Chapter 73 Penetrating Spinal Cord Injuries
Penetrating spine injury is a major cause of spinal cord injury (SCI) in the United States. Gunshot injuries have been reported to be the third leading cause of SCI.1 Stab wounds and other penetrating injuries tend to occur less in the United States than in some other countries. In South Africa, they account for 25% of all SCIs.2
Military versus Civilian Gunshot Injuries
Most experience with the management of penetrating SCIs has been gained during wartime. During World War I, survival was uncommon after a complete myelopathy (72% mortality). Treatment of these injuries consisted of laminectomy for incomplete myelopathy and debridement of the entry and exit wounds for complete myelopathy.3 A high operative mortality rate (62%) added to the dismal outcome.
During World War II, advances were made in trauma resuscitation and therapy. These advances dramatically decreased the mortality from penetrating SCIs.4–6 Some surgeons reported neurologic improvement in patients who were managed surgically.7 During the Korean War, most patients with penetrating SCIs underwent surgical exploration. There were reports of significant improvement.8 Further improvements were made in trauma resuscitation, evacuation, and surgical treatment during Operation Iraqi Freedom and Operation Enduring Freedom.9 The treatment of civilian penetrating SCIs, however, has generated less optimism than previous military reports have.10–14 Despite these findings, some authors have demonstrated benefit with early surgical intervention following civilian gunshot wounds.15 This is likely related to the pathophysiology of this type of injury.
Military weapons fire high-velocity missiles, while civilian weapons (typically handguns) fire low-velocity missiles. The pathophysiology of the SCI differs on the basis of velocity. High-velocity missiles may produce SCI by a concussive effect of the bullet passing close to, but not through, the spinal canal.16 Most SCIs caused by high-velocity missiles fit this pattern. These types of injuries may have a slightly better prognosis. Low-velocity missiles are more likely to injure the spinal cord directly, without a significant concussive effect; therefore, the prognosis for recovery is worse owing to the direct cord injury. This phenomenon may also explain the large percentage of civilian gunshot SCIs that present as complete myelopathies.10,12,17,18
Impalement Pathophysiology
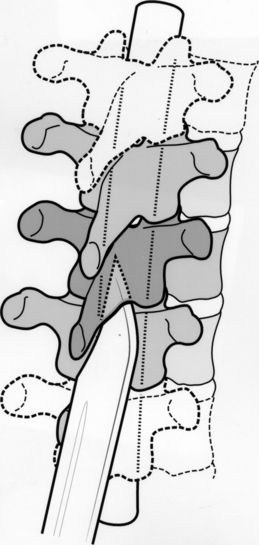
A weapon (knife) that penetrates the spinal canal may damage the spinal cord directly or indirectly. The direct injury may range from a dural tear to a total cord transection. Indirectly, there may be spinal cord contusion from the weapon impacting the cord against the bony spinal canal. The anatomy of the spinal canal may protect the spinal cord from a complete transection (Fig. 73-1). The weapon usually enters the spinal canal in the gutter between the spinous process and transverse process, thus leading to an incomplete SCI. Classically, the Brown-Séquard syndrome or a variant results.19
Resuscitation
The initial management begins with advanced trauma life support measures. The airway should be evaluated and secured. If necessary, endotracheal intubation should be performed. Oral intubation using manual in-line traction has been shown to be both safe and effective in patients with suspected SCI.20 Tracheostomy is indicated if the injury involves the trachea or larynx.21 Chest radiographs and arterial blood gas analysis (if indicated) should be part of the initial evaluation. The incidence of associated visceral injuries may be as high as 25%.22 These injuries, such as pneumothorax or vascular injury, must be sought early, as their treatment takes priority over spinal cord or spinal column injury.
The patient’s early course may be complicated by hypotension, which may be due to blood loss (hypovolemia) or to neurogenic shock from the loss of sympathetic vasomotor tone. Determining the exact cause of the hypotension is often difficult in the acute setting. However, tachycardia and cool extremities are often observed with hypovolemia, while bradycardia is often observed with spinal shock.19 The treatment for either condition is aggressive volume resuscitation. A central venous catheter is often helpful for monitoring the volume resuscitation. If the hypotension persists despite adequate intravascular volume replacement, vasopressor agents such as phenylephrine or dopamine should be employed. Vagolytic agents such as atropine may also be used. An indwelling pulmonary artery catheter may be useful if hypotension persists despite the use of vasopressor agents. Enthusiasm for the use of these catheters has waned lately.23
A Foley catheter should be placed. This allows bladder decompression and assists with gauging of the effectiveness of volume resuscitation. It also decreases the likelihood of subsequent urologic complications.19
Once the patient is stable from a cardiopulmonary standpoint, a more thorough history and physical examination should be performed. Information about the mechanism of injury and the caliber of the weapon should be obtained. The physical examination should note whether the patient has suffered a complete or incomplete myelopathy. If the injury is incomplete, the level of the SCI should be noted. The entry and exit sites should be inspected, and notation of cerebrospinal fluid (CSF) or foreign material should be made.7
Treatment of non-neurologic injuries is of primary importance because such treatment is usually lifesaving (rather than function-preserving).19 Because the course that a penetrating object takes within the torso is unpredictable, there may be an associated visceral injury.19 A trauma surgeon should assist with the evaluation for such potential injuries. Explorations of the neck, chest, and abdomen take precedence over spine surgeries.24
Some clinicians advocate exploration for wounds that penetrate the platysma, whereas others advocate the individualization of surgical planning.19 The two approaches appear equally effective if injuries to the great vessels, upper airway, and upper gastrointestinal tract can be ruled out via angiography, endoscopy, or swallowing studies.25–28
Pharyngeal perforation carries the risk of osteomyelitis.21,28,29 There are divergent views on the appropriate management of pharyngeal perforation. Some authors advocate broad-spectrum antibiotics, debridement of bone and soft tissue, drainage, and immobilization.21 Others have reported a lower infection rate with neural decompression and debridement of the wound.30
Radiographic Evaluation
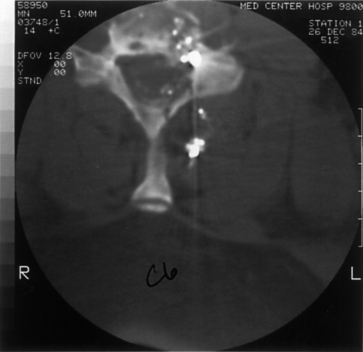
Initial evaluation should begin with routine radiographs. Fractures and bullet fragments may be seen (Fig. 73-2). A CT through the area of involvement should be performed next. This modality is generally superior to plain radiographs for the evaluation of the injury and for localizing the fracture or bullet fragments (Fig. 73-3). Compressive lesions may be identified with routine CT imaging. Bone and/or bullet fragments compressing the thecal sac may be identified. The aforementioned will also give the surgeon a sense of spinal stability or instability. CT myelography may be used to assess or confirm neural compression. This modality may also aid in the evaluation of a CSF fistula. If there is a question of spinal instability, passive flexion/extension radiographs may be used, but only in an awake, alert patient in whom there is no neurologic deficit.
MRI may also be used in the evaluation. There will be artifacts from the bullet fragments, but valuable information, such as the presence of extradural hematoma, disc herniation, or spinal cord contusion, may be gained. There is a risk of fragment migration in the magnetic field, so only patients for whom the information gained would have been difficult to obtain with other imaging modalities should undergo MRI.31