CHAPTER 75
Peroneal Neuropathy
Definition
Peroneal neuropathy, the most common entrapment neuropathy of the lower extremity [1], is compromise of any portion of the peroneal nerve. This can be from its origins within the sciatic nerve, in which it remains distinct from the tibial portion, throughout the course of the sciatic nerve, to its terminations in the leg and foot. The common peroneal nerve completely separates from the tibial nerve in the upper popliteal fossa and then traverses laterally to curve superficially around the fibular head. Before the fibular head, the lateral cutaneous nerve of the calf branches off to supply cutaneous sensation to the upper lateral leg. Near the fibular head, the common peroneal nerve bifurcates into the superficial peroneal nerve and deep peroneal nerve, which describes their relative locations as they wrap around the fibular head. Because the deep portion is immediately adjacent to the hard bony surface, it is more susceptible to compression injuries at the fibular head, which is the most common site of peroneal nerve compromise [2,3].
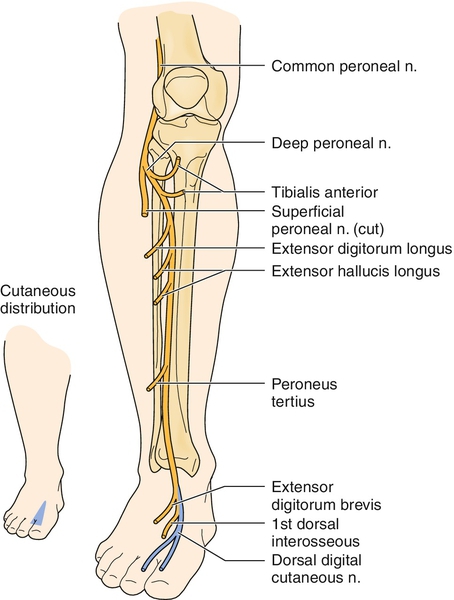
The common peroneal nerve provides the lateral cutaneous nerve of the calf and the motor branch to the short head of the biceps femoris above the fibular head. The superficial peroneal nerve is predominantly sensory, providing cutaneous sensation to the lateral lower leg and most of the foot dorsum. The superficial peroneal nerve also innervates the foot evertors, peroneus longus and brevis. The deep peroneal nerve is predominantly motor, innervating the foot and toe dorsiflexors, but it has a small cutaneous representation at the dorsal first web space of the foot.
Predisposing factors for peroneal mononeuropathy at the fibular head, the most common site of compromise, include weight loss [2,4–7], diabetes [2,8], peripheral polyneuropathy [2], and positioning and localized prolonged pressure [9], such as habitual leg crossing [1] or prolonged squatting [2,10]. A history of such sustained pressure should be elicited.
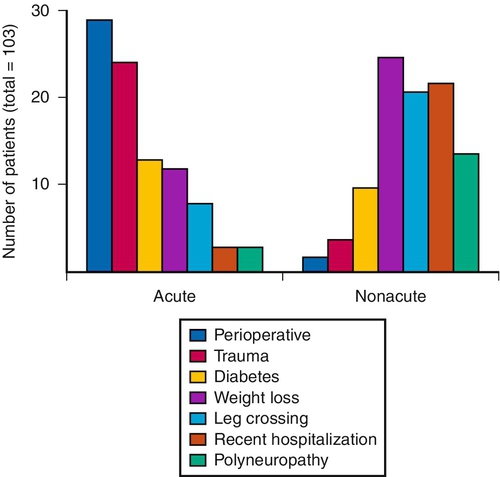
Figure 75.1 shows the most common causes of acute and nonacute lesions. Iatrogenic causes should be considered. These include anesthesia for surgery, leading to immobility and possible positioning issues [9,11,12]; surgery about the hip [13–15], knee [16], or ankle [17]; prolonged imposed bed rest with decreased sensorium due to sepsis or coma [2,18]; intermittent sequential pneumatic compression [19]; acupuncture [20]; and plaster casts [2], braces, sports icing and compression wraps [21], and, ironically, ankle-foot orthoses [5,22]. A history of severe inversion ankle sprain or blunt trauma to the ankle, leg, or fibular head can be helpful in identifying likely pathophysiologic mechanisms.
Stretch injury commonly occurs at the hip region and may be associated with hip surgery (e.g., total hip arthroplasty, especially if the limb is lengthened) [13] or traumatic hip dislocation. The peroneal portion of the sciatic nerve is more susceptible to stretch injuries than the tibial portion because of its lateral position and the shorter distance between the piriformis and the fibular head than between the piriformis and the tarsal tunnel (e.g., the sites of relative fixation of these two nerves). Distal peroneal nerve stretch injury can also occur at the point where it passes through the peroneus longus muscle. In addition, peroneal nerve injury is proposed to occur after stroke by equinovarus footdrop posturing [23].
Symptoms
Peroneal neuropathy typically is manifested with acute footdrop, but this can sometimes occur insidiously during several days to weeks. The footdrop can be complete or partial, often with increased tripping or falls as the primary complaint. Numbness or dysesthesias frequently occur in the lower lateral leg and dorsum of the foot, although pain is uncommon. When pain is present, it is usually located around the knee and felt as deep and ill-defined [2]. When pain is prominent and neuropathic in character, stretch injury of the peroneal portion of the sciatic nerve should be considered.
Physical Examination
The examination should be guided by a close understanding of the relevant anatomy, with focused study of the elements of each component of the peroneal nerve.
Sensory deficits in the upper lateral leg (Fig. 75.2) suggest a lesion proximal to the fibular head. Testing of foot inversion, to rule out concomitant tibial nerve compromise and therefore sciatic nerve as the likely site of injury, must be performed with the foot passively slightly dorsiflexed for optimal strength testing (often the foot will initially, at rest, be in a plantar flexed position during examination as a result of the existing footdrop) because inversion is normally weak when the foot is relatively plantar flexed [1]. With the long head of the biceps femoris intact, knee flexion strength will test normal despite a compromise to the short head of the biceps femoris strength. Palpation may reveal a lack of tissue tensing where the short head of the biceps femoris should be located. This is, however, challenging to discern and helpful only in the case of acute complete proximal peroneal nerve compromise with relative sparing of the tibial-innervated hamstring muscles. The function and innervation of the long and short heads of the biceps femoris can be more accurately determined electrodiagnostically. If both are compromised, knee flexion will be weak, as will plantar flexion and toe flexion, suggesting a sciatic nerve lesion. Hip abduction strength testing has been found helpful in distinguishing peroneal neuropathy from L5 radiculopathy in patients with footdrop [24]. Muscle stretch reflexes will usually be normal unless the sciatic nerve is severely compromised, when the medial hamstring and Achilles reflexes could be reduced or absent.
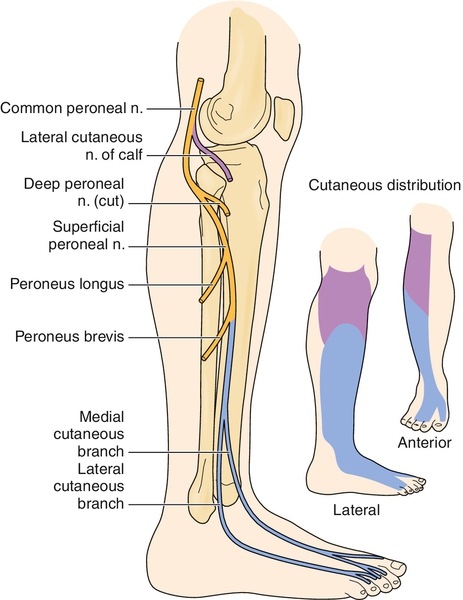
Sensory deficit or dysesthesia in the lower lateral leg and over most of the dorsum of the foot suggests involvement of the superficial peroneal or this portion of the sciatic nerve (see Fig. 75.2). Eversion weakness is consistent with superficial peroneal nerve compromise. If the superficial peroneal nerve lesion is isolated, then Achilles, quadriceps, and medial hamstring muscle stretch reflexes will be normal.
If eversion is strong but dorsiflexion is very weak, a more focal deep peroneal nerve compromise is suggested. There may be sensory deficits or dysesthesias along the isolated area of the dorsum of the first web space of the foot on the affected side (Fig. 75.3). A combination of deep and superficial peroneal nerve branch compromise often occurs, usually affecting the deep branch more severely than the superficial branch, especially with lesions at the fibular head.