Chapter 6 Management of Alopecia
Summary
Introduction
With current techniques, hair transplants can look totally natural and without signs that a procedure has been performed.1 Hair transplantation has, however, a poor reputation because so many patients in the past have had less than acceptable results.2 Scalp reconstruction with flaps and excisions and the use of tissue expanders for male patients with genetic hair loss are now rarely used except in the management of difficult secondary cases.3–20
Improvements in results in the past 15 years are due to the work of many in the field, and in particular, Dr Carlos Uebel from Brazil,21,22 who was one of the first to popularize the use of small natural-appearing grafts in large numbers performed at a single session. Today, rather than transferring a few hundred grafts at each session requiring numerous procedures, it is not unusual to transfer 1500, 2000, and even 3000 grafts in a single session.
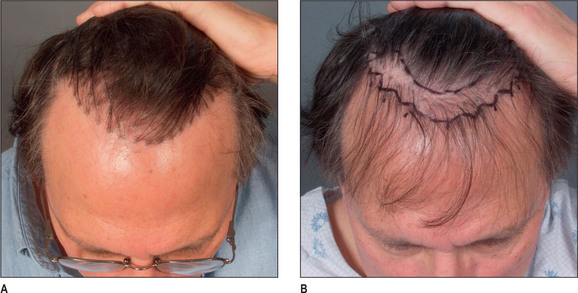
Importance of Type of Graft and Design of a Natural Hairline
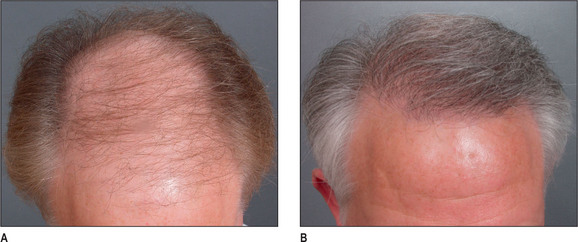
A discussion of transplantation usually refers to micro or mini grafts.23 Current nomenclature uses the term follicular grafts,24–26 which are clusters of one to three hairs that emerge from the scalp as a unit. Grafts often used to contain 10, 20, and even 40 hairs per each graft, so creating an unnatural appearance (Fig. 6.1A&B), and the hairline was often poorly designed. A successful and aesthetically pleasing hair restoration is as demanding as any other aesthetic facial procedure.
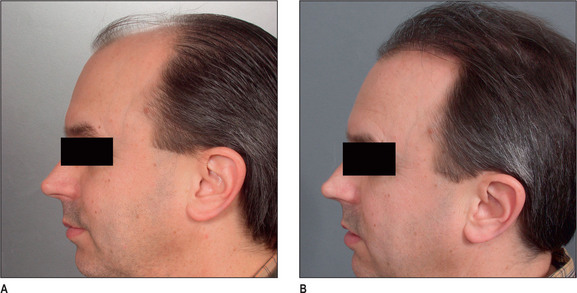
The frontotemporal recession is an important component of creating a mature natural hairline in males.27 This anatomic landmark is formed by the junction of two lines, consisting of the frontal and temporal hairlines, which converge in an acute angle. It is critical in creating a natural-appearing male hair transplant to maintain this normal frontotemporal recession. In hair restorations where the frontotemporal angle is not created, the patient frequently has an un-natural result, creating either a feminine or immature male hairline.
Other important components of a natural hairline include the transition anteriorly from fine to thicker hair with increasing density, and a significant degree of irregularity along the hairline margin. Normal hairlines should not appear straight and regular. Perfectly straight hairlines are characteristic of unnatural-appearing hair transplants. Unsatisfactory results with hair transplants usually demonstrate a fundamental lack of knowledge of these critical points required to create a natural-appearing hairline.28
Indications
Most patients seeking hair restoration due to genetic hair loss are male. Approximately 15% of patients who have primary alopecia in my current practice are women and demonstrate typical genetic pattern hair loss. The other main group of patients have had previous hair transplantation with poor results;29–31 these patients are more difficult to treat and fall into two groups:
Most women with hair loss may not be good candidates for hair transplants and may suffer from metabolic autoimmune disorders
One of the main indications in women is secondary or traumatic alopecia after procedures such as facelifts or forehead lifts. In these patients hair loss results from excessive tension or undermining of the hair follicle.32 Such women are ideal for hair transplantation because scars or abnormally high hairlines can be readily corrected. The most common area needing hair transplantation is probably the temporal and preauricular area.
Male Androgenic Alopecia
In most men, hair loss is related to androgenic alopecia. This form of alopecia is a response to androgens, which reduce the rate of hair growth as well as the diameter of the hair shaft.33 Also, the growth phase of hair referred to as anagen is shortened. It is believed that testosterone is converted by the enzyme 5-alpha reductase to dihydrotestosterone (DHT),34 which targets the hair and causes genetic hair loss. In most men with hair loss, the hair follicles in the frontal and crown regions appear to be most susceptible to DHT, leading to androgenic alopecia. In most patients, 30–50% of the hair has been lost before it becomes apparent. As the average normal head has 100 000–150 000 hairs, a significant amount of hair loss is necessary before it becomes apparent.
Female Hair Loss
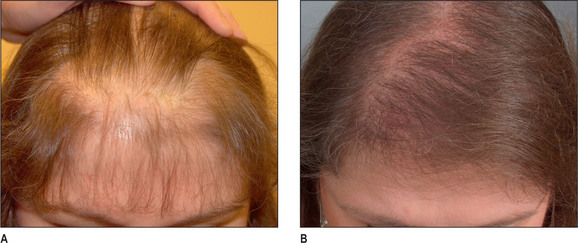
Female hair loss is frequently more diffuse, and many women are not good candidates for hair restoration because of a lack of good donor hair.35 However, a subgroup of women present with hair loss similar to androgenic alopecia36 and usually have good hair density in the lateral and posterior areas of the scalp. Many of these women have a history compatible with that seen in male pattern hair loss and report many family members with either thin hair or balding scalps.
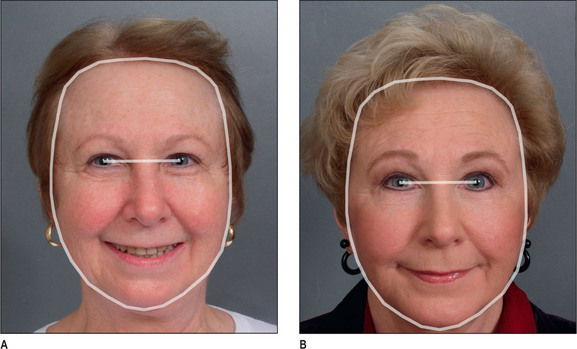
Unlike male pattern hair loss of the genetic form, women with genetic hair loss tend to maintain a low frontal hairline with an anterior margin of hair (Fig. 6.2A&B). This is very different from men where there is progressive elevation of the frontal hairline and increasing temporal recession over time. Women, however, frequently maintain a frontal hairline for life, and this factor requires hair transplantation to be performed, beginning from the frontal hairline and continuing posteriorly to fill in the defect.
Patient Selection
As in all areas of aesthetic surgery, realistic expectations of what can be accomplished with hair restoration are important.
Preoperative History and Considerations
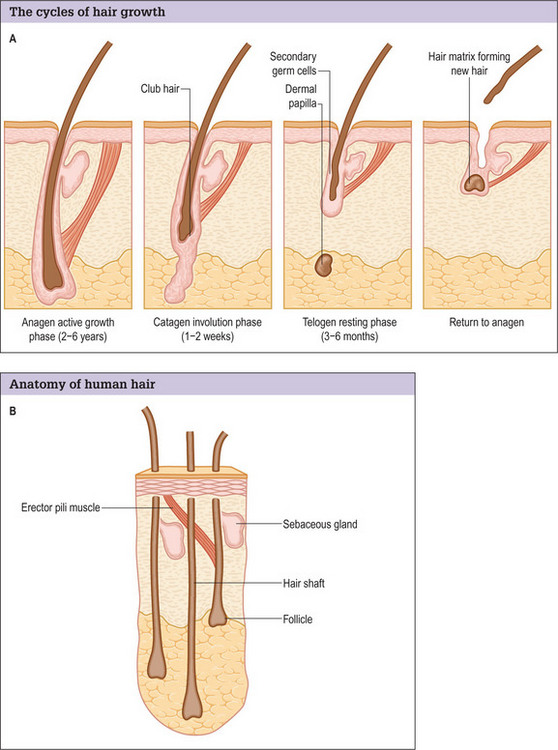
Hair normally passes through three cycles (Fig. 6.3A&B).37
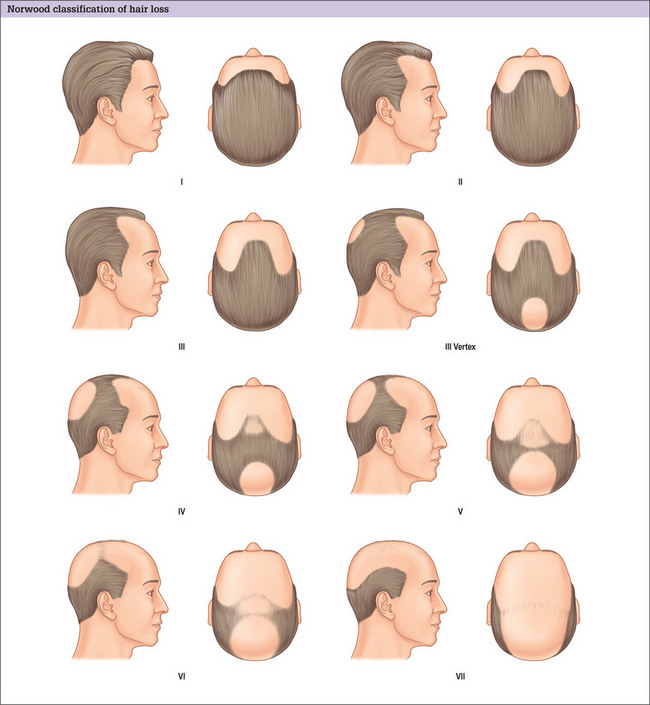
Classification of Alopecia
The major classification of alopecia used by most physicians today is the Norwood classification, which is a modification of Hamilton’s original description (Fig. 6.4).38 There are many other classifications, but most divide baldness into six to seven primary groups, with sub-groups included.39,40 These classifications can be useful, but most patients do not fit into a single specific classification or hair loss type exactly.
Ludwig has described a system for classifying androgenic alopecia in women.41
Hair Type
Goals of Transplantation
Hairline
It is important that the patient understands that the goal is to create a hairline that is harmonious with their facial characteristics and to create balance. One term that is frequently used is facial framing (Fig. 6.6A&B). This creates a more balanced appearance in the anatomic components of the face. Typically, the face can be divided into equal thirds, but in a patient who has a receding hairline, the eyes appear to have a more centralized appearance; creating a lower hairline produces better balance by framing the facial characteristics.
During the consultation, it is useful to draw the proposed transplantation pattern on the patient’s scalp and to allow the patient to see it (i.e. the most appropriate hairline) in a mirror. Patients given a marking pen will frequently draw the hairline in a relatively low position, which is usually not appropriate because a relatively youthful hairline now may lead to problems and dissatisfaction later. A demonstration of the Norwood classification allows patients to understand the normal nature of androgenic alopecia as hair recedes. A natural hairline will age appropriately with the patient as temporal recession and elevation in the frontal hairline progresses. For most patients the frontal hairline should be at least 8–10 cm above the glabella (Fig. 6.7A&B).