Chapter 95 Kyphotic Cervical Deformity
Kyphotic cervical spine deformity can be caused by advanced degenerative disease, systemic arthritides, trauma, neoplastic disease, and postsurgical (iatrogenic) causes.1 The most common cause is postsurgical.2
The postsurgical development of cervical kyphosis can follow both ventral and dorsal approaches. Following ventral approaches, kyphosis may develop secondary to pseudarthrosis or failure to restore anatomic cervical lordosis during surgery. Ventral discectomy without graft placement is associated with a 33% rate of kyphosis.3 Following dorsal surgery, kyphosis may develop and progress secondary to disruption of the dorsal elements (interspinous ligaments, laminae, and facet joints). The incidence of kyphosis after laminectomy ranges from 14% to 47%.4,5
Cervical kyphosis is biomechanically unfavorable for the cervical musculature. The kyphosis will tend to progress as axial loads of the head produce a bending moment through the moment arm of the cervical spine.6 This will often produce mechanical pain that improves when the patient is supine.7 Often, excessive degeneration of the cervical discs occurs that contributes to cervical pain. As the kyphosis progresses, the patient’s field of view, swallow, and respiration may be affected. The patient may develop low back pain and accelerated degeneration by hyperlordosing the lumbar spine to accommodate for the cervical deformity.
Clinical Presentation
Patients often present with mechanical neck pain. This pain is typically worse in the upright position and with exertion and improved with rest and recumbancy. Patients can also present with radiculopathy or myelopathy from compression on neural elements. As the kyphosis worsens, there is increased stress on the ventral spinal cord from tethering of the cord by the dentate ligaments. This may adversely affect the spinal cord vasculature and lead to worsened myelopathic symptoms.8,9 Patients with severe deformity may present with swallowing dysfunction and in some cases nutritional deficiency, compromise of horizontal gaze, and compromised breathing.10,11
Clinical Evaluation
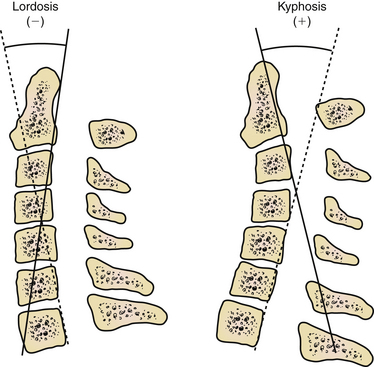
The deformity should be evaluated radiographically as well. Evaluate the cervical deformity using static upright and dynamic (flexion-extension) radiographs. The thoracic spine should be evaluated if deformity is suspected at the cervicothoracic junction. By using radiographs, the sagittal angle of the deformity may be measured (Fig. 95-1), and other abnormalities may be identified, such as subluxation and pseudarthrosis. Pseudarthrosis and existing fusion can be better clarified by using thin-cut CT scan. The ability of the alignment of the cervical spine to be reduced can also be assessed with extension or supine radiographs. Standing long-cassette radiographs can be useful to assess overall sagittal balance. In designing the treatment strategy, thoracic hyperkyphosis, lumbar hyperlordosis, and ankylosed joints must be taken into account.
Deformity Correction Strategies
The cervical spine may be exposed to coronal plane, rotational, axial (subsidence), or, most commonly, sagittal plane deformation stresses. It is important to establish goals of treatment prior to surgery. Decompression of the neural elements should be the first priority. Most commonly, the surgical approach will address the compression directly, but occasionally, this is dealt with indirectly by deformity correction. Ferch et al.12 demonstrated an association of improved myelopathy with restored lordosis in cervical kyphotic deformity patients. Fusion at abnormal levels may also prevent damage to the cord from micromotion.
Sagittal plane deformity may be addressed ventrally,13–18 dorsally,19–21 or both.18,19,22–27 If there is imaging evidence of ventral compression, then a ventral procedure should be considered. If the deformity is fixed ventrally without dorsally fused joints, then a ventral decompression with fusion can be used to correct the kyphosis. If the dynamic radiographs demonstrate normal movement and a normal lordosis can be achieved in extension, then a dorsal surgical reconstruction can adequately address the pathology. If the deformity is fixed owing to dorsally fused joints (ankylosing), then a dorsal osteotomy can be used to correct the kyphosis.10,11,28 Finally, a flexible deformity can be corrected posturally or with traction and then be fused dorsally.
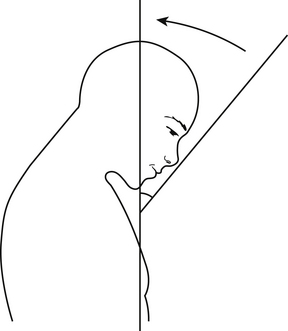
The goal for restoration of sagittal alignment is unclear. A definition of normal lordosis does not exist. However, Gore et al. measured lordotic angles in the cervical spine of patients with osteoarthritis using the perpendicular of the C2 and C7 vertebral bodies. Lordosis of 16 to 22 degrees was observed in men and 25 degrees in women.29 However, it is likely that if a patient is not restored to neutral or a lordotic posture, the deformity will continue to progress over time. Another useful measure, especially in rigid cervical kyphosis (e.g., ankylosing spondylosis), is the chin-brow vertical angle, which will help to determine whether the patient will be able to see the horizon (Fig. 95-2). Finally, overall sagittal and coronal balance is important. Ideally, the head should be balanced over the sacrum.
Ventral Strategies
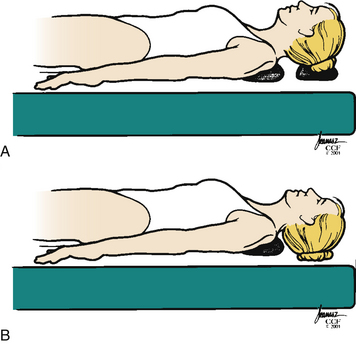
The ventral strategy uses both posture and biomechanical principles to correct the cervical deformity. Initially positioning the head on a towel or foam doughnut with the neck in a neutral or only slightly extended position allows adequate exposure for the approach but without compromising the spinal cord. After the decompression is complete, the towel or doughnut can be removed, allowing further extension of the cervical spine (Fig. 95-3).
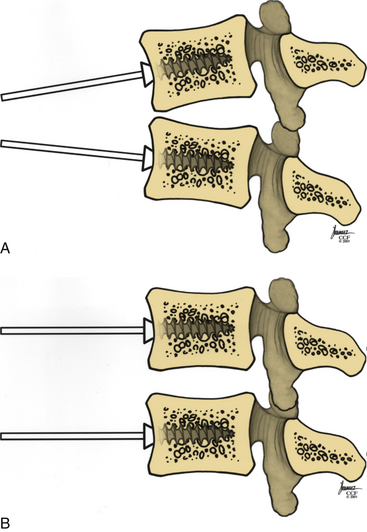
Distraction posts should be placed into the vertebral bodies in a convergent manner (Fig. 95-4A). This will allow distraction on the posts to provide further lordosis (Fig. 95-4B).
Long-segment corpectomies, greater than two vertebral bodies, have been used to correct ventral deformity. However, the authors believe that long-segment corpectomies should be avoided. Biomechanical studies show that three-segment corpectomies allow more movement than two-level corpectomies do.30 Long-segment corpectomies are more likely to fail at the terminal end because of the amount of force at the terminal screw-bone interface. Vaccarro et al. found that the early failure rate of two-segment corpectomies was 9% compared with 50% for three-segment corpectomies.31 In straight or kyphotic spines, corpectomies do not maintain as much sagittal angle correction as they do in lordotic spines.32
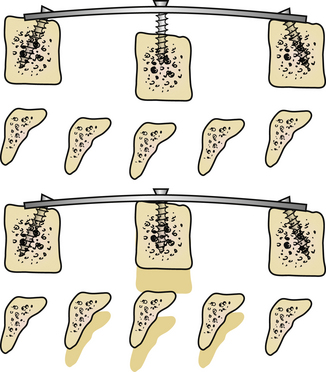
An alternative method for ventral correction is multilevel discectomy and fusion and/or a combined short-segment corpectomy. Leaving an intermediate vertebral body allows adequate decompression and provides additional intermediate fixation points for security of fixation and deformity correction (Fig. 95-5). Wei-bing et al.33 showed that two-level corpectomies had a higher rate of plate and graft migration requiring reoperation than did a combined construct of one-level anterior cervical discectomy and fusion (ACDF) plus one-level corpectomy. Oh et al.34 did not show a difference in clinical outcome between single-level corpectomy versus two-level ACDF.
The degree of correction required must be considered preoperatively to help plan the number of levels to be involved for deformity correction. Although this is often simply estimated, some recent studies may be helpful. Cabraja et al.35 found that a ventral or two-level corpectomy achieved a segmental correction of 6.2 degrees and an overall cervical lordosis correction of 8.8 degrees. However, using ventral correction only, they found that there was an approximately 2-degree loss of correction over an average 33-month follow-up period. Ferch et al.12 demonstrated that a ventral only approach can improve overall lordosis an average of 11 degrees. Eighty-five percent of the patients in their series were restored to neutral or lordotic alignments.
Dorsal Strategies
It is uncommon to use a dorsal strategy alone to correct cervical deformity because it is difficult to reduce a kyphotic deformity and achieve adequate lordosis from a dorsal approach alone. But if the deformity is flexible and no ventral decompression is required, then it should be possible to correct the deformity from a dorsal approach alone. If there is evidence of ventral compression, then a combined approach should be considered.
There are many instrumentation choices. The most common method is lateral mass fixation at the levels of C3-6. The C7 lateral masses are often not large enough to hold a screw, and screw placement often makes it difficult to align rods across the cervicothoracic junction. Lateral mass fixation might not be an optimal stabilizing anchor in some patients.20,23,36
It is also possible to use cervical pedicle screws for the dorsal correction of cervical deformity. Abumi et al.19 have demonstrated their usefulness in deformity correction, achieving a correction from 28.4 to 5.1 degrees of kyphosis with all patients achieving solid fusion. It should be emphasized that lordosis was not achieved with the dorsal procedure alone. Kotani et al.37 have demonstrated that these screw systems are biomechanically equivalent to combined ventral plate and dorsal wiring.