Chapter 704 Biologic and Chemical Terrorism
Epidemiology and Pediatric-Specific Concerns
Large-scale attacks on civilian targets will likely involve pediatric victims, and children may be more susceptible than adults to the effects of certain biologic and chemical agents (Chapters 699 and 700). Thinner skin makes dermally active chemical agents, such as mustard, a greater risk to children than adults. A larger surface area per unit volume further increases the problem. A small relative blood volume makes children more susceptible to the volume losses associated with enteric infections such as cholera and to gastrointestinal intoxications such as might be seen with exposure to the staphylococcal enterotoxins. Children’s relatively higher minute ventilation than that of adults increases the threat of agents delivered via the inhalational route. The fact that children live “closer to the ground” compounds this effect when heavier-than-air chemicals are involved. An immature blood-brain barrier may heighten the risk of central nervous system toxicity from nerve agents. Finally, developmental considerations make it less likely that a child would readily flee an area of danger, thereby increasing exposure to these various adverse effects.
Children also may experience unique disease manifestations not seen in adults; suppurative parotitis is a common characteristic occur among children with melioidosis but is not generally seen in adults with Burkholderia pseudomallei infection (Chapter 197.2).
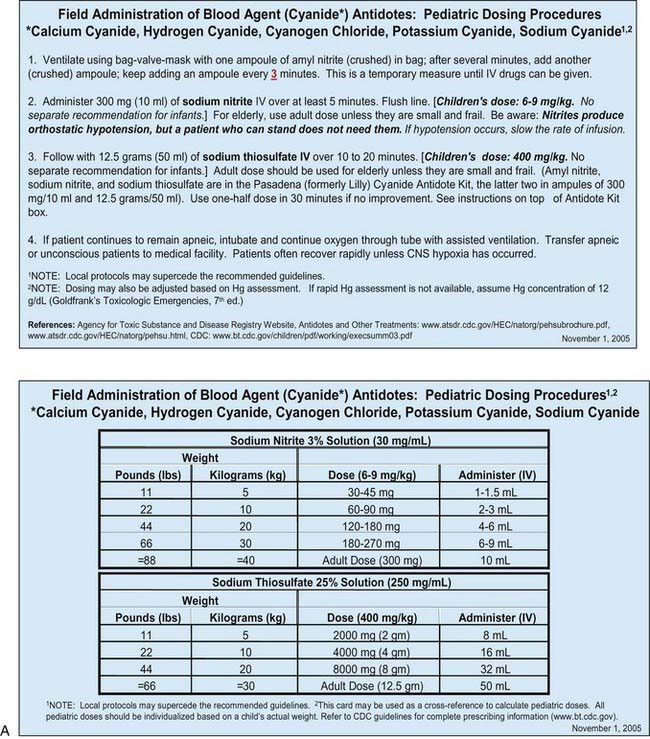
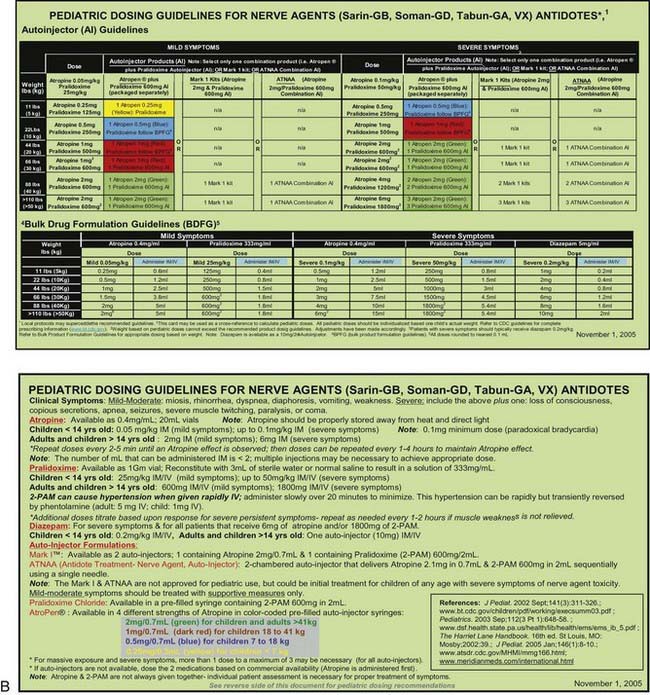
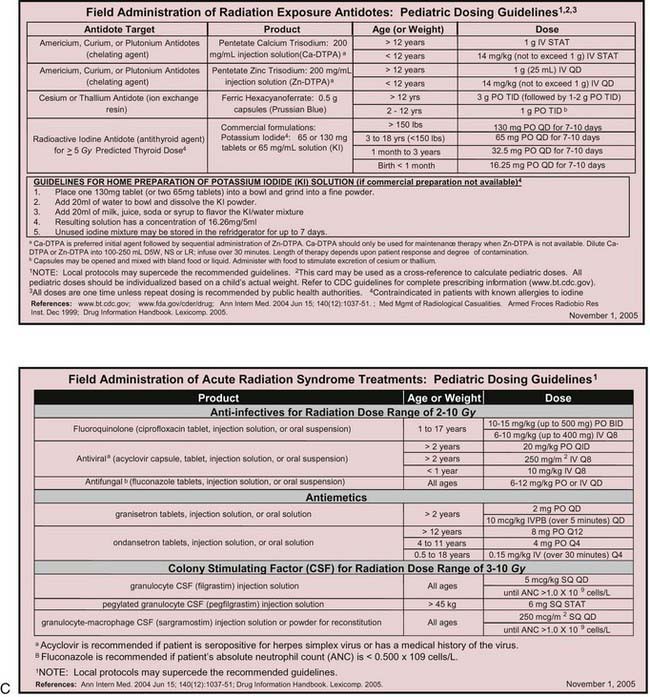
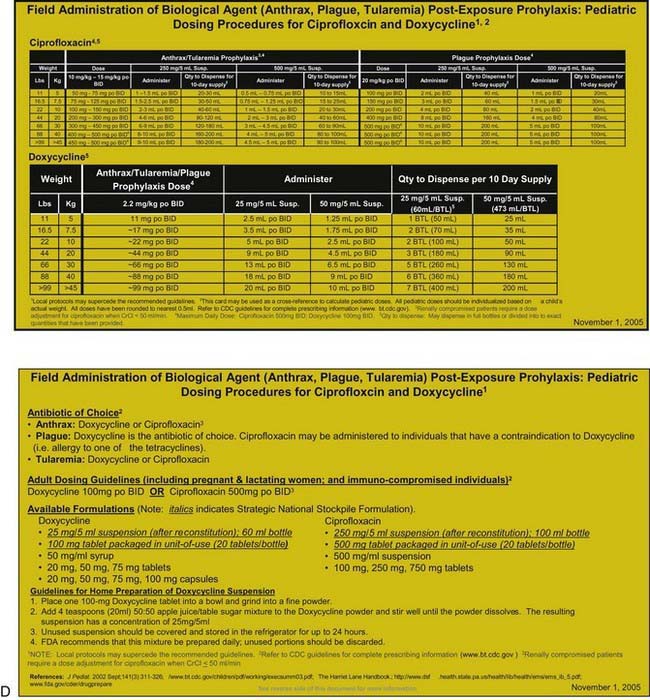
Many otherwise useful pharmaceutical agents are not available in pediatric dosing regimens. The military distributes nerve agent antidote kits consisting of prefilled autoinjectors designed for the rapid administration of atropine and pralidoxime. Many emergency departments and some ambulances stock these kits. The doses of agents contained in the nerve agent antidote kit are calculated for soldiers and thus are far in excess of those appropriate for young children, and pediatric pralidoxime autoinjectors are not yet available. Atropine autoinjectors specifically formulated for children have been approved by the FDA and are now widely available. To facilitate accurate field post-exposure dose administration for children based on age, weight, and level of exposure, the U.S. Public Health Service has prepared four pocket-sized “Weapons of Mass Destruction Pediatric Dosing Cards” for biologic agents, nerve agents, cyanide, and radiation (Fig. 704-1).
Clinical Manifestations
In the event of a terrorist attack, clinicians may be called on to make prompt diagnoses and render rapid life-saving treatments before the results of confirmatory diagnostic tests are available. Although each potential agent of terrorism produces its own unique clinical manifestations, it is useful to consider their effects in terms of a limited number of distinct clinical syndromes. This approach helps clinicians make prompt, rational decisions regarding empirical therapy. In general, casualties from a terrorist attack experience symptoms immediately upon exposure to an agent (or within the first several hours after exposure) or, alternatively, symptoms develop slowly over a period of days to weeks. In the former case, the sinister nature of the event is often obvious, and the etiology more likely to be conventional or chemical in nature. Biologic agents differ from conventional, chemical, and nuclear weapons (Chapters 699 and 700) in that they have inherent incubation periods. Patients are therefore likely to present removed in time and place from the point of an unannounced and unnoticed exposure to a biologic agent. Whereas traditional first responders such as firemen and paramedics may be at the forefront of a conventional or chemical terrorism response, the primary care physician is likely to constitute the first line of defense against the effects of a biologic agent.
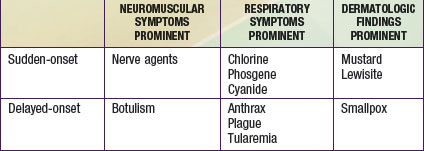
Casualties can thus be categorized as either immediate or delayed in presentation. Within each of these categories, patients can be further classified as having primarily respiratory, neuromuscular, or dermatologic manifestations (Table 704-1). A limited number of agents may cause each particular syndrome, permitting institution of empiric therapy targeted at a short list of potential etiologies. The viral hemorrhagic fevers might manifest as fever and a bleeding diathesis; these agents are considered separately in Chapter 263. In most cases, supportive care is the mainstay of hemorrhagic fever treatment.
Sudden-Onset Neuromuscular Syndrome: Nerve Agents
The very rapid onset of neuromuscular symptoms after an exposure should lead the clinician to consider nerve agent intoxication. The nerve agents (tabun, sarin, soman, and VX) are organophosphate analogues of common pesticides that act as potent inhibitors of the enzyme acetylcholinesterase. They are hazardous via ingestion, inhalation, or cutaneous absorption (Chapter 58).
Delayed-Onset Neuromuscular Syndrome: Botulism
The delayed onset (hours to days after exposure) of neuromuscular symptoms is characteristic of botulism. Botulism occurs after exposure to one of seven related neurotoxins produced by certain strains of Clostridium botulinum, a strictly anaerobic, spore-forming, gram-positive bacillus commonly found in soil. Naturally occurring botulism (Chapter 202) usually follows ingestion of preformed toxin (food poisoning) or results from intestinal toxin production (infantile botulism). An aerosol exposure would likely result in a case of clinical botulism indistinguishable from that caused by natural exposures.
Sudden-Onset Respiratory Syndrome: Chlorine, Phosgene, and Cyanide
Cyanide is a cellular poison, with protean clinical manifestations. Initially, cyanide toxicity is most likely to manifest as tachypnea and hyperpnea, progressing rapidly to apnea in cases with significant exposure (Chapter 58