Chapter 36 Neuro-ophthalmology
Afferent Visual System
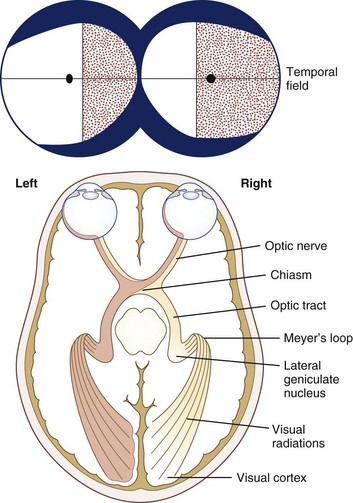
From a conceptual standpoint, it is useful to consider vision as having two components: central or macular vision (high acuity, color perception, light adapted) and peripheral or ambulatory vision (low acuity, poor color perception, dark-adapted). Light, refracted by the cornea and lens, then focuses on the retina. For the best possible vision, the object of regard must focus on the fovea, which is the most sensitive part of the macula. The cone photoreceptors, which mediate central and color vision, are greatest in density at the fovea. The cone system functions optimally in conditions of light adaptation. Visual acuity and cone density fall off rapidly as eccentricity from the fovea increases. For example, the retina 20 degrees eccentric to the fovea can only resolve objects equal to Snellen 20/200 (6/60 metric) optotypes or larger. Rod photoreceptors are present in highest numbers approximately 20 degrees from the fovea and are more abundant than cones in the more peripheral retina; rods function best in dim illumination. The total extent of the normal peripheral visual field in each eye is approximately 60 degrees superior, 60 degrees nasal, 70 to 75 degrees inferior, and 100 degrees temporal to fixation (Fig. 36.1) (see Chapter 14).
Each eye sends visual information, transduced by the retina, to both hemispheres of the brain by the optic nerves, each of which contains over 1 million axons. Axons that arise from the ganglion cells of the nasal retina of each eye cross in the optic chiasm to the contralateral optic tract. Axons from the temporal retina do not decussate at the chiasm. The percentages of crossed and uncrossed axons in the human optic chiasm are approximately 53% and 47%, respectively. Because of the optical properties of the eye, the nasal retina receives visual information from the temporal visual field, while the temporal retina receives visual information from the nasal visual field (see Fig. 36.1). Similarly, the superior retina receives information from the inferior visual field, and vice versa. These points are clinically important in evaluating visual loss (see Chapter 14).
Visual information stratifies further in the lateral geniculate nucleus (LGN), which is the only way station between the retinal ganglion cells and the primary visual cortex. The LGN, a portion of the thalamus, has six layers. Axons from ipsilateral retinal ganglion cells synapse in layers 2, 3, and 5; contralateral axons synapse in layers 1, 4, and 6. Layers 1 and 2 of the LGN are the magnocellular layers and receive input from M retinal ganglion cells. The magnocellular pathway is concerned mainly with movement detection, detection of low contrast, and dynamic form perception. After projecting to the primary visual cortex (visual area 1, V1, or Brodmann area 17), information from the M pathway is distributed to V2 (part of area 18) and V5 (junction of areas 19 and 37). Layers 3 to 6 of the LGN are the parvocellular layers and receive input from retinal P cells, which are color selective and responsive to high contrast. Information from the P pathway is distributed to V2 and V4 (fusiform gyrus) (Trobe, 2001). Superior fibers that leave the LGN go straight back to the primary visual cortex; inferior fibers loop anteriorly around the temporal horn of the lateral ventricles (Meyer loop). Since these fibers pass close to the tip of the temporal lobe, temporal lobectomy sometimes damages these fibers causing a “pie in the sky” homonymous visual field defect.
The primary visual cortex (striate cortex, area V1, or Brodmann area 17) is in the occipital lobe. Fibers from the macula project to the visual cortex closest to the occipital poles (each fovea appears to project to both occipital lobes), while fibers from the peripheral retina project to the visual cortex lying more anteriorly. The nonoverlapping part of the most peripheral temporal visual field (monocular temporal crescent) arises from unpaired crossed axons from the nasal retina that project to the most anteromedial part of the visual cortex. The primary visual cortex has interconnections with visual association areas concerned with color, motion, and object recognition (Trobe, 2001).
Neuro-ophthalmological Examination of the Afferent Visual System
Examination of Visual Acuity
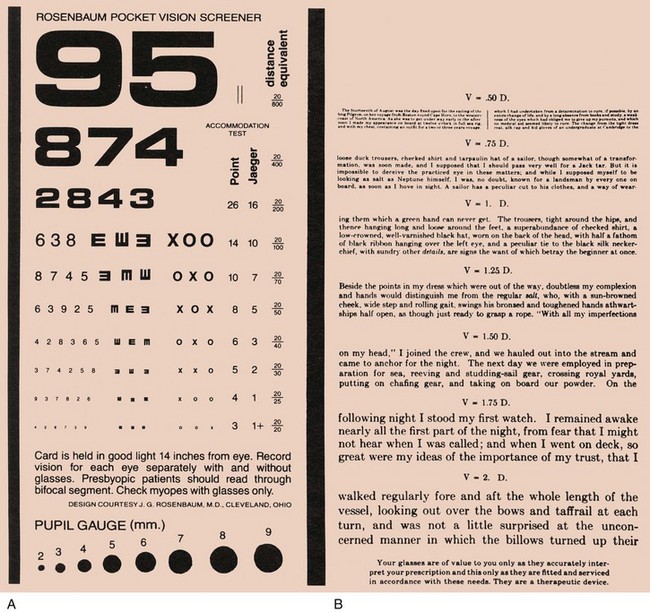
Visual acuity is the spatial resolution of vision. Visual acuity should always be measured with each eye individually and with the best possible optical correction (i.e., with the patient’s glasses); other optical means such as the pinhole device or a refraction may be needed (Wall and Johnson, 2005). The resultant measure, called best-corrected visual acuity, is the only universally interpretable measurement of central visual function. Ideally, always measure vision both at a standard distance (usually 20 feet or 6 m) and at near (usually 0.33 m). The notation 20/20 (6/6 metric) means the patient (numerator) is able to see the optotypes seen by a normal subject at 20 feet (denominator). A vision of 20/60 (6/18 metric) means that the patient sees an optotype at 20 feet that a normal person would see at 60 feet.
When measuring near vision, the reading card should be held at the specified distance of 14 inches (or 0.33 m) to control for variation in image size on the retina. The medical record should clearly specify if a nonstandard distance is used. Two types of near cards are readily available; one has numbers and the other has written text (Fig. 36.2). Both are useful, but in neurological practice, a near card with text measures not only visual acuity but also reading ability to some degree. A disparity between the measurements from the two types of near card might suggest a disturbance of some other cortical function such as language function (see Chapter 11).
Light-Stress Test
In some disorders of the macula, abnormalities are undetectable with the direct ophthalmoscope. The light-stress (or photo-stress) test is a useful method for determining whether reduced visual acuity is a consequence of macular dysfunction (Wall and Johnson, 2005). Prior to the test, the best-corrected visual acuity is measured in each eye. Then, with the eye with decreased vision occluded, the other eye is exposed to a bright light for 10 seconds. Immediately thereafter, the patient is instructed to read the next larger line on the eye chart, and the recovery period is timed. The same procedure is followed for the eye with decreased vision, and the results are compared. Fifty seconds is the upper limit of normal for visual recovery, although most normal subjects recover within several seconds. In patients with macular disease, the recovery period often takes several minutes.
Color Vision Testing
Dyschromatopsia, especially if asymmetrical between the eyes, is a good indication of optic nerve dysfunction, but it can also occur with retinal disease (Almog and Nemet, 2010). Symmetrical acquired dyschromatopsia might indicate a retinal degeneration, such as a cone-rod dystrophy. Congenital dyschromatopsia occurs in about 8% of men and 0.5% of women.
Examination of the Pupils
Examination of the pupils involves assessing pupil size and shape, direct and consensual reactions to light, near reaction, and the presence or absence of a relative afferent pupillary defect (RAPD). If a difference in pupil size (anisocoria) is noted, look for ptosis and ophthalmoplegia, keeping in mind the possibility of a Horner syndrome or third cranial nerve palsy. Record findings in an easily understood format (Table 36.1).
Measurements of pupil size and light reaction are made in dim illumination with the patient fixating on an immobile distant target. If there is anisocoria, it is useful to measure pupil size in darkness and bright ambient light. Anisocoria due to oculosympathetic paresis (Horner syndrome) is often greater in the dark, because the affected pupil does not dilate well. Conversely, anisocoria due to parasympathetic denervation (e.g., Adie tonic pupil) is often more evident in bright light, because the affected pupil does not constrict well (see Chapter 16).
The observation of an RAPD (formerly called a Marcus Gunn pupil) is an invaluable indication of a conduction defect in the optic nerve. A difference in pupillary reaction is best elicited by alternately illuminating the pupils by swinging a flashlight between them at a frequency of about once per second—hence the name, swinging flashlight test. The swinging flashlight test compares the direct and consensual reactions in the same eye. Normally these reactions are equal. However, in patients with an optic neuropathy, because of reduction in the direct reaction as compared with the consensual reaction, the pupil dilates when re-illuminated. Box 36.1 and Fig. 36.3