Chapter 4 Elbow Ultrasound
![]() Additional videos for this topic are available online at www.expertconsult.com.
Additional videos for this topic are available online at www.expertconsult.com.
Elbow Anatomy
The elbow is a synovial joint composed of three elbow joint articulations: the trochlea and ulna, the capitellum and the radial head, and the proximal ulna and radius (Fig. 4-1). The elbow joint has prominent joint recesses located in the coronoid and radial fossae anteriorly and within the olecranon fossa posteriorly. Within each joint recess exists an intracapsular but extrasynovial fat pad, which becomes displaced with joint distention. The medial elbow joint is stabilized by the ulnar collateral ligament, of which the anterior band that extends anteriorly to the sublime tubercle of the ulna is the most important. Other components of the ulnar collateral ligament include posterior and oblique bands. Laterally, the elbow joint is stabilized by the radial collateral ligament complex, which is composed of the radial collateral ligament, the annular ligament, and a smaller accessory radial collateral ligament. An additional component, the lateral ulnar collateral ligament, extends from the lateral epicondyle to insert on the crista supinator of the proximal ulna.
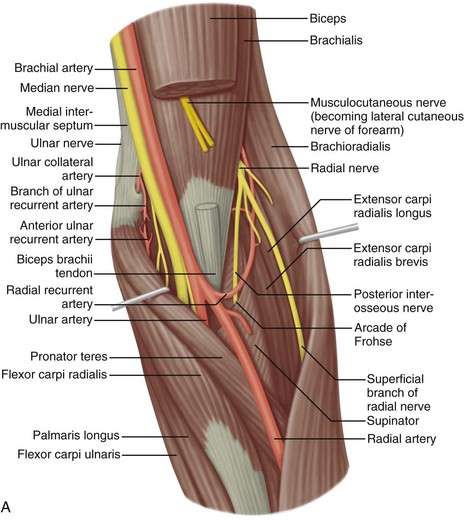
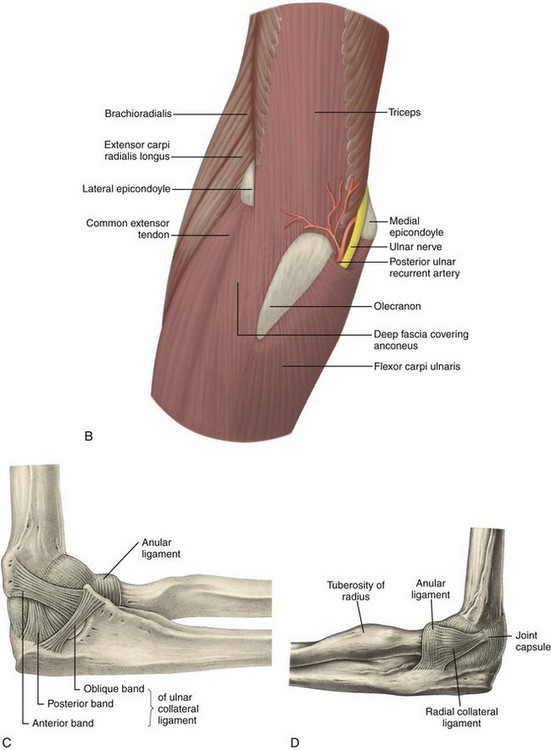
FIGURE 4-1 Elbow anatomy.
(From Standring S: Gray’s anatomy: the anatomical basis of clinical practice, ed 39, Edinburgh, 2005, Churchill Livingstone.)
Anterior to the elbow joint, the brachialis inserts on the ulna, and the biceps brachii tendon inserts on the radial tuberosity. With regard to the biceps brachii, a dual insertion exists where the short head is superficial and inserts more distal relative to the long head on the radial tuberosity.1 Posteriorly, the triceps brachii inserts on the olecranon process of the proximal ulna, over which is located the olecranon bursa. The lateral and long heads of the triceps brachii represent the most superficial layer of the distal triceps, whereas the deep aspect with a relatively shorter tendon is the medial head.2 The anconeus is located between the olecranon process and the lateral epicondyle of the humerus. Medially, the common flexor tendon, consisting of the flexor carpi radialis, palmaris longus, flexor carpi ulnaris, and flexor digitorum superficialis, originates on the medial epicondyle of the distal humerus. Laterally, the common extensor tendon, composed of the extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris, originates at the lateral epicondyle of the distal humerus. The extensor carpi radialis brevis is the most anteriorly located of the group; the extensor carpi radialis longus originates proximal to the lateral epicondyle on the lateral humeral metaphysis.
The space between the olecranon process of the ulna and the medial epicondyle is bridged by the cubital tunnel retinaculum (or Osborne fascia) and contains the ulnar nerve. Just distal to this, the ulnar nerve enters the true cubital tunnel, between the dual origins of the flexor carpi ulnaris and deep to the arcuate ligament.3 The median nerve is located medial to the brachial artery and courses distally between the ulnar and humeral heads of the pronator teres. The radial nerve is located at the posterior aspect of the humeral shaft and then courses distally and laterally beneath the brachioradialis, where a deep branch courses between the two heads of the supinator muscle and a superficial branch courses beneath the brachioradialis and into the forearm.
Ultrasound Examination Technique
Table 4-1 is an elbow ultrasound examination checklist. Examples of diagnostic elbow ultrasound reports are available online at www.expertconsult.com (see eBox 4-1 and 4-2).
| Location | Structures of Interest |
|---|---|
| Anterior |
eBox 4-1 Sample Diagnostic Elbow Ultrasound Report
Normal, Complete
Examination: Ultrasound of the Elbow
History: Elbow pain, evaluate for tendon abnormality
Findings: No evidence of joint effusion or synovial process. The biceps brachii and brachialis are normal. The common flexor and extensor tendons are also normal. No significant triceps brachii abnormality. The anterior band of the ulnar collateral ligament and radial collateral ligament complex are normal. The ulnar nerve, radial nerve, and median nerve at the elbow are unremarkable. No abnormality in the cubital tunnel region with dynamic imaging. Additional focused evaluation at site of maximal symptoms was unrevealing.
Impression: Unremarkable ultrasound examination of the elbow.
eBox 4-2 Sample Diagnostic Elbow Ultrasound Report
Abnormal, Complete
Examination: Ultrasound of the Elbow
History: Elbow pain, evaluate for tendon abnormality
Findings: There is a partial-thickness tear of the distal biceps brachii tendon involving the superficial short head tendon with approximately 2 cm of retraction but with intact long head. Dynamic evaluation shows continuity of the long head excluding full-thickness tear. No joint effusion. The triceps brachii, common extensor, and common flexor tendons are normal. The ulnar, radial, and median nerves are unremarkable, including dynamic evaluation of the ulnar nerve. Unremarkable ulnar and radial collateral ligaments. No bursal distention.
Impression: Partial-thickness tear of the distal biceps brachii tendon.
Anterior Evaluation
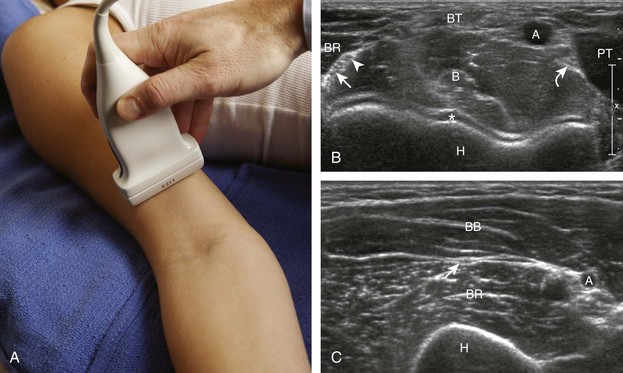
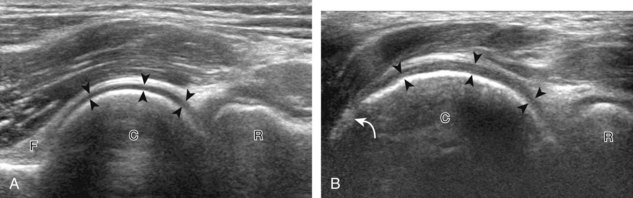
The primary structures evaluated from the anterior approach are the brachialis, the distal biceps brachii, the median nerve, and the anterior elbow joint recess. For sonographic evaluation, the elbow is comfortably extended, and the hand is supinated. Evaluation begins with the transducer short axis to the biceps brachii and brachialis just superior to the elbow joint. For orientation, it is helpful to begin at the medial aspect of the anterior elbow and locate the brachial artery, identified by its pulsation and flow on color Doppler imaging (Fig. 4-2). Deep to the brachial artery and in midline is the brachialis muscle, immediately adjacent to the distal humerus. The hypoechoic layer over the hyperechoic cortex is the hyaline articular cartilage. Normal muscle is predominantly hypoechoic with intervening hyperechoic fibroadipose septations. Just lateral to the brachial artery and superficial to the brachialis is the biceps brachii tendon. Immediately medial to the brachial artery is the median nerve, which has a speckled appearance from hypoechoic nerve fascicles and surrounding hyperechoic connective tissue. Medial to the median nerve is the humeral head of the pronator teres muscle. At the far lateral aspect of the anterior elbow is the brachioradialis muscle. In between the brachialis and brachioradialis is an oblique fascial layer, which contains the superficial and deep branches of the radial nerve. More proximal to the elbow joint, the musculocutaneous nerve can be identified between the biceps brachii and brachialis muscles (see Fig. 4-2C).
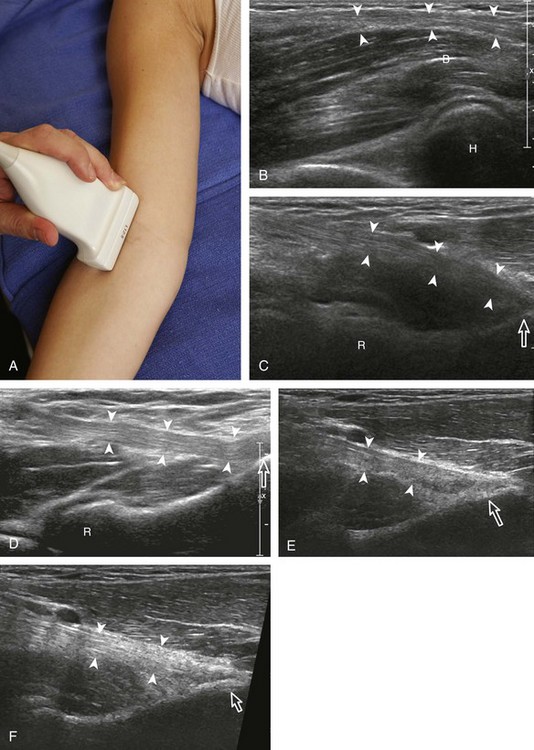
To evaluate the biceps brachii tendon, the transducer is centered over the biceps tendon and rotated 90 degrees (Fig. 4-3). At this location, the biceps tendon will be hyperechoic and fibrillar with a uniform thickness over the brachialis muscle (see Fig. 4-3B). As the biceps brachii tendon courses deep along the outer contour of the brachialis, the tendon will become hypoechoic from anisotropy (see Fig. 4-3C). Using the heel-toe maneuver, the sound beam is angled superiorly in order to image the tendon perpendicular to eliminate anisotropy (see Fig. 4-3D). Some ultrasound machines will have beam steering, which can assist in reducing anisotropy (see Figs. 4-3E and F). If the distal biceps is difficult to visualize, the elbow position may be changed with additional minimal flexion or extension. The biceps brachii is also evaluated in short axis (Fig. 4-4). The lacertus fibrosis or bicipital aponeurosis can be seen extending from the biceps brachii tendon to the pronator teres and flexor musculature, superficial to the brachial artery and median nerve, by placing the transducer over the anterior elbow angled from the biceps brachii tendon distal and medial (see Fig. 4-4C).
If the distal biceps brachii tendon insertion onto the radial tuberosity in long axis is not clearly seen, a more medial approach should be attempted (Fig. 4-5). With the transducer long axis to the biceps brachii tendon in the sagittal plane on the body, the transducer is moved slightly medial with the beam angled slightly lateral toward the center of the elbow. If the brachial vasculature is visualized, then the transducer needs to be angled laterally. This maneuver is continued, only a millimeter at a time, while adding the heel-toe manuever until the distal tendon is visualized. With the transducer over the medial elbow angled toward the lateral elbow, often the distal biceps brachii tendon can be seen through the medial brachial vasculature as an acoustic window.4 Distal tendon attachment can also be assessed during supination and pronation dynamically (Video 4-1)![]() .
.
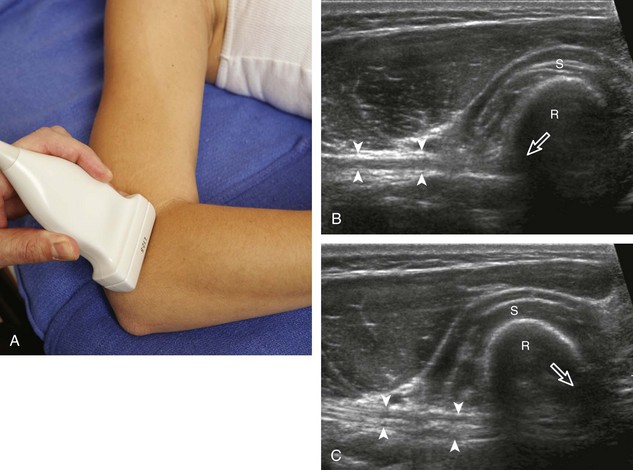
An additional method to evaluate the distal biceps brachii tendon to differentiate a nonretracted full-thickness tear from a partial-thickness tear is from a lateral approach with the elbow flexed.5 Examination with this technique begins with the transducer in short axis relative to the proximal radius (Fig. 4-6). The radial head is visualized as a curvilinear echogenic structure, and the transducer is moved toward the wrist over the radial neck, where the surrounding supinator muscle can be seen. At this level, the hand can be passively supinated and pronated to visualize movement of the biceps brachii tendon, which is perpendicular to the sound beam (Video 4-2)![]() . There is also one additional method to evaluate the most distal aspect of the biceps brachii tendon (Fig. 4-7), in which the transducer is placed transverse to the radius dorsally between the radius and ulna with the hand in pronation to visualize the radial tuberosity insertion.
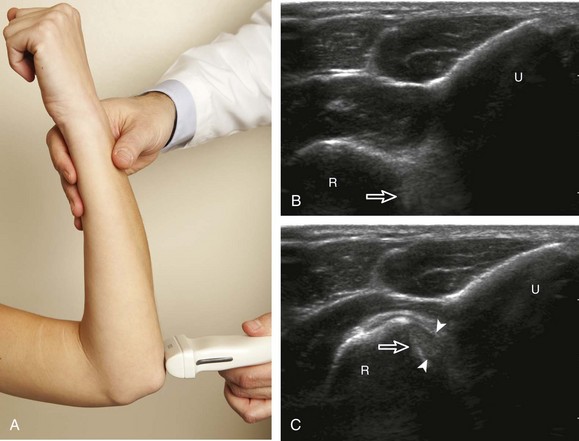
. There is also one additional method to evaluate the most distal aspect of the biceps brachii tendon (Fig. 4-7), in which the transducer is placed transverse to the radius dorsally between the radius and ulna with the hand in pronation to visualize the radial tuberosity insertion.
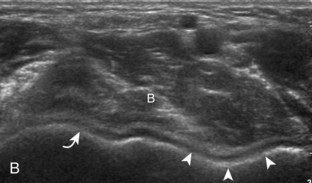
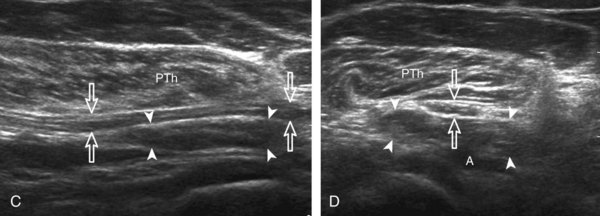
To complete the anterior evaluation of the elbow, the transducer is returned to the sagittal plane directly long axis to the brachialis to visualize the anterior recess of the elbow joint (Fig. 4-8A and B). Here, the coronoid fossa and smaller radial fossa are visible as concavities in the distal humerus. Within these fossae, a triangular hyperechoic intracapsular fat pad is normally seen. The hypoechoic hyaline cartilage of the trochlea and capitellum can also be identified. Returning to the original short axis view of the brachial artery, the normal median nerve is again identified in short axis and can be followed distally as it courses between the humeral and ulnar heads of the pronator teres, a potential site of nerve entrapment (see Fig. 4-8C and D). The ulnar head of the pronator teres is located between the median nerve and the ulnar artery.
Medial Evaluation
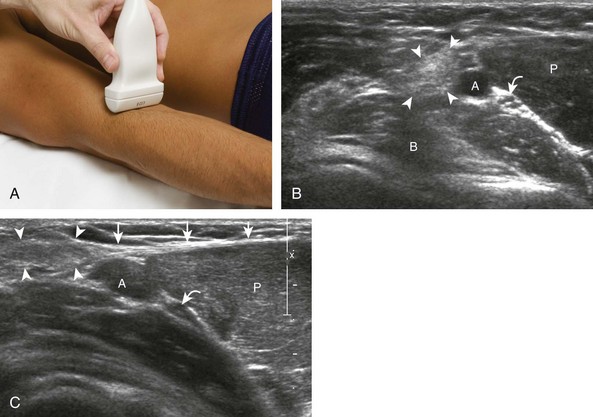
For medial evaluation, the elbow is slightly flexed to bring the anterior band of the ulnar collateral ligament into the coronal plane. Sonographic evaluation of the medial elbow structures begins by visually identifying or palpating the medial epicondyle of the humerus. The transducer is then placed in long axis to the forearm with the proximal aspect over the medial epicondyle (Fig. 4-9). The characteristic hyperechoic bony contours of the medial epicondyle should be seen. Distal to the medial epicondyle, the humerus has a flattened surface where the humerus articulates with the proximal ulna. In this imaging plane long axis to the forearm, as indicated by the characteristic bone contours, both the common flexor tendon and the anterior band of the ulnar collateral ligament can be identified (see Fig. 4-9B). The origin of the common flexor tendon should be seen at the superficial aspect of the medial epicondyle as hyperechoic and fibrillar, with transition to hypoechoic musculature more distally. In addition, the anterior band of the ulnar collateral ligament is seen attached to the medial epicondyle as hyperechoic and fibrillar, but somewhat more compact than that of tendon. If not perpendicular to the ligament, the anterior band of the ulnar collateral ligament will be hypoechoic from anisotropy, but still fairly uniform in thickness where it extends distally over the joint space to insert on the proximal ulna.6 The anterior band of the ulnar collateral ligament has a somewhat variable appearance at its proximal attachment to the humerus; it may appear as a uniform band, or it may fan out more proximally, interspersed with hyperechoic fatty tissue.7 The normal joint recess of the elbow extends proximally between the anterior band of the ulnar collateral ligament and adjacent humerus, but it should not extend medially from this point at the humeral attachment of the ligament or distal over the ulna. The long axis view is the key plane in the imaging of both the common flexor tendon and anterior band of the ulnar collateral ligament, although if a pathologic process is identified, further characterization is completed by imaging in short axis to these structures. In addition, the ulnar collateral ligament and medial joint space can be evaluated with dynamic valgus stress with the elbow in slight flexion to assess for ligamentous injury.8,9
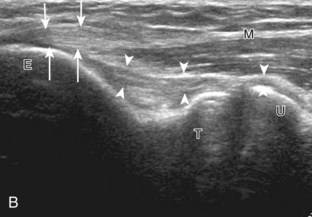
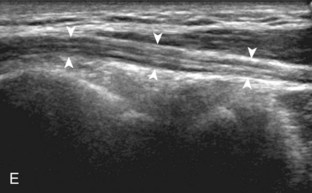
After evaluation of the common flexor tendon and anterior band of the ulnar collateral ligament is completed, attention is turned to the cubital tunnel region more posteriorly. To evaluate the cubital tunnel region, the elbow is turned outward so that the bony protuberances of the olecranon process and the medial epicondyle can be visualized and are palpable. Evaluation should begin with the elbow extended; if the elbow is flexed at this point, it is possible that the ulnar nerve may dislocate and be difficult to locate, and identification of an anconeus epitrochlearis becomes difficult as well (see discussion later). The ultrasound transducer is placed in the transverse plane between the olecranon process and the medial epicondyle, and the characteristic hyperechoic and shadowing bone contours of these structures are seen (Fig. 4-10A and B). The ulnar nerve is visible as speckled or honeycomb in appearance from hypoechoic nerve fascicles and hyperechoic connective tissue. However, the ulnar nerve posterior to the medial epicondyle often appears hypoechoic surrounded by hyperechoic fat and may be bilobed or bifid. Superficial to the ulnar nerve, the cubital tunnel retinaculum (or Osborne fascia) is located and, when present, appears as a thin structure between the olecranon and medial epicondyle. Distally, the ulnar nerve can be followed into the true cubital tunnel between the humeral and ulnar heads of the flexor carpi ulnaris and under the arcuate ligament (see Fig. 4-10C). With rotation of the transducer 90 degrees, the ulnar nerve can be evaluated in long axis (see Fig. 4-10D and E).
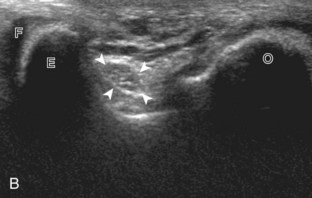
It is also important to evaluate the cubital tunnel region dynamically for pathology.10 With the transducer again placed in the transverse plane between the medial epicondyle and olecranon process and fixed over the medial epicondyle, the patient is asked to actively flex the elbow (Fig. 4-11). During this maneuver, the olecranon process moves out of the imaging plane and is replaced by the hypoechoic triceps brachii muscle. It is often helpful to first perform this maneuver passively so that if the bone contour of the medial epicondyle apex is no longer visualized, the movement can be stopped and the transducer repositioned until the epicondyle is found again and the motion continued. Normally during elbow flexion, the ulnar nerve moves toward the apex of the medial epicondyle but should not translate over the epicondyle anteriorly. Abnormal ulnar nerve translation over the medial epicondyle may be felt as a palpable snap through the transducer, and typically it returns back into normal position as the elbow is extended. It is important not to place too much pressure with the transducer during this dynamic evaluation because this may inhibit the abnormal ulnar nerve translation; intermittent reduction in transducer pressure during the maneuver avoids this pitfall. Ulnar nerve dislocation has been described in up to 20% of asymptomatic individuals, so it is important to correlate with abnormal ulnar nerve morphology and symptoms.11 It is also essential to differentiate isolated ulnar nerve dislocation from snapping triceps syndrome. In this situation, both the medial head of the triceps muscle and the ulnar nerve dislocate over the medial epicondyle of the humerus in elbow flexion.7
Lateral Evaluation
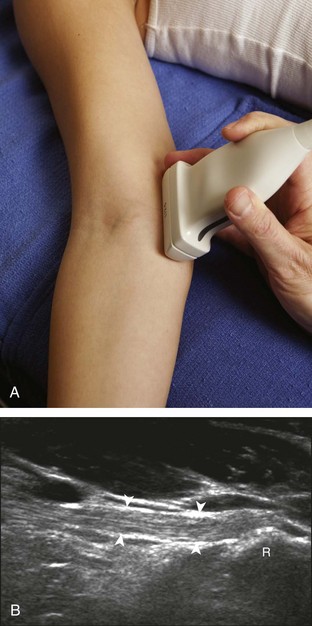
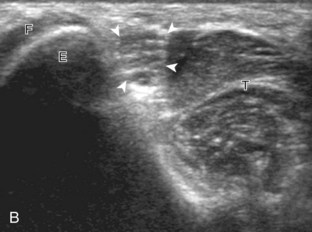
For evaluation of the lateral elbow structures, the arm is rotated inward and slightly flexed. Structures of interest laterally include the common extensor tendon, the radial collateral ligament complex, the radial head and annular recess, and the capitellum. Unlike the medial aspect of the elbow, the lateral epicondyle is not clearly visible to the eye and is more difficult to palpate. Therefore, bone landmarks as seen at sonography are used for orientation. To begin, the transducer is placed in long axis relative to the forearm over the lateral elbow (Fig. 4-12A), and the characteristic hyperechoic shadowing contour of the radial head is readily identified (see Fig. 4-12B). More proximal scanning in this plane reveals the radius articulation with the capitellum, and more proximally, the relatively flattened contour of the lateral epicondyle (see Fig. 4-12C). At this site, the hyperechoic and fibrillar common extensor tendon can be seen originating on the lateral epicondyle. Although the long axis view is optimum in identification of the common extensor tendon, any abnormality should also be characterized in short axis as well. Care should be taken to include evaluation of the most anterior aspect of the common extensor tendon, where tendon abnormalities most commonly occur. Deep to the common extensor tendon in the long axis plane over the lateral epicondyle is the radial collateral ligament (see Fig. 4-12C).12 It is often difficult to discern the separation between the proximal common extensor tendon and the adjacent radial collateral ligament; however, if one follows these structures distally, the deeper radial collateral ligament will attach to the annular ligament, seen immediately over the radial head, whereas the more superficial common extensor tendon will continue more superficial and become muscle. If the transducer is placed over the lateral elbow and angled posteriorly from the distal humerus to the ulna, the hyperechoic and fibrillar lateral ulnar collateral ligament can be seen (see Fig. 4-12D).12,13 At the level of the radial neck, the collapsed annular recess is difficult to discern unless it is abnormally distended (see Fig. 4-20B).
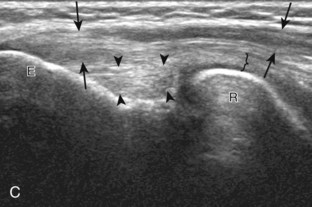
With elbow extension and the transducer anterolateral in the sagittal plane, the thin uniform hypoechoic layer of hyaline cartilage can be seen over the anterior aspect of the capitellum (Fig. 4-13A). At the radiocapitellar joint, a hyperechoic, triangular, meniscus-like synovial reflection or fold, also termed the posterolateral plica, extends from the radial collateral ligament and joint capsule into the joint.14,15 With movement of the transducer posteriorly over the capitellum, the irregular cortex represents a normal appearance void of cartilage and should not be misinterpreted as an osteochondral abnormality.14 With the elbow in flexion and the transducer posterior in the sagittal plane, the central and posterior aspect of the capitellum hyaline cartilage can also be visualized (Fig. 4-13B).
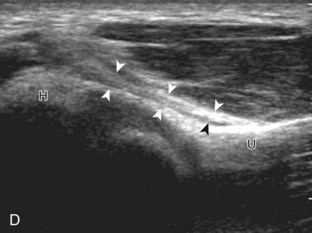
For evaluation of the radial nerve, one approach is to first find the oblique fascial plane between the brachioradialis and the brachialis anteriorly in the transverse plane, where the deep and superficial branches of the radial nerve are seen as round and hypoechoic (Fig. 4-14A; see Fig. 4-2B). These individual branches can be followed proximally in short axis where they join to form the radial nerve (see Fig. 4-14B and C). Evaluation can continue more proximal to follow the radial nerve as it traverses the intermuscular fascia and follows the posterior cortex of the humerus. The transducer is turned 90 degrees to evaluate the radial nerve and its branches in long axis as well. Following the radial nerve branches distally, the deep branch is seen entering into the supinator muscle as the posterior interosseous nerve (see Fig. 4-14D). The deep branch of the radial nerve often changes shape as it passes beneath the arcade of Frohse and should not be interpreted as nerve swelling.16