the celiac trunk) enter the liver at the porta hepatis or hilum (a horizontal fissure in the liver, containing blood and lymph vessels, nerves, and the hepatic ducts)
(c) 75% is supplied by the portal vein; each segment receives a branch of the portal vein and 25% is supplied by the hepatic artery
(d) Small branches of each of these vessels enter the acinus at the portal triad (an area in the liver consisting of the portal vein, branches of the hepatic artery, and tributaries to the bile duct
(e) Functionally, the liver can be divided into three zones, based on oxygen supply. Zone 1 encircles the portal tracts where the oxygenated blood from hepatic arteries enters. Zone 3 is located around the central veins, where oxygenation is poor. Zone 2 is located in between.
(f) Blood from both the portal vein and the hepatic artery mixes together in the hepatic sinusoids and then flows through the sinusoids to the hepatic venules (zone 3) through the central veins, branches of the hepatic vein
(1) Found between plates (layers) of hepatocytes; have a porous lining with fenestrations that allows nutrients in the blood plasma to wash freely over exposed surfaces (the spaces of Disse)
(2) Sinusoidal lining consists of endothelial cells, Kupffer cells, perisinusoidal fat-storing cells, and pit cells.
(h) Venous drainage: Begins in the central veins in the center of the lobules; central veins empty into the hepatic veins, which empty into the inferior vena cava
v. Biliary duct system for draining bile
(a) Begins at the sinusoidal level as bile canaliculi, which branch into ductules, intralobular bile ducts, and larger intrahepatic ducts
(b) Intrahepatic ducts come together at the porta hepatis to form the common hepatic duct, which becomes the common bile duct after joining with the cystic duct and drains into the duodenum
vi. Physiology: The liver is a metabolically complex organ with interrelated digestive, metabolic, exocrine, hematologic, and excretory functions. The many functions it performs are interwoven; each lobe is an independent functional unit, so that up to 80% of the liver can be destroyed and it will regenerate.
(a) Digestive functions: Plays a role in the synthesis, metabolism, and transport of carbohydrates, fats, and proteins
(1) Carbohydrates: Maintains normal serum glucose levels by
a) Glycogen storage: Approximately 900 kcal of glycogen reserves are stored in the adult liver
b) Glycogenesis: Conversion of excess carbohydrates to glycogen for storage in the liver as a metabolic reserve
c) Glycogenolysis: Conversion of large stores of glycogen in muscles and liver to glucose
d) Gluconeogenesis: Manufacture of glucose from noncarbohydrate substrate (fat, fatty acids, glycerol, amino acids)
a) Bile secretion for fat digestion plays a role in fat and lipid synthesis, metabolism, and transport
b) Principal site of synthesis and degradation of lipids (cholesterol, phospholipids, lipoprotein): Produces approximately 1000 mg of cholesterol per day
c) Exogenous lipoprotein metabolism
d) Endogenous lipoprotein metabolism: Major lipoprotein synthesized by the liver is very-low-density lipoprotein (VLDL); one third of VLDL remnants are converted to low-density lipoprotein (LDL)
e) Conversion of excess carbohydrate to triglyceride, which is stored as adipose tissue
f) Conversion of triglyceride to glycerol and fatty acids for energy
g) Storage of triglyceride and fat-soluble vitamins (A, D, E, and K)
h) Storage of fats, cholesterol, proteins, vitamin B12, and minerals
a) Production of plasma proteins (albumin, prealbumin, transferrin, clotting factors, haptoglobin, ceruloplasmin, α1-antitrypsin, complement, α-fetoprotein)
b) Deamination: Metabolism of amino acids
c) Transamination: Conversion of amino acids to ammonia, conversion of ammonia to urea for urinary excretion
(b) Endocrine functions: Metabolism of glucocorticoids, mineralocorticoids, hormones
(d) Hematologic functions: Synthesis of bilirubin, coagulation factors
b. Gallbladder: Pear-shaped saclike organ that serves as a reservoir for bile
i. Attached to the inferior surface of the liver in the area that divides the right and left lobes (gallbladder fossa)
ii. Approximately 7 to 10 cm long; holds and concentrates approximately 30 ml of bile
iii. Blood supply: Arterial blood supply is from the cystic artery; venous drainage is via a network of small veins.
iv. Innervation: Splanchnic nerve, right branch of the vagus nerve
v. Cystic duct attaches the gallbladder to the common hepatic duct
(a) Union of the cystic duct and the common hepatic duct forms the common bile duct
(b) Common bile duct either joins the pancreatic duct outside the duodenum or forms a common channel through the duodenal wall at the ampulla of Vater
(c) Intraduodenal segment of the common bile duct and the ampulla is the sphincter of Oddi
vi. Presence of CCK in the blood (in response to chyme in the duodenum)
vii. Bile is composed of water, bile salts, and bile pigments
(a) Bile salts are responsible for the absorption and emulsification of fat and fat-soluble vitamins
(b) Bile pigments: High in cholesterol and phospholipids, give feces a brown color
(c) Bilirubin is the major bile pigment; it is a breakdown product of hemoglobin metabolism from senescent red blood cells
(1) Total: Indirect bilirubin plus direct bilirubin; when total bilirubin level is elevated and the cause is unknown, indirect and direct bilirubin fractions can be measured
(2) Indirect (unconjugated): Bilirubin bound to albumin before it binds to glucuronic acid; fat soluble. Causes of elevation of indirect bilirubin concentration in serum include the following:
a) Any hemolytic process (e.g., ABO mismatch in blood transfusion, β-hemolytic streptococcal infection)
b) Gilbert’s syndrome, a common disorder characterized by a mild, chronic fluctuating increase in the level of unconjugated bilirubin
c) Inherited deficiency of bilirubin, which results in variations of the Crigler-Najjar syndrome