Chapter 24 Anterior Approaches to the Thoracic Spine and Thoracolumbar Junction
INTRODUCTION
The transthoracic approach to the mid-thoracic level is indicated in cases in which the anterior column is involved with the tumor mass. This approach enables surgeons to accomplish complete ventral decompression of the spinal cord and simultaneous anterior reconstruction.1 Depending on the intactness of the pleura, two kinds of approaches might be taken: transpleural and extrapleural. Patients should possess competent lung function to perform one-lung ventilation. If preoperative evaluation shows a pO2 <60; pCO2 >45; O2 saturation <90%; FVC <1.5 L; FEV1 <1 L; and FEV1/FVC <35%, then the transthoracic approach is contraindicated.2
TRANSTHORACIC APPROACH TO THE MID-THORACIC LEVEL
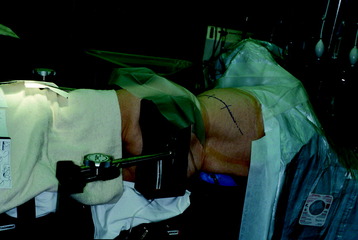
POSITIONING AND INCISION
The operation is performed with the patient in a lateral decubitus position with an axillary roll under the dependent axilla (Fig. 24-1). The patient should be extended with the kidney rest and by tilting the operating table. The side of approach is decided based on the location of the pathology. When possible, a right-sided approach is preferred in the middle and upper thoracic spine because more working space is available over the spinal surface behind the azygos vein compared with that behind the aorta. The left side is preferred for the lower thoracic spine because at this level the liver causes the right diaphragm to rise and partially obstruct the working space. The skin incision starts from four finger breadths lateral to the spinous process, running along the selected rib, and reaches anteriorly to the costochondral junction.
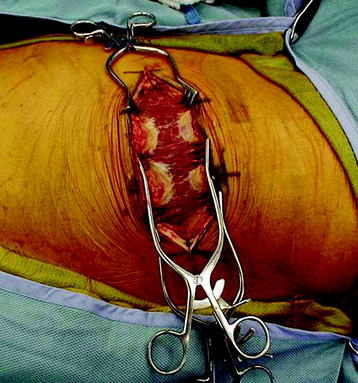
MUSCLE DISSECTION
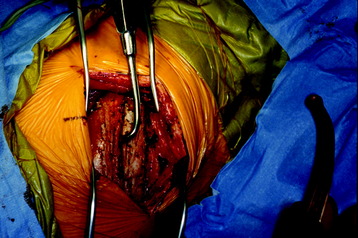
The latissimus dorsi muscle is then divided in a direction transverse to that of the fibers (Fig. 24-2). In the anterior region of the opening, the anterior serratus muscle is exposed. Posteriorly, the trapezius muscle can be exposed. When severing this muscle, the incision line should be as far caudal as possible to save the long thoracic nerve.
After the superficial muscle layer is divided, the second layer of muscles is exposed. According to the level of the lesion, the rhomboids (superiorly), serratus anterior (anterior), and serratus posterior inferior (posterior) can be severed (Fig. 24-3). In cases of the upper thoracic level, mobilization of the scapula is required.
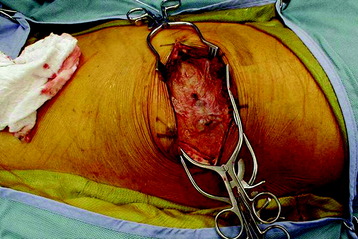
RIB REMOVAL
The outer periosteum of the selected rib is incised sharply and stripped with a periosteal elevator (Fig. 24-4). When preparing the outer and superior surfaces of the rib, a small dissector is used to free the inner periosteum from the underlying pleura. A Doyen elevator is introduced, elevating the inner periosteum anteriorly from the costal junction to the angle of the rib posteriorly (Fig. 24-5). A rib cutter is used to remove the rib. To gain additional exposure of the rib posteriorly, a longitudinal incision is made along the anterior border of the paraspinal muscles, allowing them to be retracted posteriorly past the rib angle.
EXPOSURE OF VERTEBRAL BODY (TRANSPLEURAL)
The thoracic cavity is opened in the bed of the resected rib. The spine is exposed by a longitudinal incision of the pleura 5 mm anterior to the rib heads.2 The lung is retracted anteriorly and the VB is exposed with the parietal pleura covered. Underneath the parietal pleura, the rib head is seen to be in contact with the intervertebral disc. On palpation, the intervertebral disc spaces are prominent, and the segmental vessels generally cross the middle portion of the body.
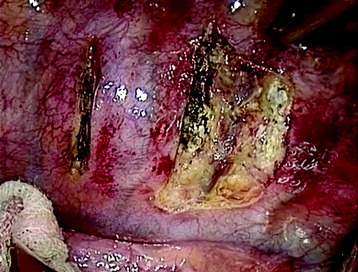
A transverse incision of parietal pleura is made along the rib head and disc space to expose segmental vessels. In cases of a T8 body lesion, dissection starts from adjacent levels (T7 and T9). The parietal pleurae overlying the segmental vessels are swept away with a monopolar coagulator (Fig. 24-6).
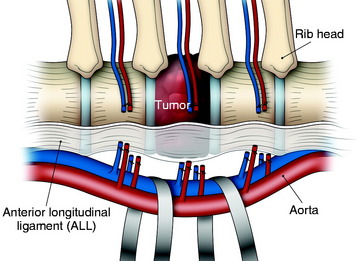
The segmental vessels are coagulated and divided (Fig. 24-7). The segmental vessels are dissected from the underlying VB with a right angle dissector. The hemoclips are applied to two sites, proximal and distal. The proximal side is controlled first, and later the distal side. After the hemoclips are applied to both sides, the vessel is cut and retracted. The sympathetic ganglion is removed to expose the rib head. For further exposure of the anterior portion of the VB, the great vessels should be dissected. The space between the anterior longitudinal ligaments (ALLs) and great vessels is easily created by blunt dissection after the segmental vessels are disconnected. The removal of the rib head is mandatory to gain exposure of the intervertebral foramen and posterior margin of the VB. The rib head is drilled away and the shell is removed with a curette. After rib head removal is completed, the costovertebral joint is exposed.
VERTEBRAL BODY RESECTION
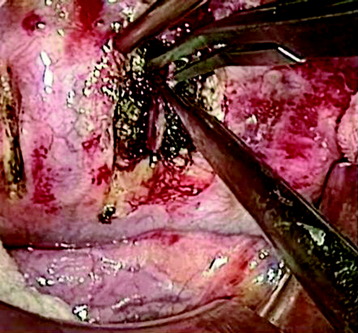
After the parietal pleura is reflected and segmental vessels are controlled, the corpectomy begins. Adjacent disc removal is completed with an osteotome and pituitary forceps. The tumor-infiltrated VB is slightly soft and friable. The resection boundary is confined with an osteotome, and internal debulking is performed with pituitary forceps (Fig. 24-8). For exposure of the ventral surface of the spinal cord, the posterior cortical shell of the VB should be removed. When the posterior cortex is removed, great care should be taken not to injure the spinal cord.
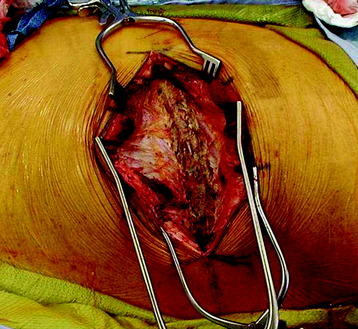
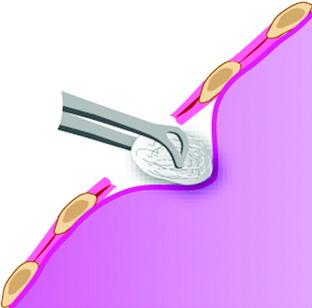
EXPOSURE OF THE VERTEBRAL BODY (EXTRAPLEURAL)
When a patient’s pulmonary function is not sustainable for one-lung ventilation, an extrapleural approach can be considered. Although this approach provides limited exposure compared with the transpleural approach, one advantage is that it can be performed with lung retraction without lung collapse. After rib removal, the endothoracic fascia is incised. The parietal pleura is kept intact. The dissection is performed between the endothoracic fascia and the parietal pleura (Fig. 24-9). This dissection provides the way to the VB (Fig. 24-10).
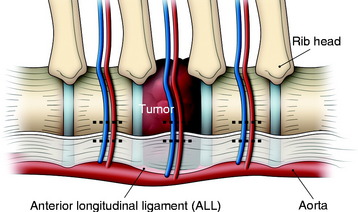
BILATERAL SEGMENTAL VESSEL LIGATION
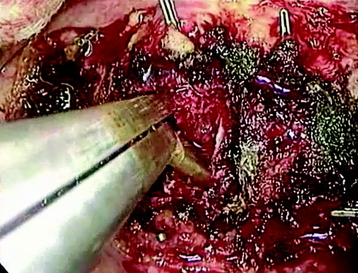
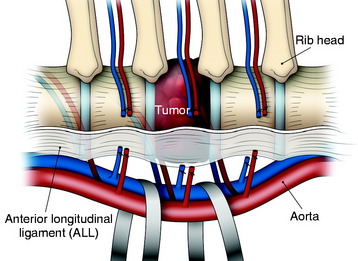
In the thoracic region, parietal pleural incisions are made on each VB level and corresponding rib head. After the dissection of the parietal pleura, the segmental vessels are seen on the midpoint of the VBs. First, the segmental vessels on the approach side are ligated (Fig. 24-11). Great care should be taken to dissect the vessel from the tumor-infiltrated cortical surface. After vessel ligation, the interface between the aorta and VB anterior surface is dissected. With traction applied to the proximal portion of the ligated segmental vessels, great vessels are moved to the anterior side to form potential space with reference to the ALL (Fig. 24-12).
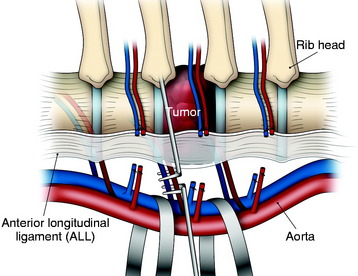
An adhesion may exist between the tumor-infiltrated VB and the great vessels. However, the dissection is relatively easy because the ALL blocks ventral expansion of the tumor mass. When the great vessels are moved forward, the segmental vessels on the contralateral side are seen to wind the lateral surface of the VBs. The exposed field is very deep. A surgical instrument such as the right angle dissector is applied to the contralateral segmental vessels, which are cut and tied (Figs. 24-13 and 24-14). Great care should be taken not to stretch these vessels. Neurological deficit after unilateral left-sided ligation of the T10–12 segmental vessels occurs in 0.75% of patients.3,4 There would appear to be virtually no risk to segmental vessel ligation provided the following: (1) vessel ligation is unilateral, (2) ligation is performed on the convexity of a scoliosis, (3) vessels are ligated at the mid-VB level, and (4) hypotensive anesthesia is avoided.