Chapter 13 Circadian Rhythm of Restless Legs Syndrome
Circadian Variation in Restless Legs Syndrome
One of the defining features of the restless legs syndrome (RLS) is that it shows a notable circadian rhythm with symptoms intensifying later in the day (see Chapter 15). This holds true at least for those who have normal sleep-wake schedules. Those who do shift work, have irregular sleep-wake schedules, or those adjusting to jet lag may not show this pattern. This circadian pattern was noted by Willis in his presumptive case1 and established as a diagnostic feature by Ekbom.2
However, it was not initially clear that this circadian pattern was due to a specific circadian factor rather than merely reflecting the fact that, later in the day, individuals typically reduce activity and begin to relax. This changed state could itself be the cause of the circadian pattern. In two studies, Trenkwalder, Hening, and colleagues3,4 showed that there was a true circadian factor to RLS (Fig. 13-1). These investigators used a semiconstant routine study in which hospitalized patients were observed approximately every 3 hours during which they attempted to stay motionless while seated in bed for 1 hour or longer (a modified suggested immobilization test [mSIT]).5–7 Both subjective (intensity of symptoms) and objective (periodic limb movements [PLM] or motor restlessness) features were measured during 2 days of normal sleep-wake cycles followed by 36 hours of sustained wakefulness. During all days as clock time increased from morning (9:00 A.M.) to early morning the following day (2:00 A.M.), both subjective and objective measures of RLS increased. During continued sleep deprivation, the patients’ discomforts and measures of PLM and motor activity decreased during the day (9:00 A.M. to 3:00 p.m.), before beginning to increase again (6:00 P.M.). Based on these findings, it was concluded that the symptoms and associated motor findings of RLS follow a quite similar circadian pattern with maximum symptoms occurring during the early part of the night.
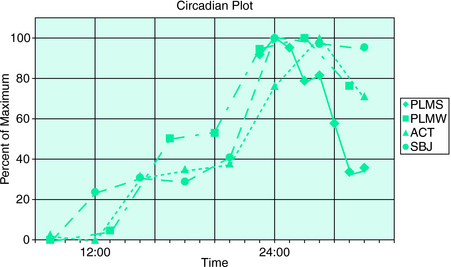
FIGURE 13-1. Circadian plot. Normalized values of the RLS measures are plotted against clock time from 8:00 A.M. through midnight (24:00) to 8:00 A.M. ACT, activity counts (measure of recorded motor activity); PLMS, periodic limb movements in sleep; PLMW, periodic limb movements when awake; SBJ, subjective leg discomfort measured with visual analog scale. Values were derived from modified suggested immobilization tests when subjects were awake (PLMW, ACT, SBJ) and from sleep recordings during sleep (PLMS). Hours represent beginning of an SIT period or beginning of an hour of enumerating PLMS. Data were obtained from two studies carried out over 72 hours during constant monitoring.3,4 Hourly averages from the first study3 from 11:00 P.M. to 7:00 A.M. are plotted as a percentage of the maximum (94.9/hr in the period from midnight to 1:00 A.M.). Mean value for 8 subjects and 2-night PSG. Other mV measures are plotted as percent from minimum (0%) to maximum (100%). PLMW is from the first study3; ACT and SBJ are from the second study.4 PLMW is minimum of 13.8/hr (9:00 A.M.), maximum of 91.5/hr (2:00). ACT is minimum of 124.9 counts (12:00), maximum of 447.8 (3:00). SBJ is minimum of 2.96 (on 0-to-10 scale averaged over five determinations per 1-hour mSIT) at 9:00 A.M., maximum of 6.04 (at midnight [24:00]). The values of PLMW, ACT, and SBJ were taken by averaging daytime SITs (or mSITs) from the first 2 days of the study; values from hours between 11:00 P.M. and 6:00 A.M. were taken from the third night of total sleep deprivation. There were nine subjects whose measures were averaged in the second study.4
The patients in these two studies were also monitored with rectal thermometers to establish the timing of their internal rhythms. The nadir of this rhythm—which occurs at approximately 4:00 A.M. to 7:00 A.M., shortly before waking in most individuals—is denominated as circadian time 0 or phase 0 degrees.8 The timing of the temperature minimum in these subjects occurred on average between 4:00 A.M. and 5:00 A.M. in clock time, not notably different from normal subjects of the same age. This made a major deficit in the system that regulates circadian phase unlikely. Comparing the temperature cycle to that of RLS features, it was evident that for these patients, RLS severity was greatest during the falling phase of core temperature, and that around the time of temperature nadir, their RLS began to decrease.
Michaud and colleagues9 confirmed the same circadian pattern of RLS severity. They noted—using a similar protocol and repeated episodes of constrained rest—that even normal subjects seemed to show a pattern of discomfort and movement that paralleled that of RLS patients, although to a considerably lesser degree. This observation echoes the finding that pain perception, too, is most intense during nighttime hours.10 In addition to level of discomfort, the rapidity with which symptoms develop shows the same circadian pattern in RLS patients: when symptoms peak, they develop more rapidly.11
These studies have indicated that RLS does have a true circadian rhythm, and that RLS is most severe before circadian time 0 (core temperature nadir). In addition, there is no evidence to date for an abnormality of circadian timing in RLS and even normal persons may show a similar rhythm of sensory discomfort and motor activity at rest. These findings have led to the questions of how RLS symptoms are related to the circadian mechanism and which features of downstream (circadian output) control are disordered in RLS.
It has been noted that both iron and dopamine (see Chapters 9, 10, and 11), potential mediators of RLS, have a circadian rhythm in which circulating levels are lowest during the evening and night-time hours when RLS symptoms are most intense.
Endocrine Markers of Circadian Phase in Restless Legs Syndrome
Potential abnormalities of circadian function have also been evaluated by means of investigation of the endocrine function across the 24-hour cycle. It is known that the pattern of secretion of many hormones across the day and night follows a circadian pattern.12 Furthermore, the effects of neuroendocrine secretion on sleep and, conversely, of sleep deprivation on endocrine secretion have also long been established.12 Thus, it can be expected that the circadian pattern of secretion of certain hormones, particularly of those that are markers of circadian rhythms or are directly influenced by dopaminergic mechanisms, might be altered in RLS. We briefly outline in the following paragraphs the circadian patterns of secretion of several hormones in RLS, both in the untreated and treated conditions as well as after treatment.
Melatonin and Restless Legs Syndrome
As the main marker of the circadian phase, the role of melatonin in RLS has been studied by investigators. Tribl and colleagues13 analyzed the urinary excretion of 6-OH melatonin-sulfate both during the daytime (7:00 A.M. to 10:00 P.M.) and the nighttime (10:00 P.M. to 7:00 A.M.) in 15 patients with idiopathic RLS and 11 control subjects by means of radioimmunoassay. For both groups, nighttime excretion was greater than daytime excretion. However, no difference between patients and control subjects could be found either in the daytime or in the nighttime. This study had major limitations, because of the poor time resolution achieved by urinary metabolites.
Michaud and colleagues9 investigated the circadian pattern of salivary melatonin in a study that involved seven patients with RLS and seven age- and gender-matched healthy control subjects. The experimental protocol consisted of an all-night sleep study followed by a 28-hour modified constant routine procedure.9 Because it was not possible to keep RLS patients in bed for 28 consecutive hours, the constant routine protocol was divided into 14 episodes of 2 hours. During the first 20 minutes, subjects had to first evaluate their subjective vigilance and provide a salivary sample before they were free to walk around (free-moving period). Afterward, they were confined to a reclining chair for 40 minutes, followed by another 20-minute free-moving period, and then by a 40-minute suggested immobilization test (SIT).5 As described previously by the same group,14 during the SIT, subjects were reclined at a 45-degree angle with their legs outstretched and were instructed to avoid voluntary movements for the duration of the test and to quantify their level of leg discomfort every 5 minutes on a visual analog scale. The SIT was performed under dim light condition. A significant circadian variation in leg discomfort and PLM was found for both groups. However, no differences were seen in the circadian rhythm of melatonin between patients and control subjects, although the profiles of leg discomfort and PLM were significantly correlated with those of subjective vigilance, core body temperature, and salivary melatonin (Fig. 13-2





