5
Cornea
Trauma
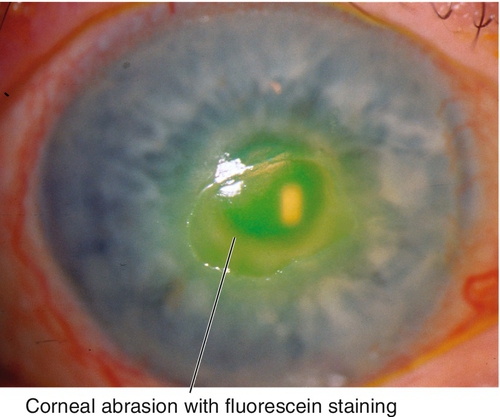
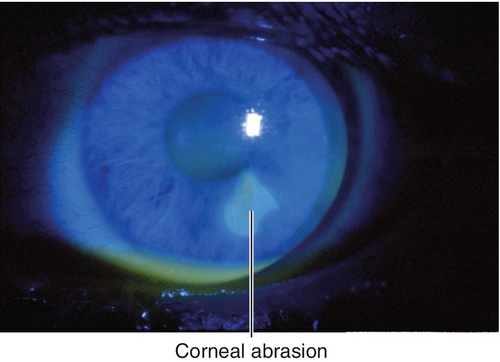
Abrasion
Corneal epithelial defect usually due to trauma. Patients note pain, foreign body sensation, photophobia, tearing, and red eye. May have normal or decreased visual acuity, conjunctival injection, and an epithelial defect that stains with fluorescein.
• Consider topical nonsteroidal anti-inflammatory drugs (NSAIDs) (ketorolac tromethamine [Acular], nepafenac [Nevanac, Ilevro], bromfenac [Bromday, Prolensa], or diclofenac sodium [Voltaren] tid for 48–72 hours) for pain.
• Consider topical cycloplegic (cyclopentolate 1% bid) for pain and photophobia.
• Pressure patch or bandage contact lens if area larger than 10 mm2. (Note: DO NOT patch if patient is contact lens wearer, there is corneal infiltrate, or injury caused by plant material, as these scenarios represent high risk for infectious keratitis if patched; no patching necessary if area of abrasion is < 10 mm2.)
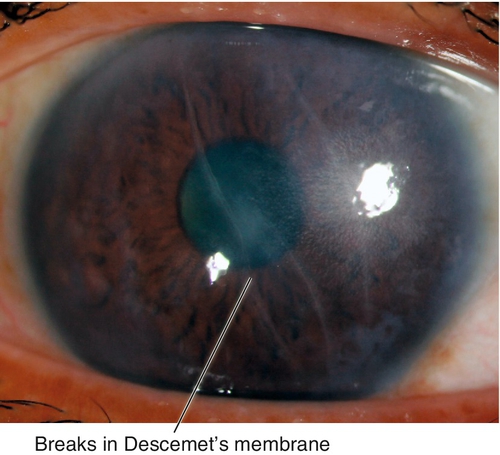
Birth Trauma
Vertical or oblique breaks in Descemet’s membrane due to forceps injury at birth. Results in acute corneal edema, scars in Descemet’s membrane; associated with astigmatism and amblyopia; may develop corneal decompensation and bullous keratopathy later in life.
• Consider Descemet’s stripping automated endothelial keratoplasty (DSAEK), Descemet’s membrane endothelial keratoplasty (DMEK), or penetrating keratoplasty for corneal decompensation.
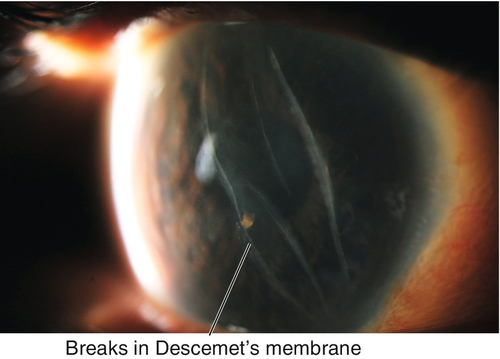
Figure 5-4 Same patient as Figure 5-3 demonstrating the corneal scars as seen with sclerotic scatter of the slit-beam light.
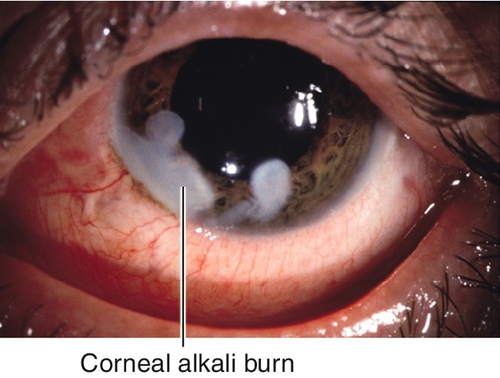
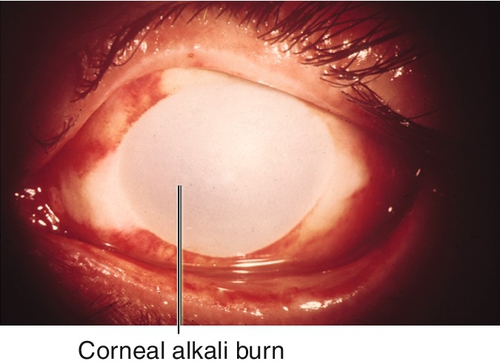
Burn
Corneal tissue destruction (epithelium and stroma) due to chemical (acid or base) or thermal (e.g., welding, intense sunlight, tanning lamp) injury; alkali causes most severe injury (penetrates and disrupts lipid membranes) and may cause perforation. Patients note pain, foreign body sensation, photophobia, tearing, and red eye. May have normal or decreased visual acuity, conjunctival injection, ciliary injection, epithelial defects that stain with fluorescein, and scleral or limbal blanching due to ischemia in severe chemical burns. Prognosis variable, worst for severe alkali burns.
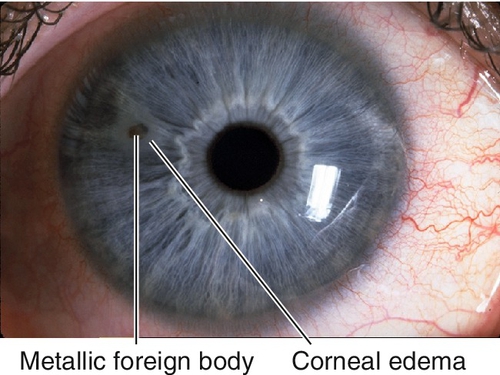
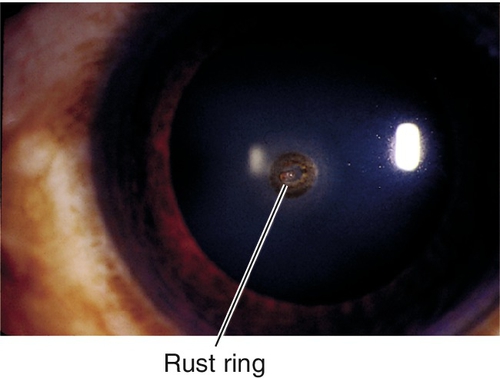
Foreign Body
Foreign material on or in cornea; usually metal, glass, or organic material; may have associated rust ring if metallic. Patients note pain, foreign body sensation, photophobia, tearing, and red eye; may be asymptomatic if deep and chronic. May have normal or decreased visual acuity, conjunctival injection, ciliary injection, foreign body, rust ring, epithelial defect that stains with fluorescein, corneal edema, anterior chamber cells and flare. Usually good prognosis unless rust ring or scarring involves visual axis.
• Remove rust ring with Alger brush or automated burr.
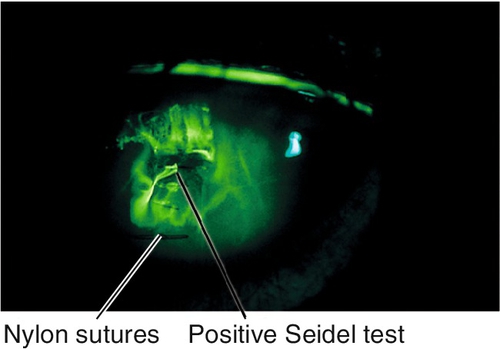
• Seidel test if deep foreign body to rule out open globe (see below).
• Topical antibiotic (polymyxin B sulfate-trimethoprim [Polytrim], moxifloxacin [Vigamox]/gatifloxacin [Zymaxid], or tobramycin [Tobrex] tid–qid).
• Consider topical cycloplegic (cyclopentolate 1% bid) for pain.
• Pressure patch or bandage contact lens as needed (same indications as for corneal abrasion; see above).
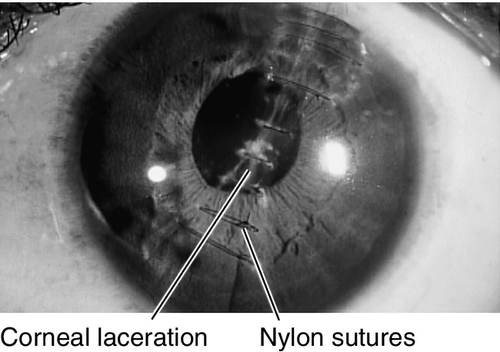
Laceration
Partial- or full-thickness cut in cornea (see Open Globe section in Chapter 4) due to trauma. Patients note pain, foreign body sensation, photophobia, tearing, and red eye. May have normal or decreased visual acuity, conjunctival injection, ciliary injection, intraocular foreign body, positive Seidel test, corneal edema, breaks or scars in Descemet’s membrane, anterior chamber cells and flare, low intraocular pressure. Potentially good prognosis unless laceration crosses the visual axis.
• Partial-thickness lacerations require topical broad-spectrum antibiotic (gatifloxacin [Zymaxid] or moxifloxacin [Vigamox] tid–qid) and cycloplegic (cyclopentolate 1% or scopolamine 0.25% tid).
• Daily follow-up until wound has healed.
• Pressure patch or bandage contact lens as needed for self-sealing or small wounds; if wound gape exists, consider surgical repair.
• Full-thickness lacerations usually require surgical repair (see Open Globe section in Chapter 4).
• Consider orbital radiographs or computed tomography (CT) scan to rule out intraocular foreign body when full-thickness laceration exists; magnetic resonance imaging (MRI) is contraindicated if foreign body is metallic.
Recurrent Erosion
Recurrent bouts of pain, foreign body sensation, photophobia, tearing, red eye, and spontaneous corneal epithelial defect usually upon awakening. Associated with anterior basement membrane dystrophy in 50% of cases, or previous traumatic corneal abrasion (usually from superficial shearing injury such as from a fingernail, paper, plant, or brush); also occurs in Meesman’s, Reis–Bücklers, lattice, granular, Fuchs’, and posterior polymorphous dystrophies, and rarely after surgery (cataract or corneal refractive).
• Topical lubrication with preservative-free artificial tears up to q1h or Muro 128 drops.
• Consider debridement (manual or with 20% alcohol for 30–40 seconds), diamond burr polishing, bandage contact lens, anterior stromal puncture /reinforcement, Nd : YAG laser reinforcement, superficial keratectomy, or phototherapeutic keratectomy (PTK) for multiple recurrences.
• Consider doxycycline 50 mg po bid for 2 months (matrix metalloproteinase-9 inhibitor) and topical steroid tid for 2–3 weeks.
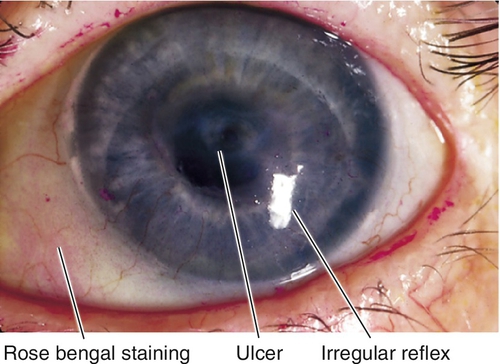
Peripheral Ulcerative Keratitis
Definition
Progressive stromal ulceration and thinning of the peripheral cornea with an overlying epithelial defect associated with inflammation.
Etiology
Due to noninfectious systemic or local diseases as well as systemic or local infections.
Marginal Keratolysis
Acute peripheral ulcerative keratitis (PUK) due to an autoimmune or collagen vascular disease (rheumatoid arthritis [most common], systemic lupus erythematosus, polyarteritis nodosa, relapsing polychondritis, and Wegener’s granulomatosis).
Mooren’s Ulcer
Idiopathic. Two types:
Type I
More common (75%), benign, and unilateral; occurs in older patients; responds to conservative management.
Type II
Progressive and bilateral; occurs in younger patients; more common in African-American males; may be associated with coexistent parasitemia.
Staphylococcal Marginal Keratitis
Immune response (hypersensitivity) to Staphylococcus aureus; associated with staphylococcal blepharitis, rosacea, phlyctenule, and vascularization.
Symptoms
Pain, tearing, photophobia, red eye, and decreased vision; may be asymptomatic.
Signs
Normal or decreased visual acuity, conjunctival injection, ciliary injection, corneal thinning, corneal edema, anterior chamber cells and flare, hypopyon; may have corneal infiltrate; may perforate.
Marginal Keratolysis
Acute ulceration with rapid progression, usually in one sector; corneal epithelium absent; melting resolves after healing of overlying epithelium; may have associated scleritis.
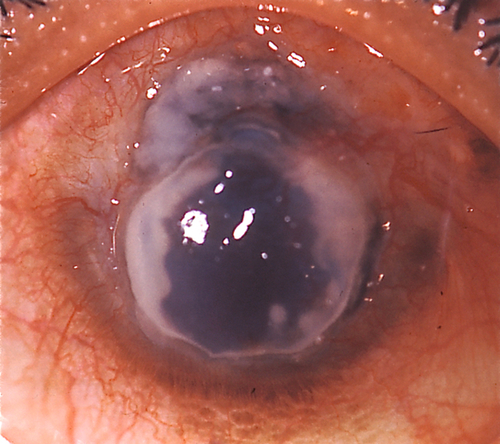
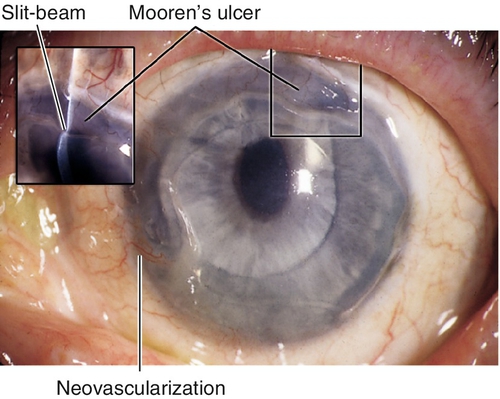
Mooren’s Ulcer
Thinning and ulceration that spreads circumferentially and then centrally with undermining of the leading edge; may develop neovascularization.
Staphylococcal Marginal Keratitis
Ulceration and white infiltrate(s) 1–2 mm from the limbus with an intervening clear zone; often stains with fluorescein; may progress to a ring ulcer or become superinfected.
Differential Diagnosis
Infectious ulcer, sterile ulcer (diagnosis of exclusion), Terrien’s marginal degeneration, pellucid marginal degeneration, senile furrow degeneration.
Evaluation
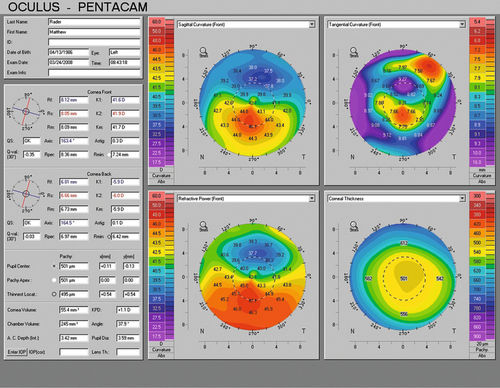
• Consider corneal topography (computerized videokeratography).
• Lab tests: Complete blood count (CBC), erythrocyte sedimentation rate (ESR), rheumatoid factor (RF), antinuclear antibody (ANA), antineutrophil cytoplasmic antibody (ANCA), anti-cyclic citrullinated peptide (anti-CCP), blood urea nitrogen (BUN), creatinine, urinalysis (UA); consider hepatitis C antigen (Mooren’s ulcer).
• Consider cultures or smears to rule out infectious etiology.
• Medical or rheumatology consultation for systemic disorders or when treatment with immunosuppressive medications is anticipated.
Prognosis
Depends on etiology; poor for marginal keratolysis and Mooren’s ulcer.
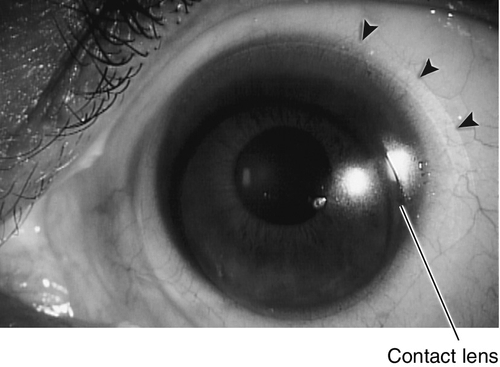
Contact-Lens-Related Problems
Definition
A variety of abnormalities induced by contact lenses. Several types of lenses exist, broadly divided into rigid and soft lenses. They are used primarily to correct refractive errors (myopia, hyperopia, astigmatism, and presbyopia), but also can serve as a therapeutic device (bandage lens) for unhealthy corneal surfaces or even for cosmetic use (to apparently change iris color or create a pseudopupil).
Rigid Lenses
Hard
Polymethylmethacrylate (PMMA) lenses impermeable to oxygen; blinking allows tear film to enter the space beneath the lens providing nutrition to the cornea. Used for daily wear with good visual results but can lead to corneal edema and visual blur due to corneal hypoxia. Rarely used today.
Gas-permeable
Rigid lenses composed of cellulose acetate butyrate, silicone acrylate, or silicone combined with polymethylmethacrylate; high oxygen permeability allows for greater comfort and improved corneal nutrition. Used for daily wear; lens of choice for patients with keratoconus and high astigmatism. Hardest contact lens to adjust to but lowest rate of contact-lens-related keratitis. Also available as specialized and hybrid lenses (i.e., SynergEyes, Boston ocular surface prosthesis [PROSE lens]).
Soft Lenses
Daily wear
Hydrogel lenses (hydroxymethyl methacrylate); more comfortable and flexible than rigid lenses; conform to corneal surface, therefore poorly correct large degrees of astigmatism; length of time of wear depends on oxygen permeability and water content. Toric versions available up to 3 diopters.
Extended wear
Disposable lenses discarded after extended wear from 1 week to 30 days; higher risk (10–15 ×) of infectious keratitis with overnight wear (occurs in approximately 1 : 500).
Symptoms
Foreign body sensation, decreased vision, red eye, tearing, itching, burning, pain, lens awareness, and reduced contact lens wear time.
Signs and management
Corneal Abrasion
Corneal fluorescein staining due to epithelial defect; contact-lens-related etiologies include foreign bodies under lens, damaged lens, poor lens fit, corneal hypoxia, poor lens insertion or removal technique (see Trauma: Corneal Abrasion section above).
• Treat as for traumatic corneal abrasion except do not patch any size abrasion.
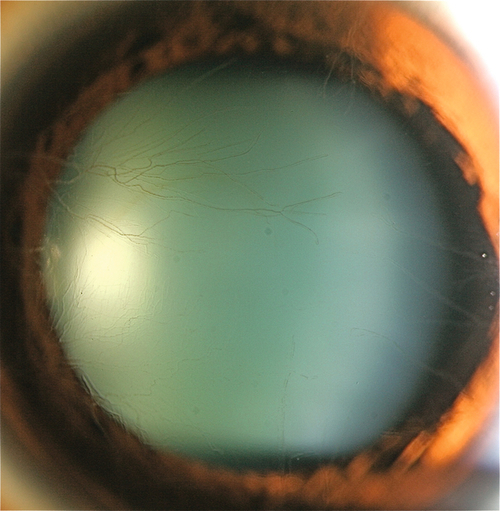
Corneal Hypoxia
Acute
Conjunctival injection and epithelial defect (PMMA contact lens).
• Topical antibiotic ointment (polymyxin B sulfate-bacitracin [Polysporin] tid for 3 days).
• When acute hypoxia has resolved, refit with higher Dk / L (oxygen transmissibility) contact lens.
Chronic
Punctate staining, corneal epithelial microcysts, stromal edema, and corneal neovascularization.
• Suspend contact lens use or decrease contact lens wear time.
• Refit with higher Dk / L contact lens.
Contact-Lens-Related Dendritic Keratitis
Conjunctivitis, pseudodendritic lesions.
Contact Lens Solution Hypersensitivity or Toxicity
Conjunctival injection, diffuse corneal punctate staining or erosion; occurs with solutions that contain preservatives (e.g., thimerosal).
• Identify and discontinue toxic source; thoroughly clean, rinse, and disinfect contact lenses; reinstruct patient in proper contact lens care or change system of care; replace soft contact lenses or polish rigid contact lens.
• Topical antibiotic ointment (erythromycin or bacitracin tid for 3 days); do not patch.
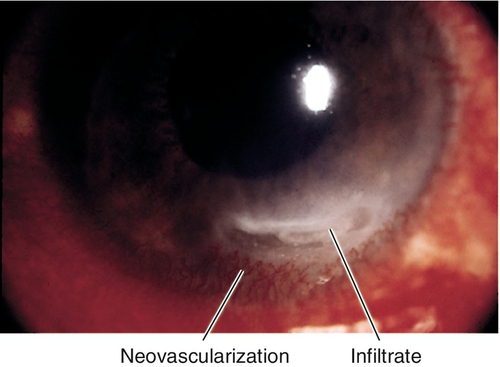
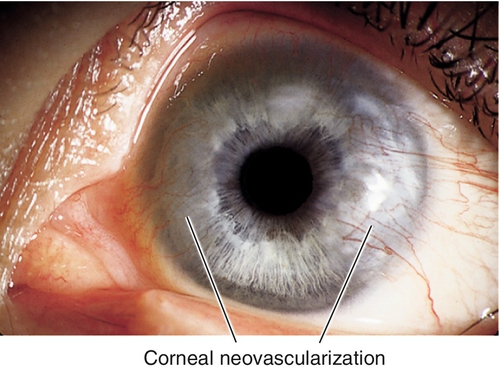
Corneal Neovascularization
Superficial or deep vascular ingrowth due to chronic hypoxia. Superior corneal pannus 1–2 mm in soft contact lens wearers is common and benign; larger than 2 mm is serious; deep vessels may cause stromal hemorrhage, lipid deposits, and scarring.
• Consider topical steroid (prednisolone acetate 1% qid) to cause regression.
• Consider argon laser photocoagulation of large or deep vessels to prevent stromal hemorrhage or rebleed.
• Consider bevacizumab (Avastin) subconjunctival injections adjacent to the neovascularization (2.5 mg /0.1 mL q month for up to 5 months).
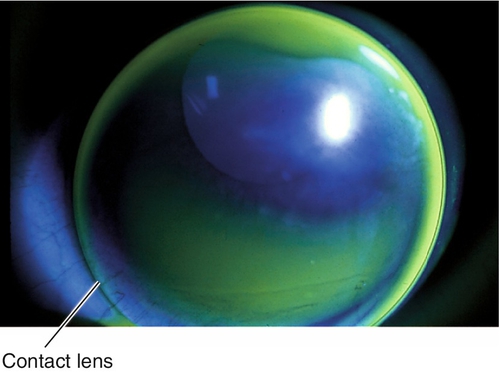
Corneal Warpage
Change in corneal shape (regular and irregular astigmatism) not associated with corneal edema; related to lens material (hard > rigid gas-permeable contact lens [RGP] > soft), fit, and length of time of wear. Usually asymptomatic, but some patients may notice poorer vision with glasses or contact lens intolerance; may have loss of best spectacle-corrected visual acuity or change in refraction (especially axis of astigmatism); hallmark is abnormal corneal topography (computerized videokeratography), which shows irregular astigmatism and may mimic keratoconus (pseudokeratoconus), may affect IOL calculations.
• Periodic evaluations with refraction and corneal topography until stabilization occurs.
Damaged Contact Lens
Pain with lens insertion and prompt relief with removal; look for chips in rigid lenses and fissures or tears in soft lenses.
• Replace defective contact lens.
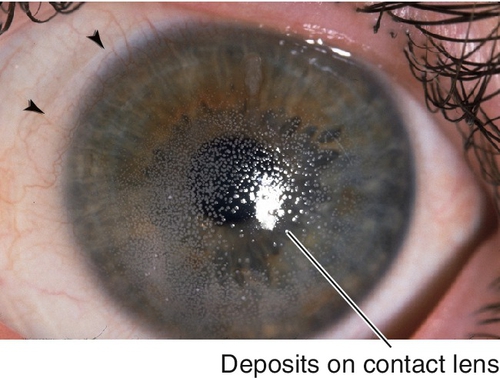
Deposits on Contact Lens
Significant contact lens deposits (film or bumps), conjunctival injection, corneal erosion, excess contact lens movement, giant papillary conjunctivitis; old contact lens.
Giant Papillary Conjunctivitis
Due to contact lens protein deposits, conjunctival contact-lens-related mechanical irritation, or soft contact lens material sensitivity reaction. Signs include large upper lid tarsal conjunctival papillae (> 0.33 mm), ropy mucous discharge, contact lens coating, and possible contact lens decentration secondary to papillae; also caused by exposed suture or ocular prosthesis (see Giant Papillary Conjunctivitis section in Chapter 4).
• Severe: Suspend contact lens use; short course (few weeks) of topical steroid (prednisolone acetate 1% or fluorometholone qid).
Infectious Keratitis
Pain, red eye, infiltrate with epithelial defect, and anterior chamber cells and flare. All contact lens-related corneal infiltrates should be treated as an infection, suspect Pseudomonas or Acanthamoeba. Occurs more often in extended wear and soft contact lens wearers (see Infectious Keratitis section below); fungal infections are more common in warmer climates.
• Lab tests: Cultures of cornea, contact lenses, solutions, and contact lens cases.
• Topical broad-spectrum antibiotic (fluoroquinolone [Vigamox, Zymaxid, or Besivance] or a fortified antibiotic q1h); be alert for Pseudomonas and Acanthamoeba.
• NEVER patch an infiltrate or epithelial defect in a contact lens wearer.
Sterile Corneal Infiltrates
Small (1 mm), peripheral, often multifocal, white, nummular, corneal lesions; corneal epithelium usually intact; diagnosis of exclusion.
• Use preservative-free solutions.
• Must treat as an infection (see above).
Poor Fit (Loose)
Upper eyelid irritation, limbal injection, excess contact lens movement with blinking, poor contact lens centration, lens edge bubbles, lens edge stand-off, variable keratometry mires with blinking, and lower portion of retinoscopy reflex darker and faster.
• Increase sagittal vault; choose steeper base curve or larger-diameter contact lens.
Poor Fit (Light)
Injection or indentation around limbus, minimal contact lens movement with blinking, blurred retinoscopic reflex, corneal edema, and distorted keratometry mires that clear with blinking.
• Decrease sagittal vault; choose flatter base curve or smaller-diameter contact lens.
Superior Limbic Keratoconjunctivitis
Due to contact lens hypersensitivity reaction or poor contact lens fit. Signs include upper tarsal micropapillae, superior limbal injection, fluorescein staining of superior bulbar conjunctiva, and 12 o’clock micropannus (see Superior Limbic Keratoconjunctivitis section in Chapter 4).
• For persistent cases, consider topical steroid (prednisolone acetate 1% or fluorometholone qid) or silver nitrate 0.5–1.0% solution.
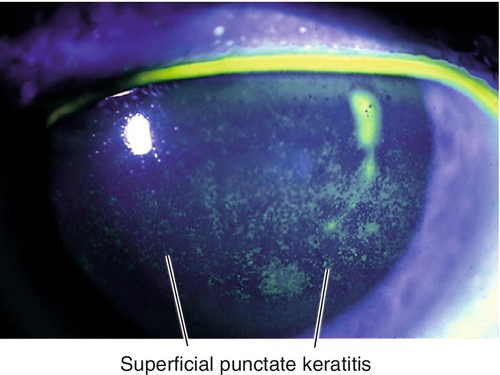
Superficial Punctate Keratitis
Punctate fluorescein staining of corneal surface due to poor lens fit, dry eye, or contact lens solution reaction (see Superficial Punctate Keratitis section below).
• Topical lubrication with artificial tears up to q1h.
• Consider topical broad-spectrum antibiotic (polymyxin B sulfate-trimethoprim [Polytrim], moxifloxacin [Vigamox], or tobramycin [Tobrex] qid) if severe.
• Refit contact lens.
• Consider punctal plugs for dry eyes.
Evaluation
• Complete ophthalmic history with attention to contact lens wear and care habits.
• Complete eye exam with attention to contact lens fit, contact lens surface, everting upper lids, conjunctiva, keratometry, and cornea.
• Consider corneal topography (computerized videokeratography).
• Consider dry eye evaluation: tear meniscus, tear break-up time, lissamine green or rose bengal staining, and Schirmer’s testing (see Chapter 4).
• Lab tests: Cultures or smears of cornea, contact lens, contact lens case, and contact lens solutions if infiltrate exists to rule out infection.
Prognosis
Usually good except for severe or central corneal infections.
Miscellaneous
Definitions
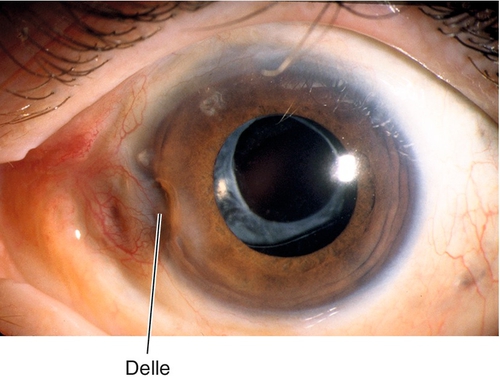
Dellen
Areas of corneal thinning secondary to corneal drying from adjacent areas of tissue elevation. Appear as focal excavations with overlying pooling of fluorescein dye; usually occur near pterygium or filtering bleb.
Exposure Keratopathy
Drying of the cornea with subsequent epithelial breakdown; due to neurotrophic (cranial nerve V palsy, cerebrovascular accident, aneurysm, multiple sclerosis, tumor, herpes simplex, herpes zoster), neuroparalytic (cranial nerve VII palsy [Bell’s palsy]), lid malposition, nocturnal lagophthalmos, or any cause of proptosis with lagophthalmos; sequelae include filamentary keratitis, corneal ulceration and scarring.
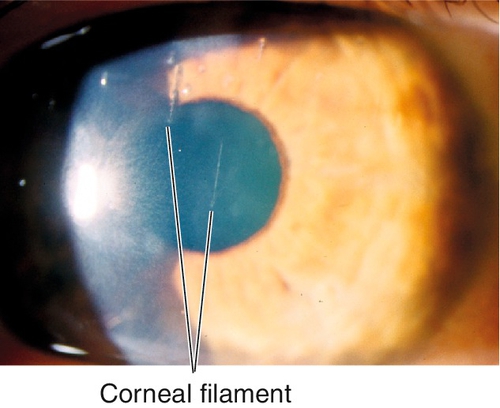
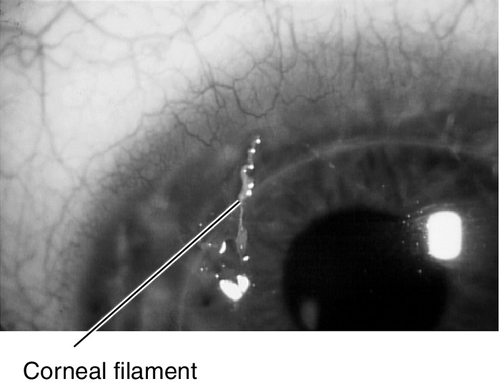
Filamentary Keratitis
Strands of mucus and desquamated epithelial cells adherent to corneal epithelium due to many conditions including any cause of dry eye, patching, recurrent erosion, bullous keratopathy, superior limbic keratoconjunctivitis, herpes simplex, medicamentosa, or ptosis; blinking causes pain as filaments pull on intact epithelium.
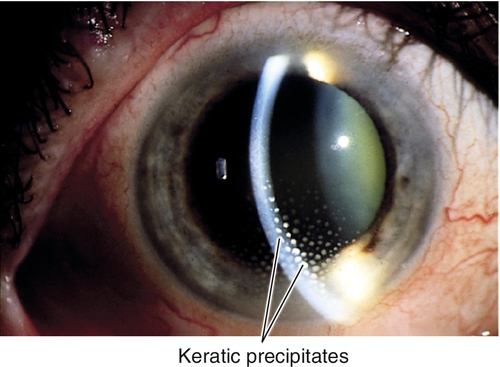
Keratic Precipitates
Fine, medium, or large deposits of inflammatory cells on the corneal endothelium due to a prior episode of inflammation. Usually round white spots, but can be translucent or pigmented; may have mutton fat (in granulomatous uveitis) or stellate (in Fuchs’ heterochromic iridocyclitis) appearance; often melt or disappear or become pigmented with time.
Superficial Punctate Keratitis
Nonspecific, pinpoint, epithelial defects; punctate staining with fluorescein. Associated with blepharitis, any cause of dry eye, trauma, foreign body, trichiasis, ultraviolet or chemical burn, medicamentosa, contact-lens-related, exposure, and conjunctivitis.
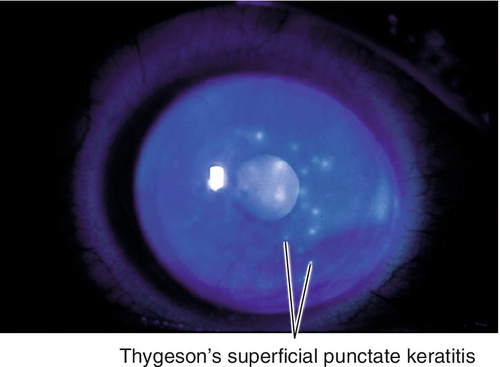
Thygeson’s Superficial Punctate Keratitis
Bilateral, recurrent, gray-white, slightly elevated epithelial lesions (similar to early subepithelial infiltrates in adenoviral keratoconjunctivitis) in a white and quiet eye; minimal or no staining with fluorescein. Unknown etiology, possibly viral; usually occurs in second to third decades.
Symptoms
Asymptomatic; may have dryness, foreign body sensation, discharge, tearing, photophobia, red eye, and decreased vision.
Signs
Normal or decreased visual acuity; may have lagophthalmos, conjunctival injection, decreased corneal sensation, corneal staining, superficial punctate keratitis (inferiorly or in a central band in exposure keratopathy), filaments (stain with fluorescein), subepithelial infiltrates, keratic precipitates, anterior chamber cells, and flare.
Differential Diagnosis
See above.