CHAPTER 12 MOTOR SPEECH AND SWALLOWING DISORDERS
Motor speech relies on a complex interaction of the resonatory, respiratory, articulatory, and laryngeal neuromuscular systems.1 Coordination of the neuromuscular components of the latter three systems is also essential for the execution of swallowing. Different neurological disorders affecting motor speech production may give it particular features that aid in anatomically localizing the disorders; there is, frequently, also an associated abnormality of the swallow mechanism.2
ANATOMY
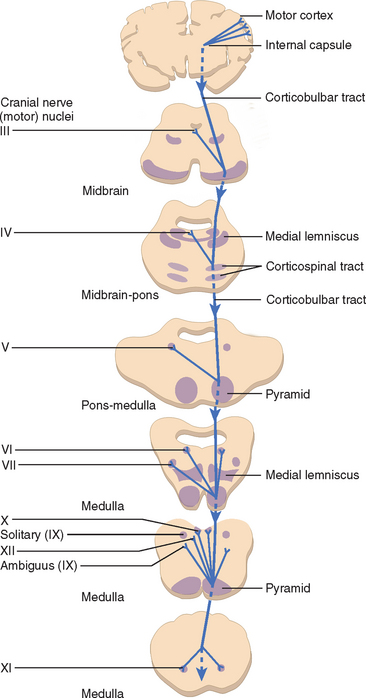
Corticobulbar Tract
Upper motor neuron (UMN) pathways responsible for motor speech and swallowing originate in the motor cortex in each cerebral hemisphere and descend through the genu and posterior limb of the internal capsule, via the cerebral peduncle, to the pons and medulla (and upper cervical cord for the spinal nucleus of cranial nerve XI). At these levels, they synapse with the various lower motor nuclei responsible for supplying the bulbar muscles: cranial nerves V, VII, IX, and X; the cranial portion of cranial nerve XI (which contributes to the motor component of the vagus nerve [cranial nerve X]); and cranial nerve XII. The UMN pathways are known as the corticobulbar tracts, and are generally bilateral (contralateral and ipsilateral). There are, however, important exceptions, such as cranial nerve XII and the lower facial muscles, which receive their upper motor connection predominantly from contralateral corticobulbar fibers (Fig. 12-1). Emotional involuntary movements and voluntary facial movements may at times be clinically dissociated, which suggests that a separate supranuclear pathway for control of involuntary facial movements probably also exists. These fibers do not pass through the internal capsule, and it appears that the right cerebral hemisphere is dominant for expression of facial emotion.3
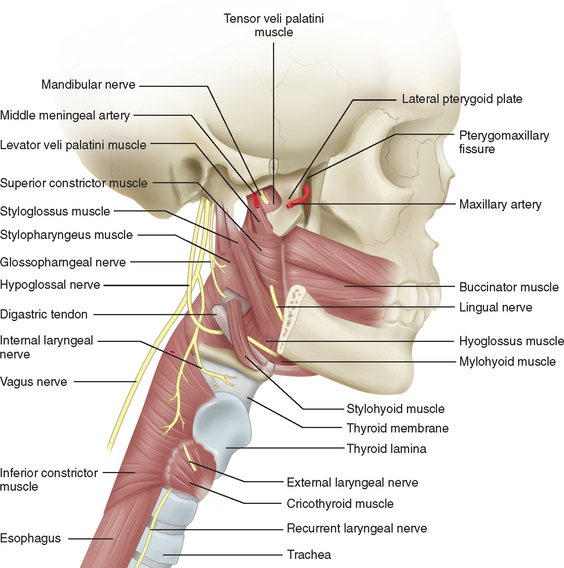
Lower Cranial Nerves
Assessment of the bulbar cranial nerves and their function is extremely important when disorders of motor speech and swallowing are considered. These cranial nerves exit the brainstem at the level of the pons or medulla and leave the cranium through the skull base, traveling either through the retropharynx or across the angle of the mandible to innervate the muscles of the face, mouth, soft palate, pharynx, and larynx (Fig. 12-2). The trigeminal nerve (V) innervates the muscles of mastication and the tensor veli palatini and communicates sensation from the face, mouth, teeth, mucosal lining, and anterior two thirds of the tongue (via the lingual nerve). The facial nerve (VII) supplies the muscles of facial expression and conveys taste from the anterior two thirds of the tongue (via the chorda tympani and lingual nerve). The glossopharyngeal nerve (IX) conveys taste from the posterior one third of the tongue, as well as sensation from this portion of the tongue, the fauces, the pharynx to about the level of the epiglottis, and the eustachian tube. It also provides the motor supply to the stylopharyngeus and, in part, to the superior and middle pharyngeal constrictor muscles through a contribution to the pharyngeal plexus. The vagus nerve (X) conveys sensation from the tympanic membrane, pharynx, larynx, and esophagus. One of its branches, the recurrent laryngeal nerve, innervates all the intrinsic muscles of the larynx other than the cricothyroideus, whereas the superior laryngeal nerve innervates the cricothyroideus and conveys sensation from the larynx and the base of the tongue. The vagus also contributes to the innervation of the pharyngeal constrictors through the pharyngeal plexus. The hypoglossal nerve (XII) innervates the muscles of the tongue, with the exception of the palatoglossus, which is supplied by the vagus nerve.4
Bulbar and Pseudobulbar Palsies
UMN lesions affecting the corticobulbar tracts can be distinguished from disorders of the lower cranial nerves or their nuclei by the distinctive changes to speech that are associated with damage to these tracts, described in the next sections. The features of such corticobulbar tract lesions are collectively known as pseudobulbar palsy, a term used to distinguish them from the true bulbar palsy, which results from pathology affecting the lower cranial nerves or their nuclei. There may, in addition to speech, be other distinguishing features on examination, typical of all UMN disorders, such as increased muscle tone (as evidenced by slow side-to-side movement of the tongue) and exaggerated reflexes (gag or jaw reflex), without signs of muscle wasting, atrophy, or fasciculations. A patient with bulbar palsy, in contrast, has the hallmarks of a lower motor neuron (LMN) disorder: namely, muscle weakness, wasting, and fasciculations.
DISORDERS OF MOTOR SPEECH
Verbal communication involves a sequence of processes culminating in the motor execution of a cortically determined set of instructions to produce speech. Disorders of this complex pathway have been classified as aphasia, apraxia of speech (AOS), and dysarthria, each of which may then be subclassified further, depending on the nature of the dysfunction and its cause. Dysarthria and AOS are termed disorders of motor speech because they exist at the output level of the motor system and disrupt only sound output, sparing semantics and syntax. The patient has a full knowledge of words they are finding difficult to articulate. This serves to distinguish these disorders from aphasia, which is defined as “a disorder of linguistic processing characterized by a disturbance in the comprehension and formulation of language caused by dysfunction in specific brain regions.”5,6 Aphasia is discussed in detail in Chapter 3 and is not considered further here.
Apraxia of Speech
Abnormalities of speech after neurological insult were subdivided into aphasias and dysarthrias before the contribution of Darley, who with colleagues delivered an unpublished paper on the topic in 1969.7 In this lecture, Darley was the first to use the term apraxia of speech and to attribute a specific disorder of speech—interposed between aphasia and dysarthria—to impaired motor programming,8,9 The term apraxia had long been used in other contexts to describe the inability to carry out a motor command despite normal comprehension and the normal ability to carry out the motor act in another context, such as by imitation or with use of a real object.10
This three-level model of sound-level speech production disorders survived without challenge until the late 1990s. In 1997, van der Merwe10 proposed a four-stage model in which there was an explicit division between “speech motor planning” and “speech motor programming.” Previously, these terms had been used interchangeably. In this model, speech motor planning involves two stages (linguistic-symbolic planning and motor planning) and refers to the planning of the temporal and spatial goals of the articulators. This is followed by a third stage, speech motor programming, which refers to the selection and sequencing of motor programs for the movements of the individual muscles of these articulators (including the vocal cords). The final stage is the execution stage, which refers to the actual realization of speech on an articulatory level. This model makes a clear assignment of AOS to the motor level of impairment as a disorder of speech motor programming.6 Aphasias are disorders of the stages of linguistic-symbolic and motor planning in this system, and dysarthrias are disorders of the execution stage.
AOS is a syndrome in which a sequence of single sounds (phonemes), especially consonant sounds, are disrupted and inconsistently misarticulated, in contrast to the consistently abnormal articulation of dysarthria. A further identifying feature of AOS is that comprehension and automatic or reactive speech are normal, but volitional or purposive speech contains substitutions, additions, prolongations, and reversal of phonemes.9 The sufferer repeats incorrect initial phonemes, words, or phrases, which results in a labored, perseverative speech pattern. This may superficially resemble stuttering, but the effortful blocking on a correct initial phoneme typical of stuttering is not seen. AOS, according to this definition, is commonly encountered during attempted speech production in the aphasias, and the sites of lesions that produce a nonfluent aphasia and AOS may overlap.6 One literature review suggests that cortical-subcortical lesions in the lower part of the left precentral gyrus in most right-handed persons, and a lesion of the corresponding region in the right hemisphere in some left-handed individuals, are the most likely to produce AOS.11 A lesion in Broca’s area may cause a combined syndrome of AOS, orobuccal dyspraxia, and nonfluent aphasia. This symptom complex is frequently referred to as Broca’s aphasia.
Dysarthria
Dysarthria is defined as a group of speech disorders resulting from disturbance in the control of speech mechanisms that, in turn, results from damage to the central or peripheral nervous systems, including muscles and neuromuscular junctions.12 There is consistently abnormal articulation of phonemes during both automatic and volitional speech. It is caused by the impaired functioning of one or several of the components of the motor speech subsystems (respiration, phonation, resonation, and articulation). Dysphonia is a subset of dysarthria, and the term refers specifically to a disruption of phonation, resulting in an abnormal voice sound without disturbance of articulation. The definition encompasses all disorders of voice sound, both organic and psychogenic.
Speech is produced by co-coordinated contraction of the muscles of the larynx, pharynx, and tongue, linked to the expiration phase of respiration. At a cortical level, articulation requires the coordinated bilateral movements of the muscles concerned, which is effected by fibers passing from the inferior region of the left lateral frontal lobe to the corresponding region of the right hemisphere via the corpus callosum.13
The motor speech system relies on the normal function of the various elements of the nervous system involved in the control of motor speech: namely, UMNs and LMNs; the coordinating and regulating influence of extrapyramidal, cerebellar, and sensory pathways; and the final output through neuromuscular junctions and muscles.14 Disorders affecting each part of this extensive control, effector, and feedback network have distinct effects on speech, which can be identified through the clinical examination. The nature of the change in speech therefore has localizing significance, which can be used to classify the motor speech disorder as AOS or a particular type of dysarthria.
Upper Motor Neuron Lesions
In view of the bilateral nature of the majority of the UMN input to the cranial nerves responsible for speech, unilateral UMN lesions produce a relatively mild dysarthria that reflects primarily weakness and some loss of skilled movement. Bilateral UMN lesions have a much more severe effect that reflects both bilateral weakness and loss of skilled movement, as well as an increase in muscle tone (spasticity).15 The dysarthria accompanying such pathology is known as spastic dysarthria and is one of the features of pseudobulbar palsy. The speech changes characteristic of this condition include slow rate of speech, imprecise consonants, distorted vowels, hypernasality, monotone pitch, short phrases, and a strained-strangled quality to the voice. A number of neurological conditions can affect these pathways and cause a spastic dysarthria (Table 12-1).
TABLE 12-1 Examples of Neurological Conditions Causing Dysarthria or Neurogenic Dysphagia
* These are uncommon causes of dysarthria; they more commonly cause dysphagia. dHMN-VII, distal hereditary motor neuropathy type VII; FALS, familial amyotrophic lateral sclerosis; HMSN-IIC, hereditary motor sensory neuropathy type IIC.
Lower Motor Neuron Lesions
Which exact speech disorder accompanies a LMN lesion depends on the nerve or nerves involved. A brainstem stroke, for example, may affect several cranial nerves, whereas a mediastinal mass may affect only the left recurrent laryngeal nerve. Patients are usually able to compensate if damage is unilateral, whereas a bilateral lesion usually results in a severe impairment. The principal causes of flaccid dysarthria are listed in Table 12-1.
Cerebellar Disorders
Disorders involving cerebellar pathways cause loss of the normal coordination and timing of speech output. This can lead to random breaks between words and syllables, vowel distortions, prolongations of sounds, and the use of equal stress on each syllable, thereby creating a “rambling” or “scanning” quality to the speech (ataxic dysarthria) (see Table 12-1). The dysarthria accompanying focal cerebellar lesions tends to occur particularly with lesions of the vermal and (usually) left dorsal intermediate zone of the cerebellum, whereas it is typically not seen with lateral neocerebellar lesions.13
Extrapyramidal Disorders
Extrapyramidal disorders, such as Parkinson’s disease or Huntington’s disease, result in hyperkinetic or hypokinetic dysarthria. The most common dysarthria accompanying Parkinson’s disease is a hypokinetic dysarthria, characterized by rapid speech rate (festination), slurring of words and syllables, and trailing off at the end of sentences. The voice is soft and monotonous, without the usual inflections. The speech disorder accompanying Huntington’s disease is hyperkinetic dysarthria, which results in an uncontrolled loud, harsh voice, poorly coordinated with breathing. Chorea and myoclonus may cause abrupt interruption between or within words by the superimposition of abnormal respiratory, phonatory, or articulatory movements.15
Dysphonia
Dysphonia may also be produced by conditions that cause weakness of the respiratory muscles—such as Guillain-Barré syndrome or a high cervical spinal cord lesion—because insufficient airflow is produced for phonation.15 Abnormalities of phonation become more apparent the longer the subject speaks, and asking the patient to read aloud from a magazine is a good means of bringing out these features.
Spasmodic Dysphonia
Spasmodic dysphonia appears to result from a dystonia restricted to the phonatory apparatus, but it can occasionally co-occur with other dystonias, such as writer’s cramp and blepharospasm. More sufferers are women, and speaking gradually becomes more of an effort. Usually, attempts to speak result in co-contraction (adduction) of the vocal folds, causing a strained, strangled-sounding voice. In rare cases, the problem may be a breathy, soft voice; in these patients, the dystonia causes abduction of the vocal cords. In either instance, other activities involving use of the same muscles, such as swallowing and singing, are usually unimpeded.15
Nonorganic Disorders of Voice
Voice disorders may have a psychological basis, rather than being the result of pathology affecting neural pathways or muscular control. The most common psychogenic speech disorders affect voice, fluency, or prosody. Prosody is the term used to describe all the variations in time, pitch, and loudness that accomplish emphasis, lend interest to speech, and characterize individual and dialectical modes of expression.16 Psychogenic speech disorders are not unusual and can account for up to 5% of acquired communication disorders.15 The most common is aphonia (hoarseness), but psychogenic spasmodic dysphonia, particularly adductor spasm, is also encountered.